Publication
Research Article
International Journal of MS Care
The Multiple Sclerosis Self-Management Scale–Revised (MSSM-R)
Author(s):
Abstract
Background:
Self-management is the most important component in the treatment of chronic diseases, including multiple sclerosis (MS). The Bishop and Frain Multiple Sclerosis Self-Management Scale–Revised (MSSM-R) is one of the valid tools available for self-management assessment. The purpose of this study was to evaluate the psychometric properties of the MSSM-R in Iranian people with MS.
Methods:
This cross-sectional study was conducted in 2018 in the 1600 people with MS in Guilan Province, Iran. In this study, 250 people were selected by convenience sampling. The reliability of the Persian version of this scale was examined by internal consistency and test-retest methods, and validity evidence was evaluated using confirmatory factor analysis.
Results:
The MSSM-R had acceptable face and content validity. Confirmatory factor analysis results showed that 24 items on this scale have factor loadings in five subscales. Other results showed the internal consistency, as measured by Cronbach α and test-retest reliability, for the MSSM-R overall (α = 0.85, r = 0.77) and for the following subscales: Healthcare Provider Relationship and Communication (α = 0.83, r = 0.70), Treatment Adherence/Barriers (α = 0.70, r = 0.71), Social/Family Support (α = 0.79, r = 0.85), MS Knowledge and Information (α = 0.89, r = 0.72), and Health Maintenance Behavior (α = 0.77, r = 0.75).
Conclusions:
This study provides evidence of the validity and reliability of the MSSM-R. To further ensure its psychometric properties, additional studies with this scale are suggested.
Multiple sclerosis (MS) is a debilitating central nervous system disorder that is progressive and chronic, usually beginning at age 20 to 40 years.1 According to valid reports, MS is the second leading cause of nontraumatic disability in young people.2 Multiple sclerosis is more common in women around the world,3 and this difference is reported to be 1.8 to 3.6.1 Various studies suggest that in recent years the spread of MS has grown vastly in Iranian cities. It has been reported that the estimated incidence of this disease in Tehran (the most populous city) is 52 in 100,000.4 In a study conducted in southeastern Iran, the prevalence of MS in 2010 was 13.96 and 2.67 in 100,000 for women and men, respectively.5 A 2018 study reported rates of MS per 100,000, by province, as 93.6 in Isfahan, 92.7 in Charmahal and Bakhtiari, 77.3 in Fars, 74.3 in Tehran, 50.4 in Qom, 35.9 in Guilan, 33.7 in Zanjan, and 18.0 in Golestan.6 In total, studies have found that Iran is no longer at moderate prevalence and is now becoming an area with a high prevalence of disease.4
There is currently no definite treatment for MS, and the options include living with a lifelong illness and symptom management, which is recognized as an essential component in the care of the disease.7 Self-management in chronic diseases is one of the main components of active participation in treatment.8
Self-management is defined as an active process for coping with disease through adherence to treatment and drug use, participation in medical decision making, self-care, and maintenance of social relationships and emotional balance.9 Also, in other definitions, self-management is described as learning and participating in the necessary skills to continue an active life and a satisfying psychological status in the face of a chronic disease.10 Self-management in chronic diseases is associated with improved quality of life9 and decreased symptoms and treatment costs.11 12 Other studies suggest that self-management is related to a wide range of positive outcomes in the field of health and rehabilitation,9 including increased self-control against disease symptoms13 and decreased hospitalization,14 pain, and anxiety.15 Self-management strategies help maintain and promote health and reduce the adverse outcomes of the disease using mechanisms such as having a better understanding of the disease, acquiring the necessary knowledge, adhering to appropriate diet and nutrition, and increasing knowledge and development of patient skills.16
Although previous studies have pointed to the importance of self-management in patients with chronic disease and have introduced it as an important aspect in chronic disease management, few studies have been conducted in the field of self-management of people with MS.9 Today, for the purpose of conducting self-management studies and reviews in people with MS, the need for credible and reliable assessments has become increasingly evident. To this end, the Multiple Sclerosis Self-Management Scale (MSSM) was created in 2007 for the comprehensive assessment of the knowledge and self-management behavior of adults with MS.17 Then it was assessed in 2011.7 In the latest study in 2014, the psychometric properties of this tool were reexamined (MSSM-Revised [MSSM-R]).18
Self-management is one of the most important aspects of MS management, but due to the lack of a standard tool, researchers and therapists in Iran have been less interested in this topic. Considering the increasing trend of people with MS in Iran and the need for self-management in clinical and research fields, the existence of a standard tool for professionals and researchers is essential. By self-management assessment, individuals' weaknesses could be identified and effective interventions provided to improve the self-management behaviors of these patients. The aims of this study were to translate the MSSM-R into Persian and to examine the reliability indices of retest, internal consistency, and face validity, as well as the content and structure of the tool, to, in turn, introduce the newest scale in the field of MS self-management to researchers and therapists to be used in clinical and research settings.
