Publication
Research Article
International Journal of MS Care
Benefits of Adhering to the Canadian Physical Activity Guidelines for Adults with Multiple Sclerosis Beyond Aerobic Fitness and Strength
Abstract
Background:
The Canadian Physical Activity Guidelines for Adults with Multiple Sclerosis (PAGs) were released in 2013 but have yet to be validated. We aimed to test the effectiveness of the PAGs in improving fitness, mobility, fatigue symptoms, and quality of life (QOL) in a large cohort of adults with multiple sclerosis (MS).
Methods:
As part of an ongoing randomized controlled trial examining implementation of the PAGs, participants were randomized to either a direct referral group (physician referral to an exercise program following the PAGs; n = 42) or a control group (provided a print copy of the PAGs; n = 37). Physical activity behavior was assessed through weekly physical activity logs. Fitness, mobility, fatigue symptoms, and QOL were assessed at baseline and after 16 weeks. Participants were categorized as either PAG adherers (n = 30) or nonadherers (n = 49) to the PAGs based on achieving the weekly exercise recommendations at least 75% of the time.
Results:
Adherence to the PAGs was twice as high in the referral group compared with the control group. Adherers experienced significantly greater improvements in peak oxygen consumption (29%), strength (7%–18%), mobility (16%), fatigue symptoms (−36%), and QOL (17%–22%) compared with nonadherers (P < .05).
Conclusions:
Following the PAGs for at least 12 of 16 weeks results in improvements in fitness, mobility, fatigue symptoms, and QOL, confirming their effectiveness for improving health in people with MS.
An estimated 100,000 Canadians currently are living with multiple sclerosis (MS), a degenerative neurologic disease that has a wide range of debilitating symptoms, including muscle weakness, extreme fatigue, loss of balance, impaired speech, double vision, declining cognitive function, and paralysis.1 Physical activity is one strategy that has been proposed to counteract the disabling symptoms of MS, and it is gaining increasing attention for its potential as a disease-modifying intervention. Accumulating evidence indicates that engaging in physical activity can improve or maintain functional ability, aerobic fitness, strength, fatigue symptoms, quality of life (QOL), depression, cognitive function, and chronic disease risk profiles in people with MS.2 3 Despite the benefits of physical activity, most people with MS are physically inactive, a behavior that is now known to carry its own specific risk regarding the development of cardiometabolic chronic diseases.4 5
Health care and service providers have struggled in the past in providing recommendations for physical activity for people with MS because there were no evidence-based guidelines on appropriate doses, intensities, and types of exercises to perform in this population. In 2013, the evidence-based Canadian Physical Activity Guidelines for Adults with Multiple Sclerosis (PAGs) were released. These guidelines suggest that to attain important fitness benefits, adults aged 18 to 64 years with MS who have mild-to-moderate disability need at least 30 minutes of moderate-intensity aerobic activity twice weekly and strength training exercises for major muscle groups twice weekly.6
Improvements in cardiovascular fitness and strength after a physical activity intervention have been demonstrated by many.2 7 8 However, the difficulty with interpreting these studies is that the authors have used different doses and types of physical activity. Having disease-specific guidelines can help researchers conduct studies using the same dose of stimulus and provide a clear physical activity promotion message to patients.
No study has validated the PAGs and provided scientific evidence that the recommended dose is effective in improving both fitness and health in people with MS. Therefore, the objectives of this study were to test the effectiveness of the PAGs for adults with MS and to affirm that following the PAGs for 16 weeks results in improved fitness, mobility, fatigue symptoms, and QOL.
