Publication
Research Article
International Journal of MS Care
Interdisciplinary Treatment of Patients with Multiple Sclerosis and Chronic Pain
Author(s):
The objective of this study was to examine the efficacy of an interdisciplinary pain rehabilitation program in a multiple sclerosis (MS) population by evaluating changes in mood, pain, and functioning. This descriptive study examined 20 patients with chronic pain and MS who were admitted to the Cleveland Clinic's Chronic Pain Rehabilitation Program (CPRP) between 2000 and 2009. At both admission to and discharge from the CPRP, measures of pain, depression, and functioning were obtained using a pain visual analogue scale (VAS), the Beck Depression Inventory (BDI), the Depression Anxiety Stress Scale (DASS), and the Pain Disability Index (PDI). Outcomes for the MS patients were compared with those of patients without MS who had participated in the same program. The results showed that MS patients who completed the CPRP reported dramatic decreases in pain and depression and an increase in daily functioning. The benefits received by MS patients from the program were similar to those received by patients without MS. Thus programs like the CPRP can result in significant improvements in pain, depression, and functioning among people with MS.
Multiple sclerosis (MS) is a neurologic disease that affects the central nervous system (CNS). It can be a debilitating disorder with an array of painful physical and emotional symptoms. In addition, deterioration of executive and cognitive functioning often presents challenges for MS patients in their day-to-day lives. Physical or psychological pain has been reported to occur in 29% to 86% of individuals with MS.1 The large discrepancy across studies may be explained by different methodologies and classifications of pain. According to a 2004 study by Solaro et al.,1 studies usually classify pain symptoms according to temporal criteria rather than the World Health Organization pain treatment guidelines.2
The physical pain described by people with MS is often widespread, chronic, and debilitating. The types of physical pain associated with MS can vary depending on the area of the brain affected. In 2008, O'Connor et al.2 proposed four classifications of MS-related pain: 1) continuous central neuropathic pain, 2) intermittent central neuropathic pain, 3) musculoskeletal pain, and 4) mixed neuropathic and non-neuropathic pain. Central neuropathic pain, which is pain experienced in the absence of any psychiatric disorder or peripheral neuropathic pain, is consistent with a CNS lesion and may affect between 27.5% and 58% of MS patients.3 In addition, as reported by Ehde et al.,4 up to 44% of people with MS experience optic neuritis pain, with 20% reporting that this type of pain significantly affects daily living. Headache pain is more common within the MS population than in the general population, affecting approximately 55% of MS patients. Some researchers believe this may be a result of plaques in the brainstem or other locations.5 According to Maleki and Sullivan,6 a diagnosis of MS further complicates the treatment plans in patients with a pain disorder. Furthermore, little research has been conducted on the psychological aspects of pain in the MS population.
Pain is generally associated with psychological distress and decreased daily functioning, including in the areas of recreation, family responsibilities, self-care, and social activity.7 Depression is also a common response in individuals with MS and pain.8 9 A nationwide study conducted by the Centers for Disease Control and Prevention estimated the prevalence of depression among all adults aged 18 years and older to be between 8.9% and 9.4%.10 In large population studies of people with MS, the prevalence of major depression has varied between 26% and 51%.9 While some researchers propose that depression in MS is a result of experiencing a chronic debilitating disease, others suggest that depressive symptoms can be explained by neurologic damage to the CNS.9 Regardless of the cause of depression, it is known that people with MS report three- to four-fold higher levels of depression than the general population.
As with pain, the amount of disability varies greatly from person to person depending on the severity of their MS. The most common symptoms are weakness, balance problems, and fatigue. Other areas in which disability may manifest are sensory, cerebellar, brainstem, and visual function and bowel/bladder control.7 11
A variety of programs have been developed with the aim of improving the quality of life of patients with various health conditions. Interdisciplinary pain rehabilitation programs have been shown to reduce pain and improve mood and functioning in patients with chronic pain conditions. However, the literature contains no reports examining the efficacy of such an approach within the MS population. Therefore, this study was conducted to investigate the effectiveness of the Cleveland Clinic's 3- to 4-week Chronic Pain Rehabilitation Program (CPRP), specifically in reducing pain and depression and increasing perceived functioning in individuals with MS.
