Publication
Research Article
International Journal of MS Care
Nursing Interventions Focusing on Self-efficacy for Patients With Multiple Sclerosis in Rehabilitation: A Systematic Review
Author(s):
CE INFORMATION
ACTIVITY AVAILABLE ONLINE: To access the article and evaluation online, go to https://www.highmarksce.com/mscare.
TARGET AUDIENCE: The target audience for this activity is nursing professionals, advanced practice clinicians, physicians, rehabilitation professionals, mental health professionals, social workers, and other health care providers involved in the management of patients with multiple sclerosis (MS).
LEARNING OBJECTIVES:
Distinguish between the concepts of self-management and self-efficacy and effectively apply them in the promotion of rehabilitation care for patients with MS.
Select best instruments to measure patients’ self-management skills which can improve selection of intervention factors (theory, satisfaction, duration) necessary in the development and refinement of effective self-management interventions.
ACCREDITATION:

In support of improving patient care, this activity has been planned and implemented by the Consortium of Multiple Sclerosis Centers (CMSC) and Intellisphere, LLC. The CMSC is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the health care team.

This activity was planned by and for the healthcare team, and learners will receive .5 Interprofessional Continuing Education (IPCE) credit for learning and change.
NURSES: The CMSC designates this enduring material for .5 contact hour of nursing continuing professional development (NCPD) (none in the area of pharmacology).
PHYSICIANS: The CMSC designates this journal-based activity for a maximum of .5 AMA PRA Category 1 Credit(s) ™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
PSYCHOLOGISTS: This activity is awarded .5 CE credits.
SOCIAL WORKERS: As a Jointly Accredited Organization, the CMSC is approved to offer social work continuing education by the Association of Social Work Boards (ASWB) Approved Continuing Education (ACE) program. Organizations, not individual courses, are approved under this program. State and provincial regulatory boards have the final authority to determine whether an individual course may be accepted for continuing education credit. The CMSC maintains responsibility for this course. Social workers completing this course receive .5 continuing education credits.
DISCLOSURES: It is the policy of the Consortium of Multiple Sclerosis Centers to mitigate all relevant financial disclosures from planners, faculty, and other persons that can affect the content of this CE activity. For this activity, all relevant disclosures have been mitigated.
Francois Bethoux, MD, editor in chief of the International Journal of MS Care (IJMSC), and planner for this activity has disclosed no relevant financial relationships. Alissa Mary Willis, MD, associate editor of IJMSC, has disclosed no relevant financial relationships. Authors Rouven Brenner, MScN; Verena Witzig-Brändli, MScN; Janine Vetsch, PhD; and Myrta Kohler, PhD, have disclosed no relevant financial relationships.
The staff at IJMSC, CMSC, and Intellisphere, LLC who are in a position to influence content have disclosed no relevant financial relationships. Laurie Scudder, DNP, NP, continuing education director CMSC, has served as a planner and reviewer for this activity. She has disclosed no relevant financial relationships.
METHOD OF PARTICIPATION:
Release Date: July 1, 2022; Valid for Credit through: July 1, 2023
In order to receive CE credit, participants must:
1) Review the continuing education information, including learning objectives and author disclosures.
2) Study the educational content.
3) Complete the posttest and evaluation, which are available at https://www.highmarksce.com/mscare.
Statements of Credit are awarded upon successful completion of the evaluation. There is no fee to participate in this activity.
DISCLOSURE OF UNLABELED USE: This educational activity may contain discussion of published and/or investigational uses of agents that are not approved by the FDA. The CMSC and Intellisphere, LLC do not recommend the use of any agent outside of the labeled indications. The opinions expressed in the educational activity are those of the faculty and do not necessarily represent the views of the CMSC or Intellisphere, LLC.
DISCLAIMER: Participants have an implied responsibility to use the newly acquired information to enhance patient outcomes and their own professional development. The information presented in this activity is not meant to serve as a guideline for patient management. Any medications, diagnostic procedures, or treatments discussed in this publication should not be used by clinicians or other health care professionals without first evaluating their patients’ conditions, considering possible contraindications or risks, reviewing any applicable manufacturer’s product information, and comparing any therapeutic approach with the recommendations of other authorities.
ABSTRACT
BACKGROUND:
Rehabilitative nursing interventions are vital in the treatment of multiple sclerosis (MS), but there is a lack of evidence on the effectiveness of such interventions. This review aims to summarize outcomes of nurse-led rehabilitation interventions for patients with MS, focusing on patients' self-efficacy and self-management and their satisfaction with the intervention. This review is the first step of our overarching goal of developing, implementing, and evaluating a research-supported nursing consultation intervention in inpatient rehabilitation.
METHODS:
We searched 3 databases from their dates of inception until April 2020 (and performed another search in August 2021) for studies involving adult patients diagnosed as having MS. We focused on studies with interventions aimed at self-efficacy and self-management of MS and studies on intervention satisfaction. We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
RESULTS:
We included 4 studies in this review with a total of 271 participants. All interventions were educational and included training programs. All studies assessed self-efficacy, and all identified an improvement in self-efficacy, particularly through group training interventions. One study focused on self-management, reporting an improvement resulting from the intervention. Two studies evaluating satisfaction with the intervention obtained good overall satisfaction scores from participants, and 1 study's program was strongly recommended by participants.
CONCLUSIONS:
This review indicates that self-efficacy and self-management abilities may be effectively promoted, particularly through group training interventions. An intervention tailored and adapted to the needs of patients with MS may promote satisfaction with the intervention and might consequently improve adherence to rehabilitation interventions.
