Publication
Research Article
International Journal of MS Care
Changes in Activity Participation After Multiple Sclerosis Diagnosis
Author(s):
Abstract
Background:
Multiple sclerosis (MS) results in impairments in cognitive and motor skills, which may reduce the level of activity participation in people with MS. This study compares past and current levels of activity participation in adults with MS and controls. The relationship between retained activity participation (since diagnosis) and cognitive, motor, functional status, and depression symptoms of persons with MS was examined.
Methods:
Twenty-seven individuals with MS living in the community and 21 controls completed cognitive and motor tests and rated their activity participation (using the Activity Card Sort), depression symptoms, and functional status.
Results:
The MS group reported significantly lower current activity participation than the control group. Percentage of retained activity participation (from prediagnosis to current) in the MS group correlated with time since diagnosis, executive function and motor skill ability, depression symptoms, and current functional status.
Conclusions:
Persons with MS report negative changes in activity participation in most aspects of life after diagnosis. These findings call attention to changes in activity participation in people with MS that are directly related to disease symptoms. Therefore, using a quantitative measure of activity participation—the Activity Card Sort—can provide important information to aid the clinician in developing individualized treatment goals for people with MS.
Multiple sclerosis (MS) is a progressive neurologic disease that affects the central nervous system with a highly variable and unpredictable clinical course. Common physical impairments caused by MS include reduced balance and coordination, muscle weakness, spasticity, increased gait variability, and decreased walking speed.1 2 Cognitive impairment occurs in 43% to 70% of people diagnosed as having MS.2 3 Affective symptoms are also prevalent in persons with MS, with a lifetime prevalence of approximately 50% and an annual prevalence of 20%.4 5 Therefore, persons with MS are faced with the daily management of multiple impairments related to daily life activity participation.6 7 For example, Basak et al8 examined performance of activities of daily living (ADLs) and self-care in persons with MS 10 years or more after diagnosis. They found that 79.1% of the sample participants were mildly dependent on various types of assistance (eg, cutting food, use of a wheelchair) to perform ADLs as indicated by the Barthel Index, a measure of performance in ADLs. These participants were also moderately dependent on assistance to perform self-care activities based on the Exercise of Self-Care Agency Scale.9 In addition, participants with a longer disease duration experienced more activity limitations compared with participants with a shorter disease duration. Karhula et al10 asked 113 persons with MS to describe problems in everyday activity participation. The most common difficulties that this sample identified were limitations in the areas of recreation and leisure. Other limitations included problems related to domestic life and moving around.
Most research on the daily functions of persons with MS connects activity participation with cognitive and motor functions and depression symptoms.11 12 For example, Vanner et al11 found that higher levels of physical and leisure/recreation activity were associated with lower levels of apathy and depression and higher levels of cognition, self-efficacy, and physical and mental quality of life. Taking a qualitative perspective, Newitt et al13 found that 44 participants with MS (along with 155 participants with various neurologic conditions, such as spinal cord injury, Parkinson disease, and stroke) reported that the most common barriers to participation in various activities were lack of walking, poor balance, muscle weakness, pain, stiffness, bladder and bowel problems, depression, issues with thermoregulation, and fear of injury. In sum, individuals with MS present with a complex symptom profile that is associated with limitations in activity participation. The way symptoms influence activity participation is unique to the individual. Therefore, it is necessary to understand how specific symptoms are associated with activity participation to adopt client-centered approaches when designing interventions.
Most measurements of everyday life activity participation do not capture the changes that a person with MS experiences specifically due to MS-related symptoms. This is likely because most assessments focus only on how a participant performs at the time of the assessment and do not capture a person's degree of activity participation before diagnosis. Without this information, it is difficult to determine whether an individual reporting limited current activity participation in leisure activity has always been less active or whether the reduced activity participation is due to MS. This is a critical distinction that could have a profound effect on a patient's perception of whether their reported levels of activity participation are problematic. Researchers and practitioners understanding the degree to which activity participation changes after diagnosis is important because this information can direct a client-centered approach to rehabilitation. This study evaluated changes in activity participation after MS diagnosis and examined whether these changes relate to disease symptoms.