Methods
Participants
Detailed recruitment and enrollment information is provided in the CONSORT diagram (Figure S1, published in the online version of this article at ijmsc.org). The Expanded Disability Status Scale (EDSS) is a way to measure disability in MS. The scale ranges from 0 to 10, with higher levels indicative of greater disability. People with MS (all types) with an EDSS score between 1 and 7 (to include varying levels of disability up to the level at which participants could not engage in the protocol) who were aged 18 to 64 years were recruited to participate from July 1, 2014, through August 31, 2017, through advertisements at the local MS Society of Canada chapter in Hamilton, Ontario. Exclusion criteria included any medical condition that would impair ability to participate in strength or aerobic exercises and participation in regular exercise (at least twice weekly). All the participants provided written informed consent, and all the procedures were approved and conducted in accordance with the ethical guidelines of the Hamilton Integrated Research Ethics Board (Hamilton, ON, Canada). After baseline tests were completed, participants were randomized to a direct referral group or a control group. All the testers were blinded to randomization until after baseline tests were completed. Participants randomized to the referral group were prescribed exercise based on the PAGs by a physician and were referred to a community-based exercise program at McMaster University in Hamilton, Ontario. The exercise prescription in the PAGs is at least 30 minutes of moderate-intensity aerobic activity 2 times per week and strength training exercises for major muscle groups 2 times per week.6 Participants randomized to the control group were given a print copy of the PAGs and an online link for information about physical activity and MS. In both groups, no monetary funds were given to pay for exercise program memberships or transportation costs to replicate a real-world, community-based setting.
Community-Based Exercise Program
Participants randomized to the referral group were referred to a community-based exercise program at McMaster University. Participants who were in the control group were not given the referral to the community-based exercise program, but, if they asked about the program after hearing about it in the community, they were able to join. The supervised program ran twice per week, each session lasting 1 to 1.5 hours, and participants were prescribed exercise based on the PAGs. Every program was individualized to participants' needs and changed every 4 weeks to keep progression and stimulus constant. The programs consisted of 10 minutes of aerobic exercise on the arm bike to start, followed by two to three sets of approximately eight to ten different strength exercises for the upper and lower body and 20 minutes of aerobic exercise on a recumbent cross trainer (NuStep LLC, Ann Arbor, MI) after the strengthening exercises were completed. Participants were prompted regularly for their ratings of perceived exertion (RPEs) after aerobic and resistance exercises to determine the intensity of the exercise program. Exercise trainers aimed to have participants achieve a score of 4 to 6 on the 10-point RPE scale9 to reach the moderate-intensity threshold of the PAGs. The equipment used for the aerobic exercise included an arm cycle ergometer (Monark arm ergometer, Patterson Medical Supply Inc, Mississauga, ON, Canada) and a hybrid recumbent stepper (NuStep T5XR). Resistance exercise was completed using a combination of multistation-accessible weight stacks (Equalizer Exercise Machines, Red Deer, AB, Canada), wall pulleys (Endorphin Pulleys, Patterson Medical Supply Inc), and free weights.
Survey and Anthropometric Assessment
At baseline and after the intervention period, participants completed a series of questionnaires assessing demographics, QOL, and fatigue symptoms. The MS Quality of Life–54 questionnaire, which contains 54 questions relating to physical, cognitive, and sexual functioning, was used to assess QOL.10 Fatigue was assessed using the Modified Fatigue Impact Scale–5, a five-item questionnaire asking about fatigue symptoms and how they have affected the participant's life during the past month.11 The five-item scale was used instead of the full version to reduce participant burden. The total possible score is 20, with a higher score indicating greater impact of fatigue on daily life.
A questionnaire to determine participants' satisfaction with the PAGs was administered after the intervention. All the items were rated on a 7-point Likert scale from 1 (strongly disagree) to 7 (strongly agree). Satisfaction with the aerobic and strengthening portions of the guidelines were evaluated, along with perception of pain (I was able to complete the exercises without any additional pain or discomfort) and enjoyment of exercise (Overall, I enjoyed the exercise program).