Multiple sclerosis (MS) is a demyelinating, chronic, inflammatory disease of the central nervous system, and it is the leading cause of disability in young and middle-aged adults in the developed world.1 It has an unpredictable disease course and can be classified into different patterns with different prevalence rates.2,3 Globally, MS affected approximately 2.8 million people in 2020, and incidence and prevalence rates are increasing4 due to longer life expectancy and an increased average age because of medical advancements in MS treatment5 and management of the superimposed comorbidities often diagnosed in patients with MS.6 Structured, multidisciplinary rehabilitation programs are essential to address symptom burden and disability associated with the disease and its comorbidities.2,7
The World Health Organization defines rehabilitation as “a set of interventions designed to optimize functioning and reduce disability in individuals with health conditions in interaction with their environment.”8 Rehabilitation thus aims to improve functional independence and increase participation through promotion of self-management abilities.9,10
The International Classification of Functioning, Disability and Health, a World Health Organization conceptual framework, offers a common approach to describe patients’ health conditions and health-related domains, such as bodily functions, activities, and participation.11 Not only does it describe body, individual, and societal perspectives, it also lists environmental factors that interact with all these components.11 Self-management and self-efficacy are key factors in the domains of participation (eg, in work, family) and activities (eg, self-care, daily routines).2,11 Based on the International Classification of Functioning, Disability and Health model, the desired outcome for rehabilitation is improved functional independence and enhanced participation in society. This can be achieved by emphasizing patient education and self-management.2,10,12
Rehabilitation of individuals with MS often requires repeated inpatient stays in specialized rehabilitation clinics with 24-hour care.2 However, depending on the needs of the individuals, rehabilitation may be accessed in outpatient clinics.13 There are also international differences between patients with MS being inpatients or outpatients. In the western part of Europe, patients with MS are more likely to be treated in outpatient settings, and in the eastern part more inpatient rehabilitation services are available.14 Regardless of the setting, nurses are key players in the multidisciplinary rehabilitation team and are part of all aspects of the rehabilitation process. Due to their continuous, robust patient relationships and their 24/7 presence, they have the best insight into patients’ situations.15 For example, nurses can detect changes in a patient’s state of health immediately and initiate appropriate interventions. Or, as nurses gain more in-depth patient information, they can support their self-management in a patient-centered way to maintain holistic care15,16 and continuity of care.15 In the outpatient setting, nurses assist patients in making the transition from the perspective of their disease needs in a clinical context to integrating those disease needs into their daily lives.17 This was recently highlighted by the Association of Rehabilitation Nurses in a competency model for professional rehabilitation nursing. One of the model’s 4 main domains is promotion of successful patient living, which includes fostering their ability to live independently at home or in a community living situation.18 Self-management is “the individual’s ability to manage the symptoms, treatment, physical and psychosocial consequences and lifestyle changes inherent in living with a chronic condition.”19 Self-management interventions are an important part of the rehabilitation process and are seen as key to active and effective disease management, especially after inpatient rehabilitation stays.20,21 A Cochrane review demonstrated that multidisciplinary inpatient rehabilitation leads to short-term gains for patients with MS; however, there was no evidence of long-term gains.2 Data about the successful implementation of self-management interventions into daily routines to achieve long-term behavior change are limited. A small study demonstrated that patients with MS in an outpatient setting had significantly higher self-efficacy for health promotion activities than the control group after an 8-week multidisciplinary health promotion education intervention.22 Another study in an outpatient setting found increased self-efficacy after 5 cognitive behavioral group sessions. The study group demonstrated a significant increase in self-efficacy after the intervention compared with the control group.23 However, these interventions were delivered by different health care professionals.
According to Bandura, successful self-management interventions that support a patient’s ability to change the way they live with a chronic condition require an underlying mechanism of self-efficacy.24–26 Self-efficacy is defined as a person’s belief in their ability to succeed in a particular situation.26 Translated to the rehabilitation of individuals with MS, self-efficacy describes how confident an individual with MS feels when implementing self-management interventions in their daily routine. Self-efficacy is a crucial psychological factor that reflects a patient’s confidence in managing their disease and is a strong predictor of self-management abilities.27,28
Previous studies with nursing interventions reported positive effects on self-efficacy and/or self-management in patients with neurologic29 and vascular30 diseases, diabetes,31 and hypertension.32 Evidence of effective interventions to increase self-efficacy and self-management is also available for patients with MS. However, these interventions were performed by health professionals,33,34 and, if they were implemented by nurses, they did not occur in the rehabilitative setting.35 Therefore, little is known about the effectiveness of nursing interventions focusing on self-efficacy and self-management of rehabilitation patients with MS.
Besides the summative outcomes of self-efficacy and self-management, satisfaction with the intervention is an important process outcome. Only when patients accept an intervention are they willing to use it continously.36 Understanding patient satisfaction with an intervention at an early stage will enhance the understanding of successful intervention implementation.36 Therefore, we focus on patient satisfaction with the intervention in this review, too.
This review is the first step of our overarching goal of developing, evaluating, and implementing a research-supported nursing consultation intervention using the Medical Research Council (MRC) framework.37 This intervention aims to continuously improve the self-efficacy and disease self-management abilities of individuals with MS through continuous contact with rehabilitation nurses regardless of inpatient or outpatient status. The renowned MRC framework will support the development process of this complex intervention. This intervention is considered complex because it has different interacting components (continuous nurse-patient relationship, self-management goal setting, etc). The intervention targets various patient-centered self-management behaviors based on the individual patient’s goals. Due to the patient-centered self-management goals, this intervention must be quite adaptive.37 The systematic review of research evidence in the development phase of an intervention is a main part of the MRC framework. A systematic review supports the identification of existing interventions to understand the evidence base.38,39 Therefore, this review summarizes the outcomes of nurse-led rehabilitation interventions focusing on the individual with MS’s self-efficacy and self-management and their satisfaction with the intervention.