Methods
Patients
This descriptive study examined 20 patients with chronic pain and MS who were admitted to the Cleveland Clinic's CPRP between 2000 and 2009. A database approved by the Cleveland Clinic Institutional Review Board was used to conduct this retrospective chart review. A total of 2030 patients were admitted to the CPRP between 2000 and 2009, and patients were selected for the current study based on their receipt of a diagnosis of MS. Data for the non-MS patients in the program were used for comparison purposes.
Measurements
Pain
Pain was measured using a visual analogue scale (VAS) in which patients rated their pain from 0 to 10, with 0 indicating “no pain” and 10 indicating “very severe pain.” This measure was taken at both admission and discharge.
Depression
Depression was measured using either the Beck Depression Inventory (BDI) or the Depression Anxiety Stress Scale (DASS).12–14 The results were used to divide the patients into four categories: no depression, mild depression, moderate depression, and severe depression. The number of patients with each type of depression was recorded before and after completion of the program. According to Scheman et al.,14 the DASS and the BDI are comparable. The same scale was used for each individual participant at admission to and discharge from the program.
Functioning
In order to measure the impact of chronic pain on functioning in different aspects of their lives, patients were administered the Pain Disability Index (PDI) at the start and the completion of the program.15 The PDI consists of seven items, each representing a separate domain and measured on a scale from 0 to 10, with the total score ranging from 0 to 70. The domains are as follows: 1) family/home responsibilities, 2) recreation, 3) social activity, 4) occupation, 5) sexual behavior, 6) self-care, and 7) life-support activity. The PDI is not a measure of pain, but rather of the degree to which pain has become disabling. The higher the overall score, the greater the patient's perceived impact of pain on functioning.
Treatment/Procedure
The CPRP is an intensive outpatient program with many components thought to be important in managing pain and improving functioning. It is an interdisciplinary program that includes physical therapy, occupational therapy, group and individual psychotherapy, relaxation training and biofeedback, and medication management, including weaning from all opioids and benzodiazepines or other addictive substances. Each patient receives all services except for substance abuse counseling, which is provided as needed based on admission screening. Patients receive education on psychological and physical dependence on medications. Daily physical therapy sessions teach proper body mechanics and are intended to improve strength, flexibility, and endurance. Patients are instructed in managing pain through stress management, focusing on reducing muscle tension and nervous system arousal. Psychotherapy—which includes group therapy, individual therapy, couples therapy, and sexual dysfunction counseling—is provided to help teach patients how healthy interpersonal relations can reduce pain levels. Occupational therapy is used to improve performance on tasks at home and at work. It aims to reduce stress and give patients more confidence in performing daily activities as they relearn how to perform daily tasks. Instruction in proper body mechanics, which reduces muscle strain, also helps patients gain confidence in performing daily activities. Other services provided in the program include vocational counseling, medical/surgical consultations, anger management and assertiveness training, and behavior modification training. The average length of stay in the program among the 20 patients with MS was 16.7 days.
Results
Of the 20 MS patients who entered the CPRP between 2000 and 2009, a total of 17 completed the program and filled out discharge questionnaires. Three patients left the program against medical advice. Data analysis was conducted using SPSS (SPSS, Chicago, IL) to calculate mean values and percentages. Most data analyses had a within-subject design, comparing the findings of a given patient at admission with those of the same patient at discharge. Between-subjects testing was conducted to compare the results of MS patients with those of non-MS patients with pain.
Demographic Information
Among the 20 patients with MS who participated in the CPRP, the mean age at admission was 48.5 years, and the average age at the time of MS diagnosis was 35.2 years. There were 16 women and 4 men, reflecting the higher incidence of MS in women than in men. Of the participants, 17 (85%) were white and the remaining 3 were of other ethnicities.
In terms of MS classification, 12 patients had the relapsing-remitting type, 4 had the primary progressive type, and 4 had the secondary progressive type. The most common comorbid pain diagnosis was neuropathic pain (81%), followed by fibromyalgia (14.2%). Before entering the CPRP, the most common comorbid psychiatric diagnoses were depression and substance abuse (28.6% each), and 4 patients reported pain disorders with mixed psychological and physical factors (20%).