Fitness and Mobility Assessment
To measure peak oxygen consumption (VO2peak), participants performed a progressive exercise test on an arm cycle ergometer (Lode B.V., Groningen, the Netherlands) to VO2peak or exhaustion. The resistance started at 0 W and increased thereafter by 10 W every minute, and participants were asked to keep the cycling cadence between 50 and 60 rpm. Expired gas and ventilatory parameters were acquired throughout the protocol using the Moxus Metabolic System (AEI Technologies, Pittsburgh, PA). Continuous measures of heart rate were obtained throughout the entire test (Polar Electro, Lachine, QC, Canada). Central (eg, breathing) and peripheral (eg, arm fatigue) RPEs were acquired every minute. The test was terminated if 1) the participant reached volitional exhaustion, 2) the cycling rate dropped below 50 rpm 3) a plateau in VO2 was observed, or 4) heart rate was greater than 90% of the participant's age-predicted maximum heart rate.
Muscle strength testing was completed on a multistation (wheelchair-accessible) weight training system (Equalizer Multistation), unilateral wall pulleys (Endorphin Pulleys), and a leg extension/flexion machine (HUR Health & Fitness Canada Inc [now HUR USA Inc, Northbrook, IL]). One repetition maximum (1RM) was assessed using established procedures12 in standardized order of latissimus pulldown, chest press, bicep curl, shoulder flexion and extension, and knee flexion and extension exercises. The participants were provided with enough rest between exercises to ensure that muscles did not fatigue before reaching maximum. A composite strength score was calculated as the sum of the 1RMs for each muscle group divided by the total number of muscle groups.
Mobility was assessed using the Timed 25-Foot Walk test. Participants were instructed to walk 25 feet as quickly but safely as possible and in their usual manner (walking aids permitted if needed); they repeated this twice. An average of the walking speeds for the two attempts was calculated.
Adherence
Adherence was assessed by having participants fill out weekly physical activity logs for 16 weeks. There were separate log entries for aerobic and strengthening exercises, which included information about the type, duration, and intensity of the exercise each day. For participants in the referral group, their physical activity logs were cross-referenced to the attendance records and exercise worksheets from the exercise program for accuracy. By evaluating the weekly logs, adherence to the PAGs was calculated based on the number of weeks in which the recommendations were achieved over the 16 weeks. Participants were classified as adherers if they met the recommendations for 12 of 16 weeks, or had a calculated adherence rate of at least 75%.
Statistical Analyses
Continuous variables are reported as mean ± SD, and categorical variables are presented as frequencies and prevalence values. Baseline and posttesting values were compared using two-way (group × time) repeated-measures analysis of variance. All the statistical analyses were performed using IBM SPSS Statistics for Windows, version 24.0 (IBM Corp, Armonk, NY). Statistical significance was set at α < .05.
Results
Participant Characteristics
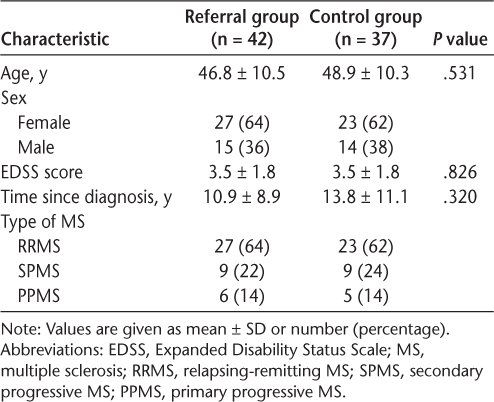
Of 91 participants randomized (Figure S1), 79 completed the 16-week randomized controlled trial (mean ± SD: age, 47.9 ± 10.0 years; EDSS score, 3.5 ± 1.8; years living with MS, 12.1 ± 10.0). Participant characteristics stratified by group are presented in Table 1. There were no significant differences in demographic characteristics between groups.
Participant characteristics
Adherence
The mean ± SD adherence rate in the referral group was 68.0% ± 28.6% versus 35.1% ± 35.0% in the control group (P < .05). There was a considerable range of adherence rates in each group; for example, 20 people in the referral group did not adhere and eight people in the control group did adhere. Thus, to test the effectiveness of the PAGs, post hoc categorization into adherers and nonadherers was warranted for analysis of fitness and functional outcomes. Using a 75% adherence rate to define an adherer, 30 people were categorized as adherers and 49 people were categorized as nonadherers. There were no significant differences in baseline characteristics between adherers and nonadherers.