METHODS
Systematic Literature Review Design
We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)40 for this systematic review.
Data Collection
Databases
We used a search string to search MEDLINE (via PubMed), the Cumulative Index to Nursing and Allied Health Literature, and the Cochrane Library from their inception through April 15, 2020. These databases were seen as the optimal combination to identify all relevant studies answering the research question.41 Two authors also handsearched Google Scholar (R.B., J.V.) using different search terms and screened the first 10 pages to identify any studies answering the research question that are not indexed in the databases. As a supplementary search method, we screened all reference lists of included studies to identify additional articles. The database searches were repeated on August 3, 2021, but no additional relevant studies were identified.
Search Strategy
The search strategy was developed by 3 of us (R.B., J.V., M.K.) and was adapted according to the requirements of each database (see TABLES S1 and S2, which are published in the online version of this article at IJMSC.org). The search was built with 4 main components: nursing, specific outcomes according to the study aims, MS, and rehabilitation. We used Medical Subject Headings where appropriate and free-text terms.
Screening
After duplicate article removal, 2 of us (R.B., J.V.) independently screened titles and abstracts for their eligibility using Rayyan (a free web and mobile app).42 The same authors independently screened the articles included for full-text screening. If consensus was not met, a third author (M.K.) was consulted. We retrieved all full texts and stored them using reference management software (Citavi; Swiss Academic Software GmbH).
Inclusion and Exclusion Criteria
All German- or English-language articles that focused on interventions to improve self-efficacy, self-management, and patient satisfaction in patients diagnosed as having MS who were older than 18 years were included. Studies with nursing interventions or interventions that could be performed by registered nurses (ie, educational interventions, counseling, or consultations) in inpatient and outpatient settings were included. We defined nursing interventions according to the National Institutes of Health guidelines for the systematic and progressive testing of nursing interventions.43 We included quantitative studies and mixed-method studies and excluded qualitative studies.
Data Extraction and Critical Appraisal
Two of us (R.B., V.W.) independently extracted the following data: author, year, country, study design, setting, participants, participants’ sociodemographic characteristics, intervention description (randomization, frequency, time point, etc), measurements, primary and secondary outcome measures, and primary and secondary outcome results related to study aims.
We used the Joanna Briggs Institute critical appraisal tools for quasi-experimental studies44 and qualitative research45 (qualitative part of any mixed-methods studies). Two of us (R.B., V.W.) independently assessed the quality of each article. Each item was judged with “yes,” “no,” or “unclear.” Any disagreements between reviewers were discussed and resolved by consensus. If consensus was not possible, a third author (M.K.) was integrated to reach a consensus. We did not exclude any study based on its quality.
The risk of bias was covered by questions in the Joanna Briggs Institute critical appraisal tools. These questions addressed selection bias (ie, similarity of participants), performance bias (ie, similarity of treatment of participants), attrition bias (ie, completeness of follow-up), detection bias (ie, equality of outcome measures across participants), and reporting bias (ie, reporting of all outcomes measured).
Synthesis
After the data were gathered, they were synthesized using an integrative approach, a narrative summary was written, and the findings were grouped according to the outcomes of interest related to the objectives of the review (ie, self-efficacy, self-management, and satisfaction with the intervention).
RESULTS
Description of Studies
After identifying 846 studies, we removed 77 duplicates (9%) and screened all remaining 769 studies. After screening titles and abstracts against the review’s inclusion criteria, 86 studies (11%) were eligible for full-text screening. Of those, 4 were included in the review (FIGURE S1).40
Critical Appraisal
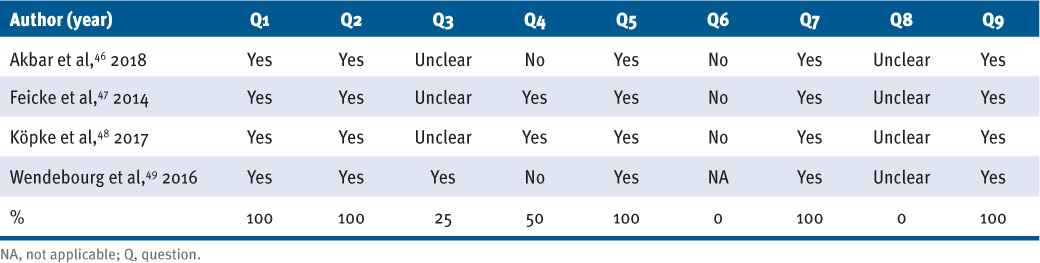
All included studies achieved a “Yes” of at least 50%. All the studies’ investigators described their inclusion criteria for the participants, and the groups were comparable at baseline. In addition, several outcome measures were used in all the studies before and after the intervention.46–49 Half of the studies had a control group.47,48 All of the studies completed some follow-up, but no studies completed or described any actions taken to reduce attrition rates.46–49 All results were measured comparably, but detailed information on the measures used was missing. All included studies used appropriate statistical analysis to calculate their results (TABLE 1).46–49
Critical Appraisal of the Included Studies
Risk of Bias
All assessed studies had a low risk of selection, detection, and reporting bias.46–49 The performance bias was unclear in 3 studies.46–48 However, according to the Cochrane Handbook, it may be possible to consider that risk of bias as low rather than high.50 For the 3 applicable studies, the risk of attrition bias was high (Table 1).46–48
Data Synthesis
In total, 271 patients with MS (203 female, 68 male) were included in the 4 studies. The mean ± SD patient age was 48.2 ± 7.9 years. The included studies were conducted in different settings: 1 inpatient study,48 1 outpatient study,46 and 2 studies with a mix of inpatients and outpatients.47,49 Two studies were conducted in rehabilitative settings.48,49 In the remaining 2 studies, rehabilitation is mentioned solely in the conclusion46 or in the description of the intervention.47
All 4 studies were published after 2014. One study was conducted in Canada46 and the other 3 were conducted in Germany.47–49 Three studies used a quasi-experimental design,47–49 and 1 used a mixed-methods design.46 Two studies combined quantitative data with qualitative data.46,49 One study used an adapted mixed-methods approach46 (TABLE 2).