Methods
Design and Participants
A cross-sectional design was used for this study, which was conducted in the population with MS in Guilan Province (N = 1600) in 2018. To determine the sample size, the scale was first performed on 25 people, and the mean ± SD score was 72.65 ± 10.90. Then, using G*Power 3.1 software, based on the formula of Chow et al19 the required sample size of 221 people was calculated, which was considered to prevent the possible loss of 250 people.
σ = 10.90, α = 0.05, d = 1.2, 1–β = 0.90. People with MS were selected by convenience sampling through the MS Association of Guilan Province, Guilan University of Medical Sciences (Rasht, Iran), pharmacies, and referrals to health and counseling centers. Sixteen participants in this study were selected for retest reliability. The criteria for their selection were interest and availability after 20 days.
During a 2-month period, the research team gathered data by referring to the mentioned centers. The criteria used for entering this research included conscious satisfaction, diagnosis of MS by neurologists using magnetic resonance imaging and clinical syndrome of the disease for 1 year, and being aged 20 to 50 years. This research has been reviewed and registered with the code IR.GUMS.REC.1397.087 at the Ethics Committee of the Guilan University of Medical Sciences.
Procedures
Written permission was received from the designer of this scale (Dr Malachy Bishop) to translate it into Persian and review its psychometric properties. The MSSM-R was then translated by a psychologist with international English-language proficiency in Persian, and, finally, English and Persian versions were considered in the appropriate selection of words and sentences to match the items by two psychologists and experts in the field of Persian language and literature, and revisions were made to it. The next step was to assess the content validity of the scale for two psychologists, two nurses, and one neurologist (five experts) to report in the content validity index (CVI). Content validity was examined in the following directions: 1) comprehensibility of scale items, 2) accurate assessment of self-management, 3) necessity of each item in the scale, 4) comprehension, and 5) expert opinion on the overall scale in self-management measurement. Experts reviewed the five indicators in five-factor spectra (very low = 0, low = 1, moderate = 2, high = 3, and very high = 4). To obtain the CVI based on the Waltz and Bausell method for each item of the five subscales mentioned, the number of those judging the item as high and very high was divided by the number of content experts (n = 5).20 Structural validity was assessed through first- and second-order confirmatory factor analysis. Face validity was assessed according to expert viewpoint.
Structural questions and first- and second-order confirmatory factor analysis were used to measure the factor structure of the scale. Lisrel software (STATCON GmbH, Witzenhausen, Germany) was used to verify the confirmatory factor analysis. The reliability of this scale was measured using IBM SPSS Statistics for Windows software, version 22.0 (IBM Corp, Armonk, NY) using internal consistency (Cronbach α) and scale stability (retest with 20-day intervals).