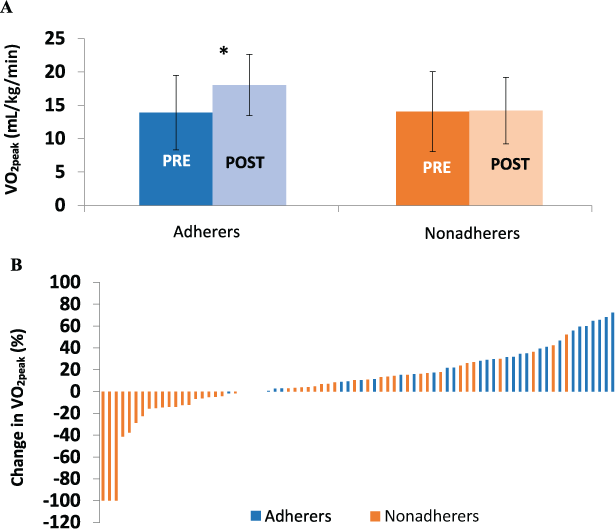
Peak Aerobic Capacity
Changes in aerobic capacity are presented in Figure 1A. There was a significant increase in VO2peak (group × time interaction: F = 52.99, P < .0001) in adherers after 16 weeks of following the PAGs. Nonadherers experienced no change in VO2peak after the 16-week training period. Individual training responses in VO2peak are presented in Figure 1B.
Mean ± SD changes in peak oxygen consumption (VO2peak) in adherers versus nonadherers (A) and mean changes in individual training responses in VO2peak for each participant (B) after 16 weeks
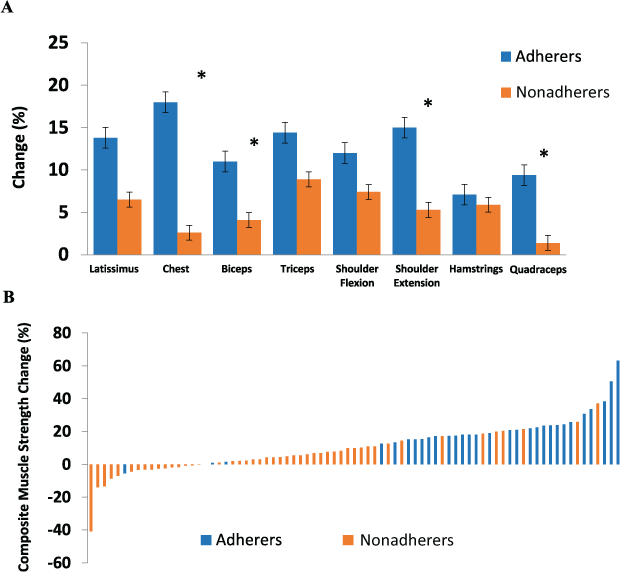
Muscle Strength
Changes in muscle strength in different muscle groups are presented in Figure 2A. Both adherers and nonadherers improved strength in every muscle group (main effect of time: P < .05), but greater improvements were observed in adherers for the chest (F = 6.35, P = .015), biceps (F = 5.73, P = .021), shoulder extensors (F = 6.03, P = .018), and quadriceps muscles (F = 2.27, P = .046) (group × time interactions). Individual training responses in overall muscle strength are presented in Figure 2B.
Mean ± SD changes in strength in each muscle group in adherers versus nonadherers (A) and mean changes in individual training responses in overall strength for each participant (B) after 16 weeks
Fatigue
Changes in perceived fatigue are presented in part A of Figure 3. There was a significant reduction in mean ± SD fatigue symptoms in both groups (main effect of time: P < .0001), but a greater reduction was seen in adherers (pre: 11.0 ± 3.2; post: 6.6 ± 2.8) compared with nonadherers (pre: 10.9 ± 4.2; post: 8.8 ± 4.5) after 16 weeks of following the PAGs (group × time interaction: F = 4.36, P = .046).