Characteristics of the Included Studies
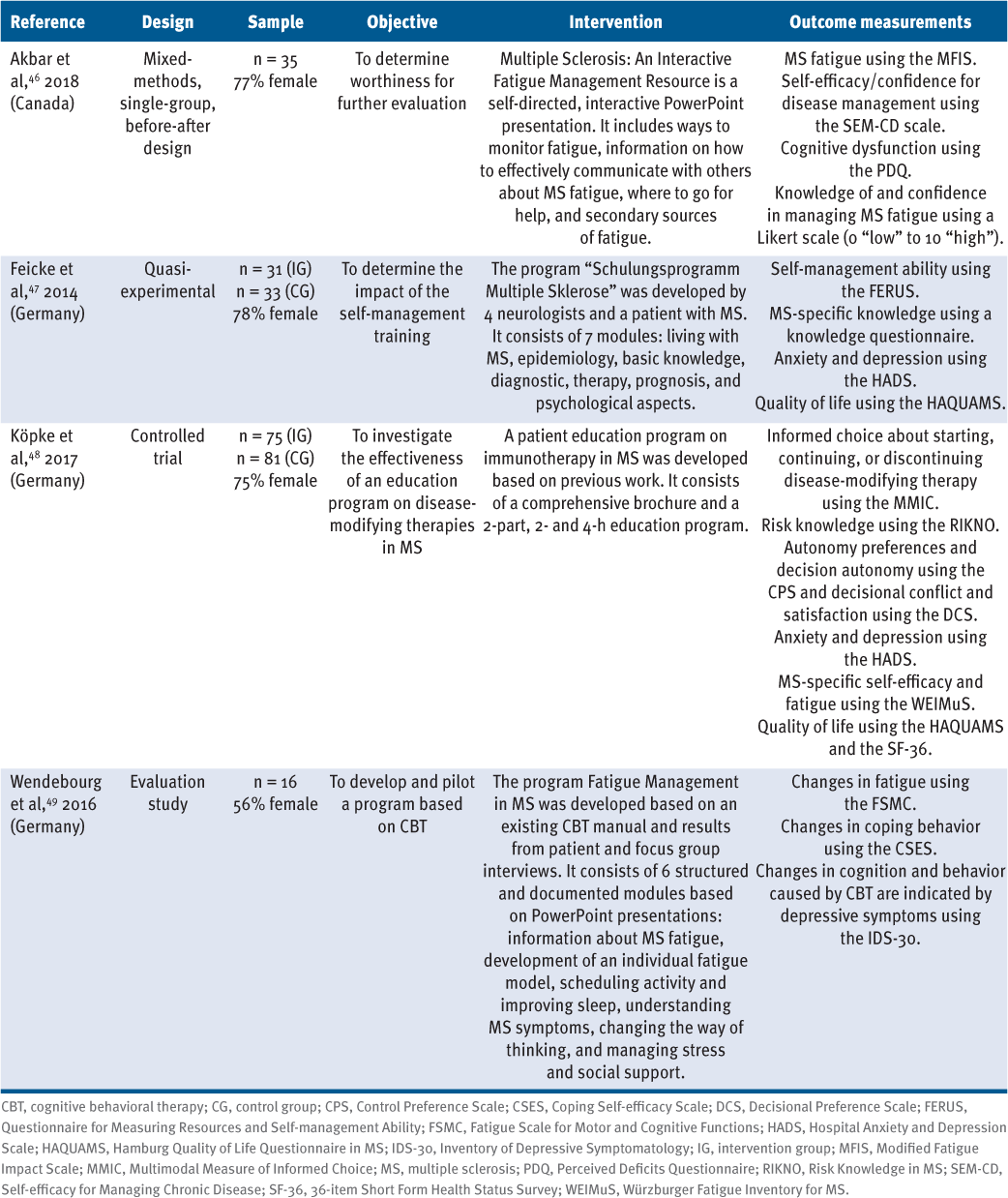
All interventions were educational and included training programs.46–49 Three of these training programs focused on MS management46,47,49 and 1 on a specific MS therapy.48 Two interventions involved training programs with PowerPoint presentations to improve the management of MS fatigue.46,49 One study reported that the intervention was performed by a nurse,48 another that the intervention was performed by a trained medical student,49 and the remaining 2 studies provided no information about the facilitator.46,47 One study focused on the self-management abilities of newly diagnosed patients with MS,47 and another on a training program about a disease-modifying therapy for patients with MS.48 Three studies with group training programs improved outcomes (ie, self-efficacy and self-management skills), although not statistically significantly in all cases.47–49
Intervention duration differed considerably among the studies (range, 41 minutes to 9 hours), with 1 study also showing a wide intrastudy range (range, 41–1545 minutes) because they had a self-directed, interactive intervention, used by the participants by their own volition.46 The 3 remaining interventions lasted 360 to 540 minutes.47–49
The 4 studies used 12 primary outcomes and 11 secondary outcomes. For 1 study, knowledge about MS itself, cognitive dysfunction, fatigue, and self-efficacy and confidence in disease management were primary outcomes.46 In 2 other studies, self-management ability, MS-specific knowledge,47 and informed choice about disease-modifying therapies48 were primary outcomes. The fourth study determined changes in fatigue, coping behavior, and cognition, and patient satisfaction with the program as primary outcomes.49 Two studies46,49 did not specify any secondary outcomes, whereas 1 study48 specified 9. Ten outcomes46–49 were related to managing disease (eg, confidence in disease management), and 5 of these outcomes were related to managing MS symptoms (eg, MS fatigue).46–49 Six measures were psychosocial outcomes (eg, cognitive dysfunction),46,48,49 and another 5 assessed educational outcomes (eg, MS-specific knowledge).46–48 Patient satisfaction with the program49 and quality of life47 were the remaining 2 study outcomes measured. All interventions had elements or principles from self-management promotion (eg, formation of a patient-provider partnership or shared decision-making).46–49
Self-efficacy
All 4 studies assessed various types of self-efficacy (ie, self-efficacy and confidence in managing MS fatigue, self-efficacy in coping, MS-specific self-efficacy, and self-efficacy as part of self-management); 3 studies46,48,49 focused on self-efficacy separately, and 1 study47 determined it in the context of other self-management abilities. Self-efficacy was measured in each of the studies using different assessment instruments. However, all self-efficacy measures were self-reported (the patient’s perception). The instruments used were the Self-efficacy for Managing Chronic Disease scale,46 the Coping Self-efficacy Scale,49 the Multiple Sclerosis Self-efficacy Scale,48 and the Questionnaire to Assess Resources and Self-management Skills (FERUS).47 The definition of self-efficacy varied among the studies. Self-efficacy was defined as control of MS symptoms (Multiple Sclerosis Self-efficacy Scale) and is seen as confidence in one’s ability to regularly complete tasks (Self-efficacy for Managing Chronic Disease scale), perform planned behaviors (FERUS), and cope with challenges and threats (Coping Self-efficacy Scale).