Measurement Tool
The MSSM-R has 24 items divided among the following five subscales: Healthcare Provider Relationship and Communication (HPRC) (items 9, 12, 14, 16, 18, 20), Treatment Adherence/Barriers (TA/B) (items 11, 15, 17, 21, 22, 23, 24), Social/Family Support (S/FS) (items 6, 10, 13), MS Knowledge and Information (MSKI) (items 1, 2, 3, 4), and Health Maintenance Behavior (HMB) (items 5, 7, 8, 19). The method of scoring the questionnaire was based on a 5-point Likert scale (1 = completely disagree, 2 = somewhat disagree, 3 = neither agree nor disagree, 4 = somewhat agree, 5 = completely agree); the higher the score, the higher the level of self-management. Note that items 21, 23, and 24 are scored oppositely. Scores range from 24 to 120 in this tool. Exploratory factor analysis revealed that these five subscales explain 57.7% of the total variance of the test. Structural validity results showed that this tool had a negative correlation with the Multiple Sclerosis Impact Scale on physical impact (r = −0.28) and psychological impact (r = −0.24) and a positive and significant correlation with the Multiple Sclerosis Self-Efficacy scale function subscale (r = 0.26) and control subscale (r = 0.31), which indicates the divergent and convergent validity of this tool, respectively. Also, the reliability of this scale was determined by the internal consistency (Cronbach α) for HPRC = 0.85, TA/B = 0.79, S/FS = 0.79, MSKI = 0.71, HMB = 0.59, and MSSM-R = 0.85. The authors of this test reported a score ranging from 59 to 119, with a mean ± SD score of 100.98 ± 11.59.8
Results
In this study, of 250 questionnaires distributed, 220 were answered completely and correctly (12% dropout rate). There were 152 women (69.1%) and 68 men (30.9%). The mean ± SD age of the participants was 35.10 ± 7.36 years. The mean ± SD illness duration was 7.39 ± 4.42 years. Table 1 shows the dispersion measures of the MSSM-R.
Dispersion measures of MSSM-R
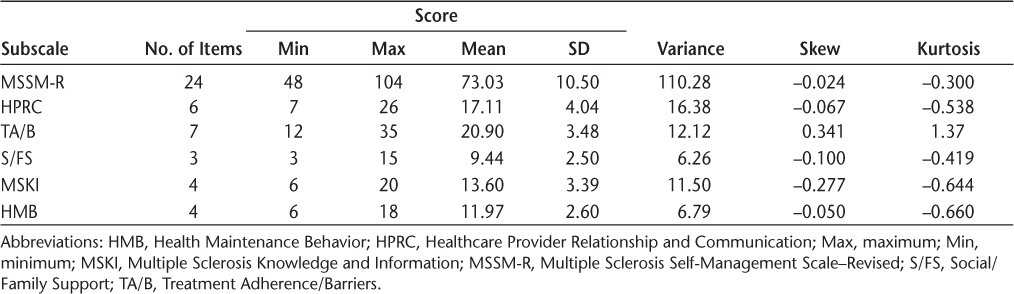
The scores on the overall scale and its five subscales are reported in the dispersion measures table. Given that the standard error of the kurtosis of variables lies within the range of +2 and −2, it can be deduced that the data have a normal distribution. In the following subsections, the psychometric indexes (validity and reliability) of this scale are investigated.
Validity
Face and Content Validity
Face validity was assessed according to expert opinion. The five experts acknowledged that the appearance of the items reflects the whole purpose of the scale. The results of CVI were 0.79 for comprehensibility of scale items; 0.81 for accurate assessment of self-management; 0.86 for necessity of each item in the scale; 0.91 for comprehension; and 1 for expert opinion on the overall scale in self-management measurement.
Structural Validity
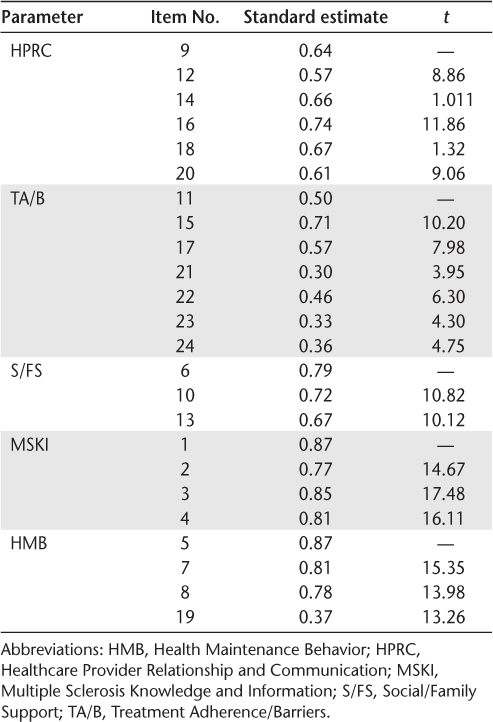
The first-order confirmatory factor analysis was used to investigate the factor load of each item with its own factor and to examine the correlation between scale dimensions, the results of which are reported later herein.