To determine the degree of change in activity participation after the diagnosis of MS, this study compares levels of past and present activity participation in persons with MS and control participants. An additional aim was to investigate the relationship between retained activity participation (the difference between past activity participation and current activity participation) and cognition, motor skills, and depression symptoms in people with MS. It was hypothesized that 1) participants with MS would have lower levels of current activity participation compared with control participants and compared with their previous level of activity and 2) the lower levels of engagement in current activity participation compared with past activity participation in persons with MS would be associated with decreased cognitive and motor ability and with more depression symptoms.
Methods
Participants
Twenty-seven individuals with clinically definite MS14 who live in the community and 21 controls were included in this study. Potential participants with MS contacted the research coordinator by responding to an advertisement for the study at local support groups and clinics in New Jersey and the New York metropolitan area. Controls were recruited via advertisements in the local community. Potential participants were aged 18 to 65 years and were able to understand and write English at a sixth-grade level, as determined by the Wide Range Achievement Test–Revised (Wilkinson GS and Robertson GJ, 2006). They also had adequate vision to read the study materials, their most recent exacerbation was at least 1 month earlier, and they were not taking corticosteroids. Potential participants who had a history of neurologic disease (aside from MS), alcohol or drug abuse, or major psychiatric disturbance were excluded. During initial phone contact, potential participants were screened using these inclusion/exclusion criteria, and qualified participants were scheduled for testing. Before study enrollment, all the participants signed a consent form approved by the institutional review board and the Health Insurance Portability and Accountability Act compliance board of Kessler Foundation (East Hanover, NJ) indicating willingness to participate in the study.
Measures
Activity Participation in MS and Control Groups
The Activity Card Sort (ACS)15 was designed to assess perceived amount of participation. The ACS is an interview-based assessment composed of 82 cards depicting activities. The pictorial cards are categorized into subgroups of high-demand (eg, exercising) and low-demand (eg, bird watching) leisure activities, social/educational activities (eg, family gatherings), and household activities (eg, doing laundry). Participants with MS were instructed to think about their current participation in the various activities and their participation before they were diagnosed as having MS. Controls were asked to report their level of activity 10 years ago compared with today. Ten years was chosen as the comparison point because the control sample was young (mean ± SD age: 38.2 ± 13.2 years), and it was necessary to compare their current activity level with a previous point in their adult life.16 To quantify their level of participation, both participants with MS and controls sorted cards into categories corresponding to numerical values: never done (no value), given up since diagnosis (MS)/since 10 years ago (controls) (0), do now (1), and do less frequently since diagnosis (MS)/since 10 years ago (controls) (0.5). This scoring system allowed for the calculation of each MS participant's current level of activity, past level of activity, and retention of activities since MS diagnosis. To calculate the percentage of activity retention, the current participation score was divided by the previous participation score and multiplied by 100.15 The ACS was originally developed for older adults with Alzheimer disease but has since been found reliable and valid in other populations, such as those with Parkinson disease, stroke, and traumatic brain injury,16–18 and across a broad range of ages (from children to elderly adults)15 19 and cultures.20 21
Everyday Behavior in MS Group
The Functional Behavior Profile (FBP)22 is a self-report questionnaire assessing current everyday life task performance, social interactions, and problem-solving ability. Higher total scores indicate more frequent engagement in functional behavior. As in previous studies (eg, see Goverover et al23), the FBP was used with participants with MS to document engagement in everyday life activities.
Cognitive Performance Capacity Measures in MS Group
Executive Functions. Subtests of the Delis–Kaplan Executive Function System (D-KEFS),24 including verbal fluency (subtests 1–3: letter fluency, category fluency, and category switching), trail making (subtest 4: number-letter switching), and color-word switching (subtests 3 and 4: inhibition and inhibition switching) were used in this study. The D-KEFS has been shown to be sensitive to deficits in executive functioning in numerous clinical populations, including MS.25 The average standard scores on the D-KEFS subtests were used to create a composite score. The resultant D-KEFS composite score served as the dependent variable in this study.