Mean ± SD changes in fatigue A) and changes in mobility B) in adherers versus nonadherers after 16 weeks
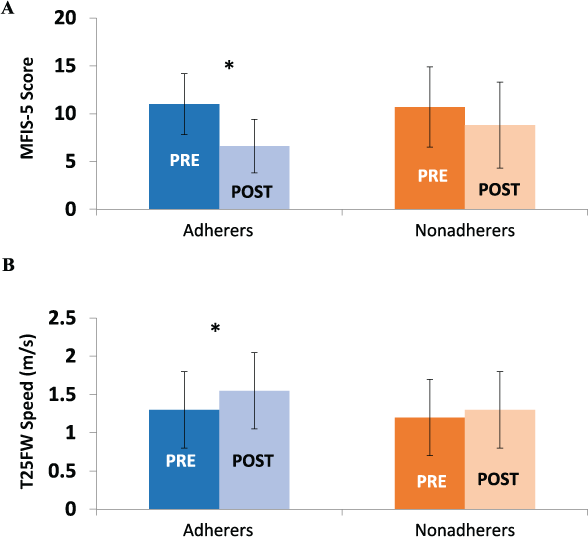
Mobility
Changes in mobility assessed by the 25-Foot Walk test are presented in part B of Figure 3. There was a significant increase in walking speed for the Timed 25-Foot Walk test (group × time interaction: F = 11.02, P = .002) in adherers after 16 weeks of following the PAGs (pre: 1.4 ± 0.5 m/s; post: 1.6 ± 0.5 m/s), with no change in nonadherers.
Health-Related QOL
Mental and physical health-related QOL scores were not different between groups at baseline, and both adherers and nonadherers significantly improved their mental and physical health-related QOL after following the PAGs for 16 weeks (main effect of time: P < .0001). However, greater improvements in both aspects of QOL were observed in adherers (group × time interaction: mental QOL, F = 4.28, P = .044; physical QOL, F = 7.37, P = .009) compared with nonadherers. Mean changes for adherers were 11.66 for mental QOL and 12.1 for physical QOL versus 5.32 for mental QOL and 4.8 for physical QOL for nonadherers.
Satisfaction with Guidelines
Mean ± SD satisfaction with the aerobic (6.2 ± 1.0) and resistance (6.3 ± 1.0) exercises in people with MS was high (maximum score of 7). Mean ± SD overall enjoyment of the exercise program was also very high (6.6 ± 1.0, maximum score of 7). Participants were able to complete the exercise program without any additional increases in pain or discomfort.
Discussion
To our knowledge, this is the first study to test the effectiveness of the Canadian Physical Activity Guidelines for Adults with Multiple Sclerosis published in 2013.6 The studies from which the PAGs were developed generally used exercise interventions lasting 12 to 24 weeks, so we chose a 16-week period in the present study to test the effectiveness of the guidelines. By evaluating weekly physical activity logs, we could determine how many weeks the guideline recommendations were met in each participant. Note that not meeting the recommendations in any given week did not necessarily mean that the participant was “inactive” that week; it could have been that they only did, for example, 25 minutes of moderate-intensity exercise on 1 day and so failed to meet the 60-minute total (30 minutes × 2 days) stipulated in the guidelines. The present findings suggest that adhering to the PAGs at least 75% of the time over 16 weeks results in significant improvements in aerobic capacity (29%), strength (7%–18%), fatigue symptoms (−36%), mobility (16%), and QOL (17%–22%). Currently there is no gold standard defining what constitutes physical activity adherence or the number of training sessions needed to reap the benefits of physical activity. An adherence rate of 75% was chosen as the threshold to classify an adherer after comparing definitions and justifications for physical activity adherence across a variety of studies in other populations.13–17
Individuals with MS characteristically have low aerobic fitness levels compared with their healthy counterparts18 19; however, exercise training programs can improve aerobic fitness in the MS population by as much as 22%.18 Previous studies evaluating aerobic training in the MS population have varied in trial duration (3–26 weeks), number of sessions (2–5 times per week), and the length of each training session (15–45 minutes).18 In the present study, participants who adhered to the PAGs had a 29% increase in VO2peak. This is greater than the approximately 10% to 22% increase reported in previous studies,18 but it could be partly due to our measuring VO2peak using an arm ergometer. As reflected in Figures 1 and 2, there was considerable individual variability in the change in fitness observed in the participants, which supports previous literature in other populations.20–22 To our knowledge, this is the first study to graphically illustrate the individual variability in responses to aerobic and resistance training in the MS population. Closer examination of individual participants who showed improvements in aerobic fitness or strength without being labeled as an adherer indicated that these individuals were often just under the threshold criterion of what would constitute adherence (75%). These individual response graphs nicely illustrate that fitness improvements occur on a continuum, and people who may not have quite met the adherer criterion could still experience improvements in aerobic capacity and overall strength.