As shown in Table 2, the factor loads of all the items on their own factors are greater than 0.30 in the standard estimation mode. Considering that, in the case of meaningful estimation, t statistics for all items are higher than 1.96, it can be said that all items have a significant factor bearing on their respective factors and are verified. Also, Table 2 shows that items 16, 15, 6, 1, and 5 have the most factor loading and are related to their factors. First-order factor analysis showed that correlation coefficients between self-management scale factors of people with MS were significant and acceptable (t ≥ 1.96), and the factors HPRC and TA/B (0.67) have the highest correlation coefficient and TA/B and MSKI (0.23) have the lowest correlation coefficient.
Standard factor loads of each item with its own factor
Goodness-of-fit index (GFI) results of the first-order factor analysis model showed χ2 = 335.91, χ2 241 = 1.393, root mean square error of approximation (RMSEA) = 0.042, normed fit index (NFI) = 0.91, parsimonious NFI (PNFI) = 0.80, incremental fit index (IFI) = 0.97, comparative fit index (CFI) = 0.97, relative fit index (RFI) = 0.90, and GFI = 0.89. Given that the IFI, NFI, CFI, RFI, and GFI range from 0 to 1, the closer they are to 1, the more favorable the model is. Also, when the PNFI is greater than 0.5, approximate error (RMSEA) is less than 0.08, and χ2 241 is less than 3, it indicates the optimal fit of the model. The fit indexes indicate that the model has an optimal fit, and this scale has structural validity in the Iranian culture.
Findings from the second-order factor analysis show that among the dimensions of self-management, MSKI, HMB, S/FS, TA/B, and HPRC, respectively, have the highest load factors with self-management. In the standard estimation, the factor loads of all factors on self-management are greater than 0.30. Considering that in the case of meaningful estimation, the t statistic for all factors is higher than 1.96, it can be said that all factors have a significant load factor. The GFI results of the second-order factor analysis model showed χ2 = 375.52, χ2 242 = 1.551, RMSEA = 0.050, NFI = 0.90, PNFI = 0.79, IFI = 0.96, CFI = 0.96, RFI = 0.89, and GFI = 0.87. It can be concluded that the model has an optimal fit, and the general structure of the tested relations is confirmed in the second-order factor analysis through the obtained data.
Reliability
The Cronbach α coefficient was calculated in 220 participants, and the test-retest reliability coefficient (r) with a 20-day interval was calculated in 16 people for the subscales of HPRC (α = 0.83, r = 0.70), TA/B (α = 0.70, r = 0.71), S/FS (α = 0.79, r = 0.85), MSKI (α = 89, r = 0.79), and HMB (α = 0.77, r = 0.75) and for the overall MSSM-R (α = 0.85, r = 0.77).