Two studies reported statistically significant improvement in self-efficacy from baseline to postintervention49 to follow-up at 6 months.47 These results were obtained for all but 1 participant49 or in all 5 subscales, including self-efficacy.47 The remaining 2 studies showed a nonsignificant change in score at follow-up after 3 months46 and slightly improved self-efficacy in the intervention group, which, however, was not stable 2 weeks after the intervention or at 6-month follow-up.48
Self-management
One of the included studies focused on several dimensions of self-management (ie, hope, coping, introspection, self-verbalization, and self-efficacy) and stated a statistically significant stable effect for total self-management ability and all dimensions of self-management abilities after the intervention. Self-management ability, as the total score of all related subscales of the FERUS, increased slightly across all 3 measurement points in the intervention group and decreased in the control group.47
Patient Satisfaction With the Intervention
Two studies evaluated the satisfaction of the patients with the training program.47,49 One of these studies47 used a validated questionnaire from a German university (ie, The Freiburg University of Education’s course evaluation survey), and the other study49 used a self-developed questionnaire from a pilot study for meta-cognitive training. Both instruments covered different aspects of the evaluation (ie, instructors’ didactic competence, course content and structure, recommendations for improvement) but also surveyed overall satisfaction with the program. The scores for this overall evaluation ranged from 1 (not at all true) to 5 (completely true)47 and from 1 (very good) to 6 (unsatisfactory).49 Both studies47,49 achieved the second highest mean score in patient satisfaction with the program, and participants in 1 of these studies47 would “strongly recommend” the program.
DISCUSSION
This review synthesized the evidence of nursing interventions in rehabilitation patients with MS, focusing on self-efficacy, self-management, and their satisfaction with the intervention. We found that nurse-led interventions, especially those consisting of group training, may improve self-efficacy and self-management abilities and lead to patient satisfaction. However, evidence on the effectiveness of nurse-led interventions in the rehabilitative setting remains limited.
The results suggest that the promotion of self-efficacy and self-management abilities is of considerable importance in the rehabilitative care of patients with MS.46–49 However, it needs to be acknowledged that it might be challenging to successfully integrate concepts such as self-efficacy into studies. Previous reviews also showed contrary findings for interventions in improving self-efficacy, which may indicate that self-efficacy is a difficult concept to define and measure in research.51,52 To conduct studies on improving self-efficacy, a particularly rigorous and stringent design needs to be used (eg, precise definitions of the outcomes and a focus on primary outcome measurements).53 The concept of self-efficacy was used in different contexts in the included studies (ie, self-efficacy in disease management,46 MS-specific self-efficacy,48 or self-efficacy in coping49), and, accordingly, was assessed using a different instrument in each study, which made comparison difficult. For future studies it would be helpful if researchers would restrict their selection of assessment tools to be able to compare results and merge data, such as in national cohort studies or registries (eg, the Swiss Multiple Sclerosis Registry54).