Verbal Memory. The California Verbal Learning Test, Second Edition (CVLT-II),26 was used to assess verbal memory. After the examiner reads 16 words aloud to participants, four words in each of four categories, participants are asked to recall as many words as possible. Five consecutive free recall trials are administered. Next, participants are administered a different 16-word list and are asked to recall as many words as they can from this second list. After a 20- to 25-minute delay, there are free and cued recall trials of the first list. In this study, total learning across trials 1 to 5 and delayed free recall were used as the dependent variables. The CVLT-II is widely used with persons with MS and has established reliability and validity.27
Processing Speed. The oral version of the Symbol Digit Modalities Test28 is widely accepted as a sensitive test of processing speed ability in people with MS, with demonstrated good reliability and validity.29 Participants are asked to use a coded key to match nine symbols with numerical digits. The final score is the correct number of substitutions performed in 90 seconds, ranging from 0 to 110. Correct responses were used as the dependent variable, and higher scores indicate a faster processing speed.
Processing Speed and Working Memory. The Paced Auditory Serial Addition Test (PASAT)30 has often been administered to people with MS31 to assess processing speed and working memory. The PASAT consists of two 60-number trials; single digits are presented every 3 seconds in the first trial and every 2 seconds in the second trial. Participants are asked to add each new digit to the digit immediately prior. The total number of correct responses across the two trials was the dependent variable.
Upper- and Lower-Extremities Motor Performance in MS Group
The Nine-Hole Peg Test (NHPT)32 and the Timed 25-Foot Walk test (T25FW)33 were used to assess motor performance because they are considered to be very sensitive to disability related to MS.34 The NHPT is a brief, standardized, quantitative test of upper extremity function, with both the dominant and nondominant hands being tested twice. Participants are asked to pick up nine pegs, one at a time, as quickly as possible and put them in the nine holes. Once they are in the holes, participants remove them one at a time as quickly as possible and return them to a shallow container. The total time to complete the task is recorded. Two consecutive trials performed with the dominant hand are immediately followed by two consecutive trials with the nondominant hand. The dependent variable in this study was the average completion time of the two dominant-hand trials.
The T25FW33 is a quantitative mobility and leg function performance test. The participant is instructed to walk a clearly marked 25-foot distance as quickly and safely as possible. Participants are timed from the start of the walk to the 25-foot mark. The task is immediately administered again by asking the participant to walk back to the start. Patients may use assistive devices when performing the task. An average time of both walking trials is used to score the test.
The Multiple Sclerosis Functional Composite was developed by the National Multiple Sclerosis Society31 to reflect the varied clinical expression of MS across patients and over time. The Multiple Sclerosis Functional Composite score is the average z scores of three tests described previously herein: the PASAT, the NHPT, and the T25FW.
Affect Symptoms in MS Group
The Beck Depression Inventory (BDI)35 is a 21-item questionnaire designed to measure depth of depression independent of psychiatric diagnosis. The items of the BDI contain four statements each that describe the intensity of a particular depression symptom. It has demonstrated good content, concurrent, and construct validity.36 In the present study, the total BDI score was used as a continuous variable.
Statistical Analyses
To compare the MS and control groups on past and present levels of activity and participation, two-way analysis of covariance with repeated measures was performed, with age as a covariate. Eta squared was used to determine the effect size. Bivariate correlational analyses were performed to assess relationships between percentage of retained activity and participation and demographic characteristics, cognitive performance, motor performance, depression symptoms, and functional status of persons with MS. Pearson correlation coefficients were used for the continuous variables. All the statistical tests were two-tailed, and an alpha level of P < .05 was considered significant.