The improvements in muscle strength observed in this randomized controlled trial are similar to those in previous work in the MS population, indicating that 8 to 20 weeks of resistance training, 2 to 3 times per week at a moderate intensity significantly improves muscular strength.7 23 24 The greater improvements in strength across all muscle groups in adherers is likely indicative of the dose-response associated with a greater volume of training (more sessions attended, greater strength improvements).
The improvements seen in aerobic fitness and overall strength after following the PAGs were expected, but, arguably, the results that may be of even more importance are the improvements in fatigue symptoms, mobility, and health-related QOL. One of the most commonly reported and debilitating symptoms in the MS population is fatigue.11 Sixty-six percent of participants in this study were characterized by high levels of fatigue, having scores greater than 10 on the Modified Fatigue Impact Scale–5.25 After 16 weeks of following the PAGs, fatigue symptoms were significantly reduced to what would be categorized as low levels of fatigue. This is an extremely important result, countering historical precautions that exercising may actually increase fatigue symptoms. Research summarized by Heine and colleagues26 confirm these findings as well, indicating the association between exercising and improvements in fatigue symptoms in the MS population.
People with MS typically report decreased QOL compared with the general population,27 although physical activity participation has been demonstrated to improve health-related QOL in people with MS.3 28–32 The results of this randomized controlled trial confirm that the PAG activity recommendations are sufficient to improve QOL in people with MS; in fact, this is the first study to observe such large improvements in QOL after exercise training in the MS population. A mean difference in score of 16 was observed in the mental health composite score and a mean difference of 13 in the physical health composite score for adherers after 16 weeks of following the PAGs.
Mobility impairment in the MS population results in difficulties in maintaining independence and is one of the most life-altering symptoms associated with MS.33 The Timed 25-Foot Walk test is regularly used in both clinical and research-based settings34 to assess walking mobility. Studies using resistance and/or aerobic training programs in the MS population have reported improvements in walking speed and endurance.7 35 The results of this study are aligned with previous research7 31 32 35 suggesting that 16 weeks of following the PAGs for people with MS is associated with improved walking speed. These improvements may translate to improvements in completing activities of daily living and community independence in people with MS.
The responses from the questionnaire about satisfaction with the PAGs indicate that participants rated the guidelines for adults with MS quite highly, and they were able to complete the exercise sessions without any pain or discomfort. The results from this trial demonstrate not only that the PAGs are effective but that they are also palatable in adults with MS.
It was encouraging to note that many of the nonadherers also improved in many of the measured outcomes (although not to the same degree as adherers). This indicates that even if someone is unable to meet the specific PAG recommendations, the performance of some degree of physical activity is still beneficial. A limitation to note is that the participants' performed the 1RM strength testing after the VO2peak test on the arm ergometer. Although rest time was given to participants, some of the upper body strength measures may have been compromised due to lingering muscle fatigue.