The 3 studies that conducted group training programs showed improvements in self-management abilities or self-efficacy,47–49 although this was statistically significant in only 2 studies. With several researchers emphasizing the importance of social support and peer support in self-management20,21,55 and with basic principles of self-efficacy theory, this suggests that self-efficacy can be fostered by vicarious experiences (ie, social role models) and social persuasions (ie, positive verbal feedback).26 These are all important factors to consider when promoting self-efficacy and self-management in patients with MS. In addition, patients’ family environments and their individual needs have to be considered throughout rehabilitation to provide tailored, individualized, participatory, and appreciative support.24,25 Despite nurses being a prime stakeholder to take over this role, no intervention in the included studies was designed as a nursing intervention,15 even though nurses are an important part of the multidisciplinary team in rehabilitation.2
Nursing in general and specifically in rehabilitation contains a high level of complexity due to the various interacting components, the presence of special problems, and situational instability.15,56 This is particularly applicable to the care of patients with MS.57,58 Nurses in rehabilitation are responsible for care, take charge of assessments, coordinate with other health care providers, and are responsible for internal and external communication. They establish a professional relationship with patients and their families, involve them in planning care, provide emotional support, and are an essential link between each inpatient stay.15,16 These actions are in line with the Association of Rehabilitation Nurses’s competency model. In the domain of “promotion of successful living,” nurses promote and facilitate safe and effective care transitions and foster patients’ self-management through coordinative and communicative competencies.18
However, the competency of nurses and the scope of nursing practice vary by country.59,60 The extent of any country’s nursing practices also reflects historical and current issues (shortages of nurses or physicians, etc).60 Due to the different understanding of the scope of practice and nursing competencies in different countries, nursing interventions require appropriate cultural adaptations. These variations challenge the ability to define a nursing intervention. Previously, some national and international efforts have been made to define rehabilitation care,61,62 but they lack acceptance or dissemination. Therefore, in our review, all the studies were included because they described interventions that could have potentially been nurse-led or performed in rehabilitation.
Strengths and Limitations
The key strength of this review is the participation of reviewers with proven expertise in rehabilitative care: 2 initially screened and reviewed articles independently, and 1 was on hand to produce consensus. Web-based software supported the reviewers in this process.
The main limitations of this systematic review were the low number of eligible studies and the lack of randomized controlled trials. As previously mentioned, the heterogeneity of the interventions, the outcome measurements, and the outcomes challenged the data synthesis. Another limitation is the restriction to 3 databases, although these were the most relevant with the most significant data sets. An equally limiting factor is that only studies in English and German were considered. Hence, substantially valuable content may have been missed. Another limitation of this review was a lack of focus on the contexts and specific features of the included interventions because we could not find this information in all included studies.
Conclusions
This review summarizes the existing studies of nursing interventions aimed at self-efficacy, self-management, and patient satisfaction with the intervention for rehabilitation patients with MS. This review indicates that self-efficacy and self-management abilities may be effectively promoted particularly by group training interventions. An intervention tailored to the needs of the patient promotes satisfaction with the intervention and might consequently improve adherence to the intervention. This finding underscores the need for developing, implementing, and evaluating nurse-led rehabilitation interventions tailored and adapted to the needs of patients with MS.
PRACTICE POINTS
» There is a need for the development, implementation, and evaluation of a nurse-led rehabilitation consultation for individuals with multiple sclerosis.
» This review indicates that self-efficacy and self-management abilities may be effectively promoted by group training interventions.
» We encourage rehabilitation nurses from around the world to develop and distribute a comprehensive and generally accepted definition of rehabilitation nursing.
ACKNOWLEDGEMENTS:
We thank Vanessa Gasser (Eastern Switzerland University of Applied Sciences, School of Health Professions) for useful discussion and her support in the data extraction.
References
Dobson R, Giovannoni G. Multiple sclerosis: a review. Eur J Neurol. 2019;26(1):27–40. doi: 10.1111/ene.13819
Amatya B, Khan F, Galea M. Rehabilitation for people with multiple sclerosis: an overview of Cochrane Reviews. Cochrane Database Syst Rev. 2019;1(1):CD012732. doi: 10.1002/14651858.CD012732.pub2
Amatya B, Young J, Khan F. Non-pharmacological interventions for chronic pain in multiple sclerosis. Cochrane Database Syst Rev. 2018;12(12):CD012622. doi: 10.1002/14651858.CD012622.pub2
Walton C, King R, Rechtman L, . Rising prevalence of multiple sclerosis worldwide: insights from the Atlas of MS, third edition. Mult Scler. 2020;26(14):1816–1821. doi: 10.1177/1352458520970841
Palmer AJ, van der Mei I, Taylor BV, Clarke PM, Simpson S Jr, Ahmad H. Modelling the impact of multiple sclerosis on life expectancy, quality-adjusted life years and total lifetime costs: evidence from Australia. Mult Scler. 2020;26(4):411–420. doi: 10.1177/1352458519831213
Sanai SA, Saini V, Benedict RH, . Aging and multiple sclerosis. Mult Scler. 2016;22(6):717–725. doi: 10.1177/1352458516634871
University of California, San Francisco MS-EPIC Team; Cree BA, Gourraud PA, Oksenberg JR, . Long-term evolution of multiple sclerosis disability in the treatment era. Ann Neurol. 2016;80(4):499–510. doi: 10.1002/ana.24747
World Health Organization. World Report on Disability 2011. World Health Organization; 2011.