Results
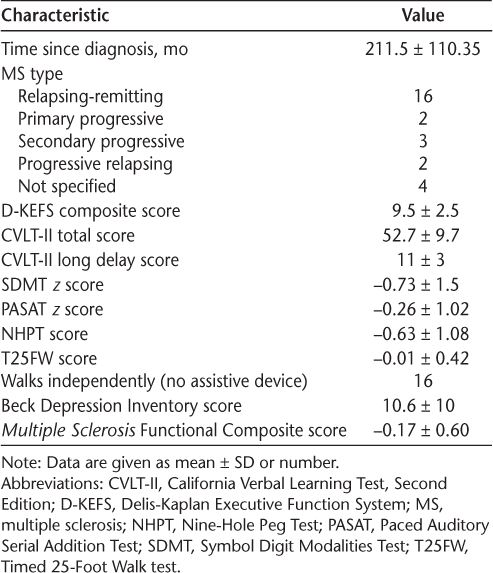
Participants with MS were significantly older than controls (mean ± SD age: 51.6 ± 8.9 years vs 38.2 ± 13.2 years, F 1,47 = 17.1, P < .001). The groups had similar mean ± SD levels of education (MS: 15.5 ± 1.6 years; controls: 14.5 ± 1.8 years). Time since MS diagnosis ranged from 72 to 432 (mean ± SD: 211.5 ± 110.35) months. Multiple Sclerosis Functional Composite scores ranged from −1.47 to 0.58 (mean ± SD: −0.17 ± 0.60). Sixteen participants with MS had relapsing-remitting disease course, two had primary progressive, three secondary progressive, and two progressive relapsing. Four participants did not specify a disease type. These demographic characteristics are detailed in Table 1.
Descriptive characteristics of the 27 study participants with MS
The difference in current and past levels of activity participation between the MS and control groups was examined first using group and time as two-way repeated measures of analysis of covariance, with age as a covariate (Table 2). A significant time × group interaction was found (F 1,45 = 4.9, P = .03, η2 = 0.099; small to medium effect). Control participants reported similar levels of activity over time, but participants with MS reported significantly lower current activity participation levels compared with past levels compared with controls (t 26 = −10.3, P < .001).
Differences between MS and control groups on past and current levels of activity, with age as a covariate
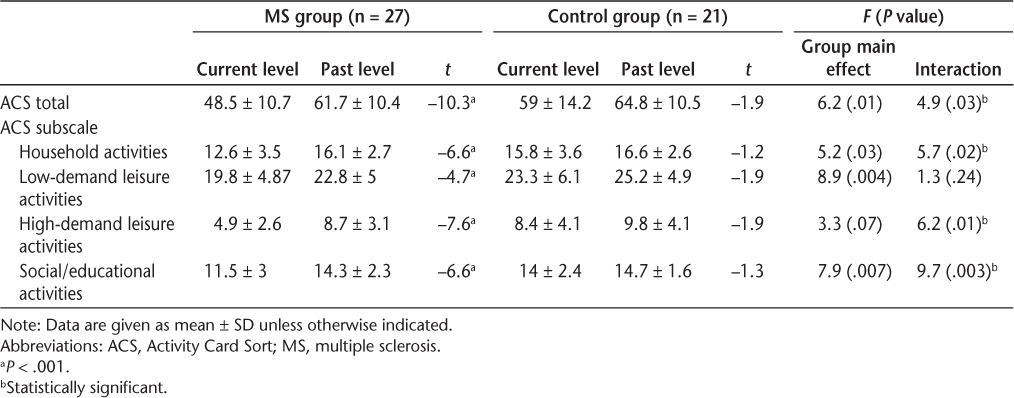
The ACS total and four subscales were examined individually (Table 2). There was a significant time × group interaction regarding level of activity participation in household activities, with a large effect size (F 1,45 = 5.7, P = .02, η2 = 0.108). Compared with controls, participants with MS showed a decline in household activity levels after diagnosis. A significant time × group interaction was noted for social activity and participation (F 1,45 = 9.7, P = .003, η2 = 0.17; large effect size), which shows that the decrease in current social activity participation for the MS group was significantly greater (t 26 = −6.6, P < .001) than that for the control group.
The group × time interaction was significant in high-demand leisure activities (F 1,45 = 6.2, P = .01, η2 = 0.115; large effect size). The MS group reported a larger decrease in levels of activity after diagnosis compared with before diagnosis than controls did for past versus present (t 26 = −7.6, P < .001). However, when activity participation in low-demand leisure activities was examined, the time × group interaction was not statistically significant, indicating the same pattern of decreased activity participation for both the MS and controls groups.