In conclusion, the PAGs are effective in inducing significant improvements in physical fitness, fatigue symptoms, mobility, and QOL. Moreover, the PAGs are both feasible and palatable to this patient population. Physicians and health care professionals should highly encourage their patients to use these guidelines as a starting point toward incorporating physical activity into their lives to improve fitness, fatigue symptoms, mobility, and QOL while living with MS.
PRACTICE POINTS
This study highlights the effectiveness of the Canadian Physical Activity Guidelines for Adults with Multiple Sclerosis and stresses that following the guidelines leads to improvements in fitness, mobility, fatigue symptoms, and overall quality of life.
Physicians and health care professionals should highly encourage their patients to use the guidelines as a starting point toward incorporating physical activity into their lives to improve health and function while living with MS.
Financial Disclosures
The authors declare no conflicts of interest.
References
MS Society of Canada. What is MS? https://mssociety.ca/about-ms/what-is-ms. Accessed January 2019.
Latimer-Cheung AE, Pilutti LA, Hicks AL, et al. Effects of exercise training on fitness, mobility, fatigue, and health-related quality of life among adults with multiple sclerosis: a systematic review to inform guideline development. Arch Phys Med Rehabil. 2013;94:1800–1828.e3.
Mostert S, Kesselring J. Effects of a short-term exercise training program on aerobic fitness, fatigue, health perception and activity level of subjects with multiple sclerosis. Mult Scler. 2002;8:161–168.
Motl RW, Mcauley E, Sandroff B, Hubbard E. Descriptive epidemiology of physical activity rates in multiple sclerosis. Acta Neurol Scand. 2015;131:422–425.
Sandroff B, Dlugnski D, Weikert M, Suh Y, Balantrapu S, Motl R. Physical activity and multiple sclerosis: new insights regarding inactivity. Acta Neurol Scand. 2012;126:256–262.
Latimer-Cheung AE, Martin Ginis KA, Hicks AL, et al. Development of evidence-informed physical activity guidelines for adults with multiple sclerosis. Arch Phys Med Rehabil. 2013;94:1829–1836.e7.
Dalgas U, Stenager E, Jakobsen J, et al. Resistance training improves muscle strength and functional capacity in multiple sclerosis. Neurology. 2009;73:1478–1484.
Platta ME, Ensari I, Motl RW, Pilutti LA. Effect of exercise training on fitness in multiple sclerosis: a meta-analysis. Arch Phys Med Rehabil. 2016;97:1564–1572.
Borg G. Psychophysical bases of perceived exertion. Med Sci Sport Exerc. 1982;14:377–381.
Vickrey BG, Hays RD, Harooni R, et al. A health-related quality of life measure for multiple sclerosis. Qual Life Res. 1995;4:187–206.
Fisk JD, Ritvo PG, Ross L, et al. Measuring the functional impact of fatigue: initial validation of the Fatigue Impact Scale. Clin Infect Dis. 1994;18:S79–S83.
Kraemer W, Ratamess N, Fry A, French D. Strength training: development and evaluation of methodology. In: Maud P, Foster C, eds. Physiological Assessment of Human Fitness. Human Kinetics; 2006:119–150.
Deka P, Pozehl B, Williams MA, Yates B. Adherence to recommended exercise guidelines in patients with heart failure. Heart Fail Rev. 2017;22:41–53.
Geraedts HAE, Zijlstra W, Zhang W, Bulstra S, Stevens M. Adherence to and effectiveness of an individually tailored home-based exercise program for frail older adults, driven by mobility monitoring: design of a prospective cohort study. BMC Public Health. 2014;14:1–7.
Hicks G, Benvenuti F, Fiaschi V, et al. Adherence to a community-based exercise program is a strong predictor of improved back pain status in older adults: an observational study. Clin J Pain. 2013;28:195–203.
Kampshoff CS, van Mechelen W, Schep G, et al. Participation in and adherence to physical exercise after completion of primary cancer treatment. Int J Behav Nutr Phys Act. 2016;13:100.