Discussion
The aim of this study was to investigate the psychometric properties of the MSSM-R. The descriptive result showed that the mean ± SD score of this scale in Iranian people with MS was 73.03 ± 10.5; Bishop and Frain reported scores ranging from 59 to 119, with a mean ± SD of 100.98 ±11.59.7 This finding implies that the amount of self-care behavior in Iranian people with MS is lower than that reported by the designers of the MSSM-R. Another study in Iran reported that 51.47% of patients with MS performed self-care behaviors,21 which is very weak. In addition, the participants in the study were those who did not have a long history of illness (mean, 7.39 years); the results suggest that the longer the disease duration, the greater the self-care behaviors in people with type 2 diabetes.22 However, there are no data available in the field of MS. Also, in another study in Iran (Mashhad City), the mean ± SD score of 87.34 ± 13.86 for this scale was calculated for individuals aged 21 to 40 years,23 similar to the present results; therefore, self-management behaviors in patients can be influenced by several factors, such as age and self-management knowledge, and this requires further studies in the future.21
The verification of structural validity by confirmatory factor analysis showed that the 24 items in five subscales were confirmed and all items with factor load were acceptable, and the result is in line with that of the study by the designers of this scale.7 In the present study, the internal consistency for subscales was calculated to be between 0.70 and 0.89, and it was 0.85 for the overall score of the MSSM-R. The designers reported α coefficients for subscales between 0.59 and 0.88, and 0.85 for the overall score of the MSSM-R.7 The overall score of the study is identical to that of the study by the original designers, but the study of subscales shows that the Persian version has better internal consistency and all the subscale scores were calculated to be higher than 0.70. Furthermore, in Mashhad, the internal consistency of this scale was calculated in 291 patients with MS (α = 80), but other psychometric information was not reported in that study.23 In another study, the reliability coefficient was tested by a 2-week test method of 0.83, indicating high reliability of this scale.18
In the present study, the CVI shows that the experts' viewpoint in the field of comprehensibility of the scale for people with MS, accurate assessment of self-management, is less than 0.86, whereas the CVI should be greater than or equal to 0.86 to validate content validation. However, the expert viewpoint about the overall scale in self-management assessment in people with MS receiving a complete score of 1 can attest to the content validity of this scale. One of the main limitations of this study was the lack of consideration of other experts (such as occupational and physical therapists) for the CVI evaluation; taking into account the views of these experts in future studies is suggested for a thorough examination.
In the context of translating the questionnaire from English to other languages, the World Health Organization has made valuable recommendations. In the present study, the recommendations of forward translation and expert panel were considered, but because of the shortness and transparency of the scale, back-translation was not used. Careful examination of the sentences, alternative terms, and common terms in the Persian language were tried in the expert panel. Also, due to the use of expert opinion in determining the face and content validity, no pretesting and cognitive interviewing was used with people with MS.
The participants in this study were younger people with a mean ± SD age of 35.10 ± 7.36 years, and the results of this study cannot be categorically generalized to older people with MS. The mean ± SD disease duration was 7.39 ± 4.42 years; they were either recently affected or were in the early years of the disease.
The selection of 16 people with MS to retest based on their accessibility and their interest in test-retest can reduce the net effect of the retest, especially in this study, which had a short test interval. However, cooperation of many people with MS and the implementation of a retest for a longer interval were not possible. This study was conducted in Guilan Province, but to obtain better results, it must be done in other provinces, especially Isfahan, which has the highest number of people with the disease. In addition, an increase in the number of contributors in the retest reliability and construct validity is suggested for future studies.
In the beginning, people with MS were supposed to be randomly selected from the MS community list, but due to lack of cooperation and lack of access to them in dispersed areas of the province, convenience sampling was used, which makes it difficult to generalize the results. Despite all of the limitations, the researchers hope that this study will be the starting point for future studies to complete the psychometric properties of the scale and for it to be used directly in clinical studies and interventions.
In conclusion, the results of this study provide evidence of the validity and reliability of the self-management scale of people with MS in an Iranian sample. Note that more studies need to be performed in the field of psychometric scales before extensive use of this tool in clinical and research situations. However, this tool has the ability to fill the vacuum of self-management measurement in people with MS, and this study can be extended with more research and other psychometric methods, such as construct validity
PRACTICE POINTS
Recent epidemiological studies suggest that the prevalence of MS is high in Iran.
Self-management is an important aspect of coping with MS. The Multiple Sclerosis Self-Management Scale–Revised (MSSM-R) was developed to assess knowledge and behavior related to self-management.
This study provides evidence of the validity and reliability of the Iranian version of the MSSM-R.
Acknowledgments
This research is based on Mr Saadat's final PhD thesis in Psychology at the University of Isfahan. We thank the people with MS in Guilan Province, the Multiple Sclerosis Society of Guilan, and the Clinical Research Development Unit Poursina. Special thanks to Dr Malachy Bishop, designer of the MSSM-R, who allowed us to translate and use this questionnaire.