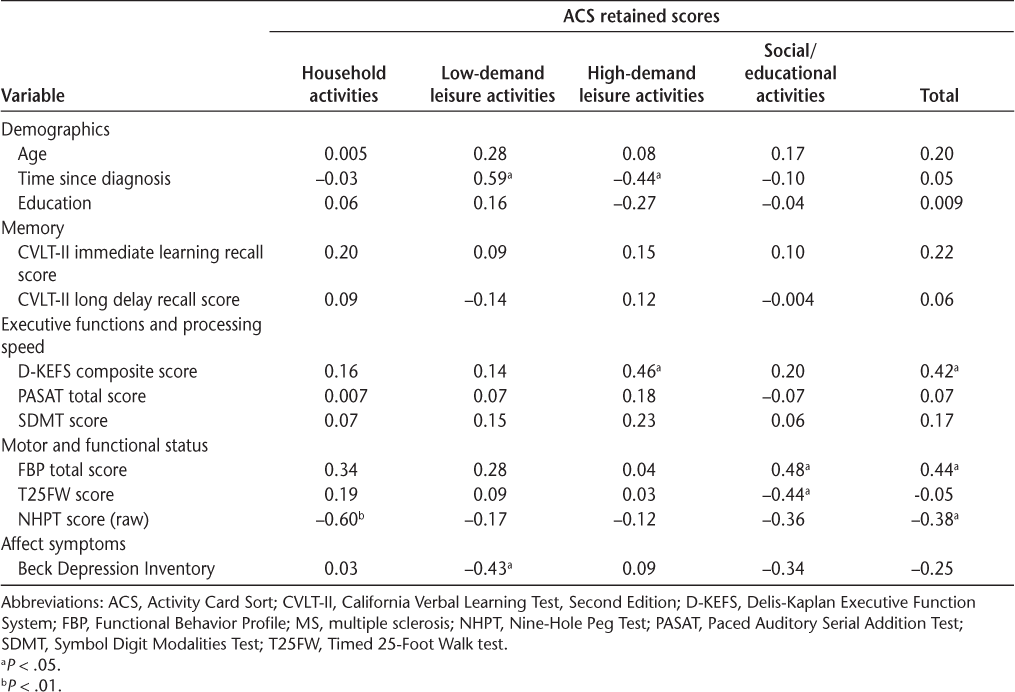
Pearson product moment correlations were performed to examine associations between participant demographic characteristics, ACS scores, and scores obtained on cognitive, functional status, depression symptom, and motor skill tests in persons with MS (Table 3). The mean ± SD scores included in this analysis are described in Table 1. Longer time since diagnosis and fewer depression symptoms were significantly associated with more retention of low-demand leisure activity participation. However, retention of high-demand leisure activity participation (eg, swimming, fishing, or hiking) was associated with better executive functioning and shorter time since MS diagnosis. Better functional status (as measured using the FBP) and better motor skills were associated with higher retained social activity since disease onset. Memory and processing speed were not associated with retained levels of activity participation.
Associations between ACS retained scores and demographics, cognitive and motor abilities, and functional status in MS group (N = 27)
Discussion
A major finding of this study is that participants with MS reported reduced participation in all activities after onset of the disease, as reflected in the percentage of activity retained. In addition, level of activity participation after diagnosis of MS is significantly lower than that in controls compared with 10 years ago. This was true for most activities considered: household activities (eg, doing laundry, watching the kids), high-demand leisure activities (eg, swimming, camping), and social activities (eg, traveling, family gathering). This finding is consistent with previous research that reports that persons with MS have difficulty performing ADLs37 38 and are not satisfied with their levels of participation in leisure and recreational activities.10 However, the novelty of the present study is that it assessed previous levels of activity participation compared with current levels to ascertain the degree of change after diagnosis and that it differentiates activity participation into various domains. The present study demonstrates not only that participants with MS are less involved in activity participation than controls but also that people with MS experience a decrease in participation in household, social, and high-demand leisure activities compared with activity participation before diagnosis.
Executive function was the only cognitive skill associated with retained activity participation in persons with MS. The present study results suggest that individuals with executive dysfunctions report decreased retained activity participation, especially in high-demand leisure activities. It may be that high-demand leisure activity requires persons with MS to adapt and plan to accommodate their current level of functioning to the high demands of the leisure activity, which, by definition, is demanding cognitively and physically. Several studies have noted that executive dysfunction is common in MS. For example, Ruano et al39 found that 40.8% of their entire study sample had executive function impairment, with the highest prevalence of impairment in those with primary progressive MS (92.3%). It is, thus, important that future work delineate executive dysfunction of persons with MS to establish its prevalence in this population and understand its relationship with activity participation.