Khan F, Amatya B, Kesselring J, Galea M. Telerehabilitation for persons with multiple sclerosis. Cochrane Database Syst Rev. 2015;2015(4):CD010508. doi: 10.1002/14651858.CD010508.pub2
Beer S, Khan F, Kesselring J. Rehabilitation interventions in multiple sclerosis: an overview. J Neurol. 2012;259(9):1994–2008. doi: 10.1007/s00415-012-6577-4
World Health Organization. Towards a common language for functioning, disability and health: ICF. Published 2002. Accessed April 5, 2022. https://cdn.who.int/media/docs/default-source/classification/icf/icfbeginnersguide.pdf?sfvrsn=eead63d3_4&download=true
World Health Organization. World Health Organization (WHO) International Classification of Functioning, Disability and Health (ICF). https://icd.who.int/dev11/l-icf/en
Tacchino A, Brichetto G, Zaratin P, Battaglia MA, Ponzio M. Multiple sclerosis and rehabilitation: an overview of the different rehabilitation settings. Neurol Sci. 2017;38(12):2131–2138. doi: 10.1007/s10072-017-3110-7
Rasova K, Freeman J, Martinkova P, . The organisation of physiotherapy for people with multiple sclerosis across Europe: a multicentre questionnaire survey. BMC Health Serv Res. 2016;16(1):552. doi: 10.1186/s12913-016-1750-6
Gutenbrunner C, Stievano A, Nugraha B, Stewart D, Catton H. Nursing: a core element of rehabilitation. Int Nurs Rev. 2022;69(1):13–19. doi: 10.1111/inr.12661
Gallien P, Gich J, Sánchez-Dalmau BF, Feneberg W. Multidisciplinary management of multiple sclerosis symptoms. Eur Neurol. 2014;72(suppl 1):20–25. doi: 10.1159/000367620
Schulman-Green D, Jaser S, Martin F, . Processes of self-management in chronic illness. J Nurs Scholarsh. 2012;44(2):136–144. doi: 10.1111/j.1547-5069.2012.01444.x
Vaughn S, Mauk KL, Jacelon CS, . The Competency Model for Professional Rehabilitation Nursing. Rehabil Nurs. 2016;41(1):33–44. doi: 10.1002/rnj.225
Barlow J. How to use education as an intervention in osteoarthritis. Best Pract Res Clin Rheumatol. 2001;15(4):545–558. doi: 10.1053/berh.2001.0172
Ghahari S, Forwell SJ, Suto MJ, Morassaei S. Multiple sclerosis self-management model: personal and contextual requirements for successful self-management. Patient Educ Couns. 2019;102(5):1013–1020. doi: 10.1016/j.pec.2018.12.028
Kidd T, Carey N, Mold F, . A systematic review of the effectiveness of self-management interventions in people with multiple sclerosis at improving depression, anxiety and quality of life. PLoS One. 2017;12(10):e0185931. doi: 10.1371/journal.pone.0185931
Ennis M, Thain J, Boggild M, Baker GA, Young CA. A randomized controlled trial of a health promotion education programme for people with multiple sclerosis. Clin Rehabil. 2006;20(9):783–792. doi: 10.1177/0269215506070805
Graziano F, Calandri E, Borghi M, Bonino S. The effects of a group-based cognitive behavioral therapy on people with multiple sclerosis: a randomized controlled trial. Clin Rehabil. 2014;28(3):264–274. doi: 10.1177/0269215513501525
Lorig KR, Holman H. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med. 2003;26(1):1–7. doi: 10.1207/S15324796ABM2601_01
Battersby M, Von Korff M, Schaefer J, . Twelve evidence-based principles for implementing self-management support in primary care. Jt Comm J Qual Patient Saf. 2010;36(12):561–570. doi: 10.1016/s1553-7250(10)36084-3
Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215. doi: 10.1037//0033-295x.84.2.191
Yao J, Wang H, Yin X, Yin J, Guo X, Sun Q. The association between self-efficacy and self-management behaviors among Chinese patients with type 2 diabetes. PLoS One. 2019;14(11):e0224869. doi: 10.1371/journal.pone.0224869
Wilski M, Kocur P, Brola W, Tasiemski T. Psychological factors associated with self-management in multiple sclerosis. Acta Neurol Scand. 2020;142(1):50–57. doi: 10.1111/ane.13236
Imhof L, Suter-Riederer S, Kesselring J. Effects of mobility-enhancing nursing intervention in patients with MS and stroke: randomised controlled trial. Int Sch Res Notices. 2015;2015:785497. doi: 10.1155/2015/785497
Sol BG, van der Graaf Y, van der Bijl JJ, Goessens NB, Visseren FL. Self-efficacy in patients with clinical manifestations of vascular diseases. Patient Educ Couns. 2006;61(3):443–448. doi: 10.1016/j.pec.2005.05.011
Subramanian SC, Porkodi A, Akila P. Effectiveness of nurse-led intervention on self-management, self-efficacy and blood glucose level among patients with type 2 diabetes mellitus. J Complement Integr Med. 2020;17(3). doi: 10.1515/jcim-2019-0064
Savadkooh OK, Zakerimoghadam M, Gheyasvandian G, Kazemnejad A. A survey of the effect of a self-management program on self-efficacy and control of disease in hypertensive patients. J Mazandaran Univ Med Sci. 2012;22:19–28.
Hersche R, Weise A, Michel G, Kesselring J, Barbero M, Kool J. Development and preliminary evaluation of a 3-week inpatient energy management education program for people with multiple sclerosis-related fatigue. Int J MS Care. 2019;21(6):265–274. doi: 10.7224/1537-2073.2018-058
Mulligan H, Wilkinson A, Barclay A, Whiting H, Heynike C, Snowdon J. Evaluation of a fatigue self-management program for people with multiple sclerosis. Int J MS Care. 2016;18(3):116–121. doi: 10.7224/1537-2073.2015-019
Hemmati Maslakpak M, Raiesi Z. Effect of a self-management and follow-up program on self-efficacy in patients with multiple sclerosis: a randomized clinical trial. Nurs Midwifery Stud. 2014;3(4):e25661. doi: 10.17795/nmsjournal25661
Proctor E, Silmere H, Raghavan R, . Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health. 2011;38(2):65–76. doi: 10.1007/s10488-010-0319-7
Skivington K, Matthews L, Simpson SA, . A new framework for developing and evaluating complex interventions: update of Medical Research Council guidance. BMJ. 2021;374:n2061. doi: 10.1136/bmj.n2061
O’Cathain A, Croot L, Duncan E, . Guidance on how to develop complex interventions to improve health and healthcare. BMJ Open. 2019;9(8):e029954. doi: 10.1136/bmjopen-2019-029954
Skivington K, Matthews L, Simpson SA, . Framework for the development and evaluation of complex interventions: gap analysis, workshop and consultation-informed update. Health Technol Assess. 2021;25(57):1–132. doi: 10.3310/hta25570
Page MJ, Moher D, Bossuyt PM, . PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372:n160. doi: 10.1136/bmj.n160
Nordhausen T, Hir t J. Manual zur Literaturrecherche in Fachdatenbanken. In: Ref Hunter, Version 5 . 2020:5.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan: a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210. doi: 10.1186/s13643-016-0384-4
Whittemore R, Grey M. The systematic development of nursing interventions. J Nurs Scholarsh. 2002;34(2):115–120. doi: 10.1111/j.1547-5069.2002.00115.x
Tufanaru C, Munn Z, Aromataris E, Campbell J, Hopp L. Systematic reviews of effectiveness. In: Aromataris E, Munn Z, eds. JBI Manual for Evidence Synthesis . Joanna Briggs Institute; 2020.