References
Khodaveisi M, Ashtarani F, Beikmoradi A, et al. The effect of continuous care on the lifestyle of patients with multiple sclerosis: a randomized clinical trial. Iran J Nurs Midwifery Res. 2017;22:225–231.
Eftekharian MM, Mousavi M, Hormoz MB, Roshanaei G, Mazdeh M. Multiple sclerosis and immunological-related risk factors: results from a case-control study. Hum Antibodies. 2014;23:31–36.
Harbo HF, Gold R, Tintoré M. Sex and gender issues in multiple sclerosis. Ther Adv Neurol Disord. 2013;6:237–248.
Sahraian MA, Khorramnia S, Ebrahim MM, Moinfar Z, Lotfi J, Pakdaman H. Multiple sclerosis in Iran: a demographic study of 8,000 patients and changes over time. Eur Neurol. 2010;64:331–336.
Moghtaderi A, Rakhshanizadeh F, Shahraki-Ibrahimi S. Incidence and prevalence of multiple sclerosis in southeastern Iran. Clin Neurol Neurosurg. 2013;115:304–308.
Sahebi R, Amiri M, Jami MS. Multiple sclerosis in Iran. Int J Epidemiol Res. 2018;5:30–33.
Bishop M, Frain MP. The Multiple Sclerosis Self-Management Scale: revision and psychometric analysis. Rehabil Psychol. 2011;56:150–159.
Wilski M, Tasiemski T, Kocur P. Demographic, socioeconomic and clinical correlates of self-management in multiple sclerosis. Disabil Rehabil. 2015;37:1970–1975.
Bishop M, Frain MP, Tschopp MK. Self-management, perceived control, and subjective quality of life in multiple sclerosis: an exploratory study. Rehabil Couns Bull. 2008;52:45–56.
Lorig K. Self-management of chronic illness: a model for the future. Generations. 1993;17:11–14.
Holman H, Lorig K. Patient self-management: a key to effectiveness and efficiency in care of chronic disease. Public Health Rep. 2004;119:239–243.
Johnson KL, Kuehn CM, Yorkston KM, Kraft GH, Klasner E, Amtmann D. Patient perspectives on disease-modifying therapy in multiple sclerosis. Int J MS Care. 2006;8:11–18.
Jordan JE, Osborne RH. Chronic disease self-management education programs: challenges ahead. Med J Aust. 2007;186:84–87.
Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self-management of chronic disease in primary care. JAMA. 2002;288(:2469–2475.
Lorig KR, Holman HR. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med. 2003;26:1–7.
Newman S, Steed L, Mulligan K. Self-management interventions for chronic illness. Lancet. 2004;364:1523–1537.
Bishop M, Frain M. Development and initial analysis of Multiple Sclerosis Self-Management Scale. Int J MS Care. 2007;9:35–42.
Ghahari S, Khoshbin LS, Forwell SJ. The Multiple Sclerosis Self-Management Scale: clinometric testing. Int J MS Care. 2014;16:61–67.
Chow S, Shao J, Wang H. Sample Size Calculations in Clinical Research. 2nd ed. Chapman & Hall/CRC Biostatistics Series; 2008.
Waltz C, Bausell BR. Nursing Research: Design Statistics and Computer Analysis. FA Davis; 1981.
MorowatiSharifabad M, Momeni Z, Eslami M, DehghaniTafti A, Hakimzadeh A. Study of factors associated with self-care behaviors in patients with multiple sclerosis in Yazd City based on Health Belief Model. J Toloo-e-behdasht. 2016;15:82–93.
Bigdeli MA, Hashemi Nazari SS, Khodakarim S, Brodati H, Mafi H. Factors associated with self-care behavior in patients with type II diabetes. J Mazandaran Univ Med Sci. 2015;25:61–72.
Zarei B, Vagharseyyedin SA, Gorganie E. Relationship between spiritual well-being and self-management among Iranian people with multiple sclerosis. Jundi J Chron Dis Car. 2015;4:18–24.