Kronish IM, Diaz KM, Goldsmith J, Moise N, Schwartz JE. Objectively measured adherence to physical activity guidelines after acute coronary syndrome. J Am Coll Cardiol. 2017;69:1205–1207.
Langeskov-Christensen M, Heine M, Kwakkel G, Dalgas U. Aerobic capacity in persons with multiple sclerosis: a systematic review and meta-analysis. Sports Med. 2015;45:905–923.
Koseoglu BF, Gokkaya NKO, Ergun U, Inan L, Yesiltepe E. Cardiopulmonary and metabolic functions, aerobic capacity, fatigue and quality of life in patients with multiple sclerosis. Acta Neurol Scand. 2006;114:261–267.
Ross R, de Lannoy L, Stotz PJ. Separate effects of intensity and amount of exercise on interindividual cardiorespiratory fitness response. Mayo Clin Proc. 2015;90:1506–1514.
Hautala A, Kiviniemi A, Makikallio T, et al. Individual differences in the responses to endurance and resistance training. Eur J Appl Physiol. 2006;96:535–542.
Sisson SB, Katzmarzyk PT, Earnest CP, Bouchard C, Blair SN, Church TS. Volume of exercise and fitness nonresponse in sedentary, postmenopausal women. Med Sci Sport Exerc. 2009;41:539–545.
Kjølhede T, Vissing K, Dalgas U. Multiple sclerosis and progressive resistance training: a systematic review. Mult Scler. 2012;18:1215–1228.
Broekmans T, Roelants M, Feys P, et al. Effects of long-term resistance training and simultaneous electro-stimulation on muscle strength and functional mobility in multiple sclerosis. Mult Scler. 2010;17:468–477.
Garg H, Bush S, Gappmaier E. Associations between fatigue and disability, functional mobility, depression, and quality of life in people with multiple sclerosis. Int J MS Care. 2016;18:71–77.
Heine M, van de Port I, Rietberg M, van Wegen EE, Kwakkel G. Exercise therapy for fatigue in multiple sclerosis. Cochrane Database Syst Rev. 2015;(9):CD009956.
Mitchell AJ, Benito-León J, González J-MM, Rivera-Navarro J. Quality of life and its assessment in multiple sclerosis: integrating physical and psychological components of wellbeing. Lancet Neurol. 2005;4:556–566.
Oken BS, Kishiyama S, Zajdel D, et al. Randomized controlled trial of yoga and exercise in multiple sclerosis. Neurology. 2004;62:2058–2064.
Schulz K-H, Gold SM, Witte J, et al. Impact of aerobic training on immune-endocrine parameters, neurotrophic factors, quality of life and coordinative function in multiple sclerosis. J Neurol Sci. 2004;225:11–18.
Motl RW, Gosney J. Effect of exercise training on quality of life in multiple sclerosis: a meta-analysis. Mult Scler. 2008;14:129–135.
Rampello A, Franceschini M, Piepoli M, et al. Effect of aerobic training on walking capacity and maximal exercise tolerance in patients with multiple sclerosis: a randomized crossover controlled study. Phys Ther. 2007;87:545–555.
Pilutti LA, Lelli DA, Paulseth JE, et al. Effects of 12 weeks of supported treadmill training on functional ability and quality of life in progressive multiple sclerosis: a pilot study. Arch Phys Med Rehabil. 2011;92:31–36.
La Rocca NG. Impact of walking impairment in multiple sclerosis perspectives of patients and care partners. Patient. 2011;4:189–201.
Goldman MD, Motl RW, Scagnelli J, Pula JH, Sosnoff JJ, Cadavid D. Clinically meaningful performance benchmarks in MS Timed 25-Foot Walk and the real world. Neurology. 2013;81:1856–1863.
Cakt BD, Nacir B, Genç H, et al. Cycling progressive resistance training for people with multiple sclerosis: a randomized controlled study. Am J Phys Med Rehabil. 2010;89:446–457.