Interestingly, mobility (as measured by the T25FW) was associated with the percentage of retained social/educational activity participation (ie, persons with faster walking speed retained more social and educational activities), and fine motor skills (as measured by the NHPT) were associated with the percentage of retained everyday life/household activity participation (ie, persons with better fine motor skills retained more household activities). The most visible symptom of MS frequently is loss of motor function; motor dysfunction usually occurs in the lower extremities, but upper extremity weakness and ataxia are also common.2 When considering the cognitive and motor requirements of both social/educational activity participation and fine motor skills, this dissociation is not surprising; that is, social and educational activities are usually performed outside the home and require transfer from place to place while getting to and engaging in such activities. Similarly, household activities tend to be more demanding of the fine motor system and require fine motor dexterity for successful completion.40 This finding corroborates existing evidence showing that motor and cognitive impairments are associated with activity limitations in MS, particularly regarding work/employment.41 In fact, motor skills have been shown to be predictive of performance of ADLs33 and of pathologic features, such as gray matter atrophy.34 Results of the present study support these findings but also reveal an interesting dissociation between type of motor impairment (gross vs fine) and type of activity (social vs household).
Given that individuals with MS commonly experience depression symptoms5 and that depression has been found to be significantly associated with quality of life and activity participation,12 especially when depression is assessed via self-report measures,23 we expected to observe a stronger association between depression symptoms and retained activity participation than what was found in the present study. However, a higher depression symptom profile was significantly associated only with less retained low-demand leisure activity. This finding is in concordance with those of other studies performed with elderly adults that found that engaging in leisure activities was associated with fewer depression symptoms.42 Note, however, that participants with MS in the present study were only mildly depressed, and, therefore, more studies are needed to investigate the variability of affect symptoms associated with MS and its effect on activity participation.
Another finding of the present study was that disease duration was associated with retention of low-demand leisure activities but not high-demand leisure activities. Previous studies have not differentiated between low- and high-demand leisure activities. It may be that people who were diagnosed with MS longer ago adjust better to disease symptoms by modifying their level of activity, and, therefore, they may retain low-demand leisure activity and give up high-demand leisure activity. At the same time, it is also possible that people who have had MS longer would have more disease symptoms that affect activity participation8 compared with people with shorter disease duration. Health professionals may need to determine where the “tipping” point is from high activity to low activity to help ascertain the best time to intervene to reduce the risk of decreasing activity.
The use of a small, nonrepresentative sample of individuals with MS and the cross-sectional design are among the limitations of this study. To confirm the results and determine the causal nature of the relationship between disease symptoms and activity participation, longitudinal investigation and path analyses with a larger, more representative cohort are needed. The lack of an age-matched control group is another limitation. A matched cohort should be identified for future studies. Including measurements of activity performance and a broader range of executive function skills could also be beneficial. Furthermore, the ACS is a self-report measure of activity participation. Self-reporting has its own weaknesses, such as the potential inability to accurately recall function before diagnosis or a lack of awareness regarding present activity performance. Specifically, some persons with MS were diagnosed 36 years before the present study, and, therefore, these participants may have difficulty recalling their activity levels before diagnosis. Last, information that may have helped explain reductions in participation were not collected, including household income, whether the participants lived alone, bladder/bowel dysfunction, etc. The inclusion and examination of such variables may help better explain participation issues in individuals with MS.
In conclusion, the quantitative measure of activity participation in this study, the ACS, may be beneficial in identifying areas of concern related to activity participation in people with MS and in directing rehabilitation efforts. Identifying the modifiable factors that may affect activity participation in persons with MS may allow clinicians to make more targeted rehabilitation recommendations, thus enhancing activity participation. This study is a good starting point for further research, as activity participation remains seldom studied in MS.
PRACTICE POINTS
People with MS report negative changes in activity participation in most aspects of life after diagnosis.
Changes in activity participation in people with MS are related to the types of symptoms an individual has, making it important to conduct individualized assessments to examine the risks of potential decreased activity participation in a given patient.