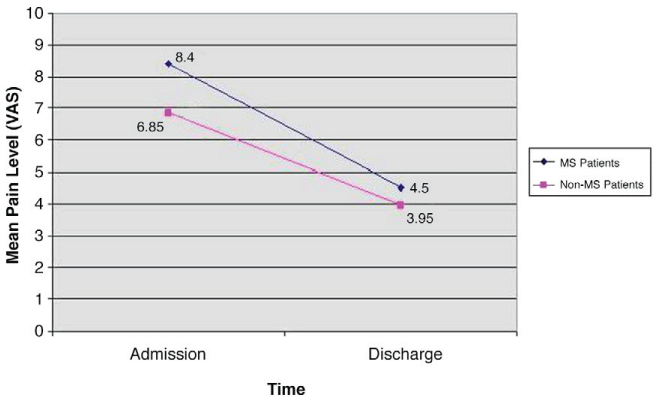
Pain
The average VAS pain rating for MS patients at admission was 8.40 (Figure 1). This score was higher than that of non-MS patients, who reported an average pain rating at admission of 6.85. At discharge, the average pain rating for MS patients had decreased to 4.50, while pain scores for non-MS patients decreased to 3.95. Thus, although MS patients were discharged from the program with higher pain ratings than non-MS patients, they still received a significant benefit in terms of pain reduction.
Mean pain level scores on a visual analogue scale (VAS) from admission to discharge in MS and non-MS patients
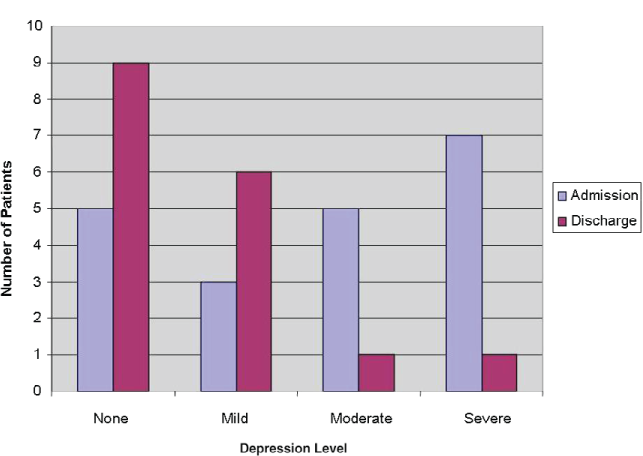
Depression
When MS patients were admitted to the CPRP, they were diagnosed with the following severities of depression: none (5), mild (3), moderate (5), severe (7). At discharge from the program, depression severities had changed to the following: none (9), mild (6), moderate (1), severe (1). Thus depression was reduced considerably by the program, with all but 2 patients having depression ratings of none or mild at discharge (Figure 2).
Depression severities of MS patients at admission and discharge
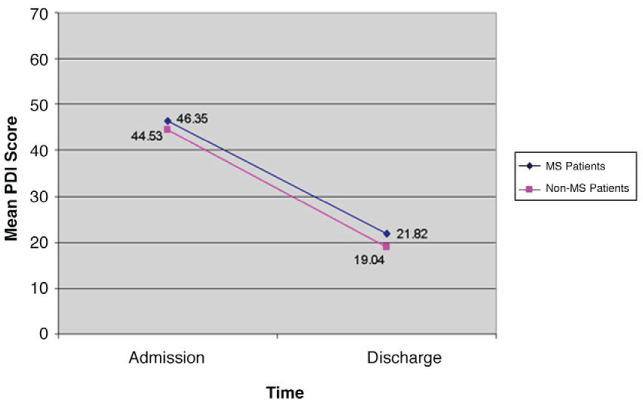
Functioning
At admission, MS patients had an average PDI score of 46.35, compared with 44.53 for non-MS patients (Figure 3). At discharge, MS patients had an average score of 21.82. Non-MS patients reported similarly decreased levels of perceived disability at discharge, with an average score of 19.04. These results indicate similar benefits from the CPRP for patients with and those without MS.
Mean Pain Disability Index (PDI) scores for MS and non-MS patients at admission and discharge
Discussion
Greater pain severity in patients with MS is associated with increased disability, female sex, increased age, unstable MS symptoms, lower educational level, longer duration of pain, and more health-care utilization.1 All of these factors are associated with the presence of depression. With nearly two-thirds of patients in our study reporting depressive symptoms, it is imperative to address both pain and depression in MS patients.9
Our data suggest that people with MS can benefit from participation in interdisciplinary pain rehabilitation programs like the Cleveland Clinic's CPRP. Although MS patients' pain and depression may differ from those of patients with other diseases, these conditions can be relieved. Reductions in pain and depression lead directly to improvements in day-to-day functioning. Using a multifaceted approach to treatment, therapists can teach patients how to overcome pain affecting various parts of their lives. For patients with severe functional and psychological impairments, effective treatment requires awareness of and attention to both physical and psychological factors involved in pain.6
This study has two limitations. Because of the small sample size, the data presented cannot easily be generalized to all MS patients. What this study does show, however, is that MS patients can show great improvements through participation in an already existing interdisciplinary program that is not tailored specifically to people with MS. We intend to continue recruiting patients to gain a larger sample that is more representative of the MS population. Many MS patients may not be referred to such a program by their physicians because of primary diagnoses in addition to chronic pain. Our hope is that this study will inform physicians and other providers about the efficacy of such programs.