Lockwood C, Munn Z, Porritt K. Qualitative research synthesis: methodological guidance for systematic reviewers utilizing meta-aggregation. Int J Evid Based Healthc. 2015;13(3):179–187. doi: 10.1097/XEB.0000000000000062
Akbar N, Turpin K, Petrin J, Smyth P, Finlayson M. A pilot mixed-methods evaluation of MS INFoRm: a self-directed fatigue management resource for individuals with multiple sclerosis. Int J Rehabil Res. 2018;41(2):114–121. doi: 10.1097/MRR.0000000000000271
Feicke J, Spörhase U, Köhler J, Busch C, Wirtz M. A multicenter, prospective, quasi-experimental evaluation study of a patient education program to foster multiple sclerosis self-management competencies. Patient Educ Couns. 2014;97(3):361–369. doi: 10.1016/j.pec.2014.09.005
Köpke S, Kasper J, Flachenecker P, . Patient education programme on immunotherapy in multiple sclerosis (PEPIMS): a controlled rater-blinded study. Clin Rehabil. 2017;31(2):250–261. doi: 10.1177/0269215516639734
Wendebourg MJ, Feddersen LK, Lau S, . Development and feasibility of an evidence-based patient education program for managing fatigue in multiple sclerosis: the “Fatigue Management in MS” Program (FatiMa). Int J MS Care. 2016;18(3):129–137. doi: 10.7224/1537-2073.2014-105
Higgins JPT, Thomas J, Chandler J, . Cochrane Handbook for Systematic Reviews of Interventions . John Wiley & Sons; 2019.
Franek J. Self-management support interventions for persons with chronic disease: an evidence-based analysis. Ont Health Technol Assess Ser. 2013;13(9):1–60.
Kuspinar A, Rodriguez AM, Mayo NE. The effects of clinical interventions on health-related quality of life in multiple sclerosis: a meta-analysis. Mult Scler. 2012;18(12):1686–1704. doi: 10.1177/1352458512445201
Rae-Grant AD, Turner AP, Sloan A, Miller D, Hunziker J, Haselkorn JK. Self-management in neurological disorders: systematic review of the literature and potential interventions in multiple sclerosis care. J Rehabil Res Dev. 2011;48(9):1087–1100. doi: 10.1682/jrrd.2010.08.0159
Steinemann N, Kuhle J, Calabrese P, . The Swiss Multiple Sclerosis Registry (SMSR): study protocol of a participatory, nationwide registry to promote epidemiological and patientcentered MS research. BMC Neurol. 2018;18(1):111. doi: 10.1186/s12883-018-1118-0
Learmonth YC, Motl RW. Physical activity and exercise training in multiple sclerosis: a review and content analysis of qualitative research identifying perceived determinants and consequences. Disabil Rehabil. 2016;38(13):1227–1242. doi: 10.3109/09638288.2015.1077397
Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. Int J Nurs Stud. 2013;50(5):587–592. doi: 10.1016/j.ijnurstu.2012.09.010.
Soelberg Sorensen P, Giovannoni G, Montalban X, Thalheim C, Zaratin P, Comi G. The multiple sclerosis care unit. Mult Scler. 2019;25(5):627–636. doi: 10.1177/1352458518807082
Péloquin S, Schmierer K, Leist TP, Oh J, Murray S, Lazure P. Challenges in multiple sclerosis care: results from an international mixed-methods study. Mult Scler Relat Disord. 2021;50:102854. doi: 10.1016/j.msard.2021.102854
Maier CB, Barnes H, Aiken LH, Busse R. Descriptive, cross-country analysis of the nurse practitioner workforce in six countries: size, growth, physician substitution potential. BMJ Open. 2016;6(9):e011901. doi: 10.1136/bmjopen-2016-011901. Published correction appears in BMJ Open. 2016;6(9):e011901corr1.
Drennan VM, Ross F. Global nurse shortages: the facts, the impact and action for change. Br Med Bull. 2019;130(1):25–37. doi: 10.1093/bmb/ldz014.
Suter-Riederer S, Mahrer Imhof R, Gabriel C, Kesselring J, Schnepp W, Imhof L. Consenting on principles of rehabilitation nursing care: a Delphi Study. Rehabil Nurs. 2018;43(6):E35–E41. doi: 10.1097/rnj.0000000000000111
Pryor J, Smith C. A framework for the role of registered nurses in the specialty practice of rehabilitation nursing in Australia. J Adv Nurs. 2002;39(3):249–257. doi: 10.1046/j.1365-2648.2002.02271.x
FINANCIAL DISCLOSURES: The authors declare no conflicts of interest.
FUNDING/SUPPORT: The authors disclosed receipt of the following financial support for the research, authorship, and publication of this article: Swiss MS Society.