The quantitative measure of activity participation in this study, the Activity Card Sort, may be beneficial in directing rehabilitation efforts and should be considered for clinical use.
Financial Disclosures
The authors declare no conflicts of interest.
References
D'Orio VL, Foley FW, Armentano F, Picone MA, Kim S, Holtzer R. Cognitive and motor functioning in patients with multiple sclerosis: neuropsychological predictors of walking speed and falls. J Neurol Sci. 2012;316:42–46.
Benedict RHB, Holtzer R, Motl RW, et al. Upper and lower extremity motor function and cognitive impairment in multiple sclerosis. J Int Neuropsychol Soc. 2011;17:643–653.
Chiaravalloti ND, DeLuca J. Cognitive impairment in multiple sclerosis. Lancet Neurol. 2008;7:1139–1151.
Siegert RJ, Abernethy DA. Depression in multiple sclerosis: a review. J Neurol Neurosurg Psychiatry. 2005;76:469–475.
Feinstein A. Multiple sclerosis and depression. Mult Scler. 2011;17:1276–1281.
Goverover Y, Haas S, DeLuca J. Money management activities in persons with multiple sclerosis. Arch Phys Med Rehabil. 2016;97:1901–1907.
Goverover Y, Strober LB, Chiaravalloti N, DeLuca J. Factors that moderate activity limitation and participation restriction in people with multiple sclerosis. Am J Occup Ther. 2015;69:1–9.
Basak T, Unver V, Demirkaya S. Activities of daily living and self-care agency in patients with multiple sclerosis for the first 10 years. Rehabil Nurs. 2015;40:60–65.
Kearney BY, Fleischer BJ. Development of an instrument to measure exercise of self-care agency. Res Nurs Health. 1979;2:25–34.
Karhula ME, Kanelisto KJ, Ruutiainen J, Hämäläinen PI, Salminen A-L. The activities and participation categories of the ICF Core Sets for multiple sclerosis from the patient perspective. Disabil Rehabil. 2013;35:492–497.
Vanner EA, Block P, Christodoulou CC, Horowitz BP, Krupp LB. Pilot study exploring quality of life and barriers to leisure-time physical activity in persons with moderate to severe multiple sclerosis. Disabil Health J. 2008;1:58–65.
Ben Ari (Shevil) E, Johansson S, Ytterberg C, Bergström J, von Koch L. How are cognitive impairment, fatigue and signs of depression related to participation in daily life among persons with multiple sclerosis? Disabil Rehabil. 2014;36:2012–2018.
Newitt R, Barnett F, Crowe M. Understanding factors that influence participation in physical activity among people with a neuromusculoskeletal condition: a review of qualitative studies. Disabil Rehabil. 2016;38:1–10.
Polman CH, Reingold SC, Banwell B, et al. Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann Neurol. 2011;69:292–302.
Baum CM, Edwards D; American Occupational Therapy Association. ACS Activity Card Sort. AOTA Press; 2008.
Goverover Y, Genova H, Smith A, Chiaravalloti N, Lengenfelder J. Changes in activity participation following traumatic brain injury. Neuropsychol Rehabil. 2017;27:472–485.
Hartman-Maeir A, Soroker N, Ring H, Avni N, Katz N. Activities, participation and satisfaction one-year post stroke. Disabil Rehabil. 2007;29:559–566.
Spitzer J, Tse T, Baum C, Carey L. Mild cognitive impairment after stroke is associated with activity participation in an Australian cohort. Int J Stroke. 2010;5:S8–S15.
Katz N, Karpin H, Lak A, Furman T, Hartman-Maeir A. Participation in occupational performance: reliability and validity of the Activity Card Sort. OTJR Occup Particip Heal. 2003;23:10–17.
Hamed R, Holm MB. Psychometric properties of the Arab Heritage Activity Card Sort. Occup Ther Int. 2013;20:23–34.
Chan VWK, Chung JCC, Packer TL. Validity and reliability of the Activity Card Sort-Hong Kong version. OTJR Occup Particip Heal. 2006;26:152–158.
Baum C, Edwards DF, Morrow-Howell N. Identification and measurement of productive behaviors in senile dementia of the Alzheimer type. Gerontologist. 1993;33:403–408.