The second limitation is that two different scales, the BDI and the DASS, were used to measure depression, although the same scale was used for each individual patient at admission and discharge. Ideally, the same depression scale would have been used for all patients throughout the entire study. The DASS was used to replace the BDI because of financial considerations, but because a high correlation between these inventories has been reported (correlation coefficient of 0.74),16 we believe the results would not have differed significantly had the same scale been used throughout. Thus our conclusions would have remained the same.
PracticePoints
People with MS often experience widespread, chronic, and debilitating physical pain.
Participation in chronic pain rehabilitation programs can result in significant improvements in pain, depression, and functioning among people with MS.
Both patients with and without MS benefit similarly from such programs.
Acknowledgments
We would like to thank the patients who were involved in this study.
References
Solaro C, Brichetto G, Amato MP, et al. The prevalence of pain in multiple sclerosis: a multicenter cross-sectional study. Neurology. 2004; 63: 919–921.
O'Connor AB, Schwid SR, Herrmann DN, et al. Pain associated with multiple sclerosis: systematic review and proposed classification. Pain. 2008; 137: 96–111.
Osterberg A, Boivie J, Thuomas KA. Central pain in multiple sclerosis: prevalence and clinical characteristics. Eur J Pain. 2005; 9: 531–542.
Ehde DM, Gibbons LE, Chwastiak L, et al. Chronic pain in a large community sample of persons with multiple sclerosis. Mult Scler. 2003; 9: 605–611.
Gee JR, Chang J, Dublin AB, Vijayan N. The association of brainstem lesions with migraine-like headache: an imaging study of multiple sclerosis. Headache 2005; 6: 670–677.
Maleki J, Sullivan A. Assessment and treatment of pain disorders in multiple sclerosis. In: Cohen JA, Rudick RA, eds. Multiple Sclerosis Therapeutics. 4th ed. New York, NY: Cambridge University Press; 2011:707–713.
Kratz A, Molton I, Jensen M, et al. Further evaluation of the motivational model of pain self-management: coping with chronic pain in multiple sclerosis. Ann Behav Med. 2011; 41: 391–400.
Nyenhuis DL, Rao SM, Zajecka JM, et al. Mood disturbance versus other symptoms of depression in multiple sclerosis. J Int Neuropsychol Soc. 1995; 1: 291–296.
Sadovnick AD, Remick RA, Allen J, et al. Depression and multiple sclerosis. Neurology. 1996; 46: 628–632.
Centers for Disease Control and Prevention. Current depression among adults—United States, 2006 and 2008 morbidity and mortality. 2010. http://www.cdc.gov/Features/dsDepression/. Accessed September 25, 2011.
Scalfari A, Neuhaus A, Degenhardt A, et al. The natural history of multiple sclerosis: a geographically based study 10: relapses and long-term disability. Brain. 2010; 133: 1914–1929.
Ng F, Trauer T, Dodd S, et al. The validity of the 21-item version of the Depression Anxiety Stress Scales as a routine outcome measure. Acta Neuropsychiatrica. 2011; 19: 304–310.
Corbière M, Bonneville-Roussy A, Franche R, et al. Further validation of the BDI-II among people with chronic pain originating from musculoskeletal disorders. Clin J Pain. 2011; 27: 62–69.
Scheman J, Janotta C, Covington E. Validity study of the Depression Anxiety Stress Scales in a sample of chronic pain patients. Poster presented at: 26th Annual Scientific Meeting of the American Pain Society, Washington, DC. J Pain. 2007;8.
Tait RC, Pollard CA, Margolis RB, et al. The Pain Disability Index: psychometric and validity data. Arch Phys Med Rehabil. 1987; 68: 438–441.
Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther. 1995; 33: 335–342.
Financial Disclosures: The authors have no conflicts of interest to disclose.