Goverover Y, Kalmar J, Gaudino-Goering E, et al. The relation between subjective and objective measures of everyday life activities in persons with multiple sclerosis. Arch Phys Med Rehabil. 2005;86:2303–2308.
Delis D, Kaplan E, Kramer J. Delis-Kaplan Executive Function System (D-KEFS). Can J Sch Psychol. 2001;20:117–128.
Delis DC, Kramer JH, Kaplan E, Holdnack J. Reliability and validity of the Delis-Kaplan Executive Funciton System: an update. J Int Neuropsychol Soc. 2004;10:301–303.
Delis DC, Kramer JH, Kaplan E, Ober BA. California Verbal Learning Test: Adult Version (CVLT-II): Manual. 2nd ed. San Antonio, TX: The Psychological Corporation; 2000.
Stegen S, Stepanov I, Cookfair D, et al. Validity of the California Verbal Learning Test-II in multiple sclerosis. Clin Neuropsychol. 2010;24:189–202.
Smith A. Symbol Digit Modalities Test (SDMT) manual (revised). West Psychol Serv. 1982;c:1–37.
Benedict RHB, DeLuca J, Phillips G, LaRocca N, Hudson LD, Rudick R. Validity of the Symbol Digit Modalities Test as a cognition performance outcome measure for multiple sclerosis. Mult Scler. 2017;23:721–733.
Rudick R, Antel J, Confavreux C, et al. Recommendations from the National Multiple Sclerosis Society Clinical Outcomes Assessment Task Force. Ann Neurol. 1997;42:379–382.
Fischer JS, Rudick RA, Cutter GR, Reingold SC; National MS Society Clinical Outcomes Assessment Task Force. The Multiple Sclerosis Functional Composite Measure (MSFC): an integrated approach to MS clinical outcome assessment. Mult Scler. 1999;5:244–250.
Earhart GM, Cavanaugh JT, Ellis T, Ford MP, Foreman KB, Dibble L. The 9-Hole Peg Test of upper extremity function. J Neurol Phys Ther. 2011;35:157–163.
Kaufman M, Moyer D, Norton J. The significant change for the Timed 25-Foot Walk in the Multiple Sclerosis Functional Composite. Mult Scler. 2000;6:286–290.
Kragt JJ, Van Der Linden F, Nielsen JM, Uitdehaag BMJ, Polman CH. Clinical impact of 20% worsening on Timed 25-Foot Walk and 9-Hole Peg Test in multiple sclerosis. Mult Scler. 2006;12:594–598.
Beck A, Steer R, Carbin M. Psychometric properties of the Beck Depression Inventory: twenty-five years of evaluation. Clin Psychol Rev. 1988;8:77–100.
Benedict RHB, Fishman I, McClellan MM, Bakshi R, Weinstock-Guttman B. Validity of Beck Depression Inventory-Fast Screen in multiple sclerosis. Mult Scler. 2003;9:393–396.
Goverover Y, Chiaravalloti N, DeLuca J. Brief International Cognitive Assessment for Multiple Sclerosis (BICAMS) and performance of everyday life tasks: actual reality. Mult Scler. 2015;22:544–550.
Costa SL, DeLuca J, Sandroff BM, Goverover Y, Chiaravalloti ND. Role of demographic and clinical factors in cognitive functioning of persons with relapsing-remitting and progressive multiple sclerosis. J Int Neuropsychol Soc. 2018;24:139–146.
Ruano L, Portaccio E, Goretti B, et al. Age and disability drive cognitive impairment in multiple sclerosis across disease subtypes. Mult Scler. 2017;23:1258–1267.
Öhrvall AM, Eliasson AC, Löwing K, Ödman P, Krumlinde-Sundholm L. Self-care and mobility skills in children with cerebral palsy, related to their manual ability and gross motor function classifications. Dev Med Child Neurol. 2010;52:1048–1055.
Bishop M, Rumrill PD. Multiple sclerosis: etiology, symptoms, incidence and prevalence, and implications for community living and employment. Work. 2015;52:725–734.
Fulbright SA. Rates of depression and participation in senior centre activities in community-dwelling older persons. J Psychiatr Ment Health Nurs. 2010;17:385–391.







