Publication
Research Article
International Journal of MS Care
Summary of Eye Examinations of 284 Patients with Multiple Sclerosis
The aim of this article is to report the findings of ocular examinations in a group of patients diagnosed with multiple sclerosis who were referred to the eye department of the Nationaal Multiple Sclerosis Centrum of Melsbroek, Belgium, from 2007 to 2010. Patients were evaluated by a single examiner, who noted visual acuity for distance, the state of the optic disks, oculomotor balance, and the presence of nystagmus, uveitis, trigeminal neuralgia, and facial palsy. The sample consisted of 284 adults born between 1920 and 1989: 111 males and 173 females. There were 51 patients with a corrected visual acuity in the better-seeing eye of less than 6/20. The optic nerve head was found to be normal in 245 eyes. Nystagmus was noted in 104 patients. Diplopia at distance was found to be present in 20 males, of whom 12 also had nystagmus, and in 31 females, of whom 13 also had nystagmus. Oscillopsia was present in 6 males and 11 females. In summary, most of the patients evaluated had sufficient visual function to allow performance of activities of daily living without help. A small number of patients had visual failure due to dysfunction of the visual sensory pathway and/or disturbances of oculomotor balance, often of a supranuclear origin, resulting in considerable disability.
This article describes the findings of ocular examinations of patients who were referred to the eye department of the Nationaal Multiple Sclerosis Centrum of Melsbroek, Belgium, from 2007 to 2010. All of the examinations were performed by a single clinician (JMR). All of the patients were known to have experienced multiple neurologic deficits for some period of time before attending the multiple sclerosis (MS) clinic. The sample consisted of 284 adults: 111 males and 173 females. Only the findings of patients with a definite diagnosis of MS are reported.
Some patients were seen at the time of hospitalization for treatment of problems resulting from their disease. Other patients came from outside, often to obtain a certificate needed to get an official driver's license, to obtain a “certificate formule 5” (a certificate provided by an ophthalmologist to enable the individual to request public assistance because of a major visual handicap), or to seek other help that was not offered elsewhere. The main reason for consultation was to determine whether there were refractive errors that needed correction. Other reasons for consultation were headache, disturbing diplopia, suspected acute optic neuritis, blepharoconjunctivitis, evaluation of profound visual failure, diabetes mellitus, arterial hypertension, measurement of intraocular pressure, cataracts, nystagmus, uveitis, photophobia, anisocoria, and dry eye.
Patients were evaluated in the eye department and underwent a normal screening ophthalmologic examination. Particularly noted were visual acuity for distance, the state of the optic disks, oculomotor balance, and the presence of nystagmus, uveitis, trigeminal neuralgia, and facial palsy. The Expanded Disability Status Scale (EDSS; as established by Kurtzke) score was recorded for each patient. A score between 1 and 3 was assigned to 23 patients, a score between 4 and 6 was assigned to 110 patients, and a score between 7 and 9 was assigned to 151 patients.
Findings
Sample Characteristics
Patients were categorized according to gender and date of birth in 10-year ranges. They were also categorized according to their best visual acuity (Table 1). A total of 284 adults born between 1920 and 1989 participated in this study: 111 males and 173 females. The male group had a mean age of 54 years and a median age of 53.5 years. The female group had a mean age of 56 years and a median age of 55 years.
Gender and ocular examination results by age group
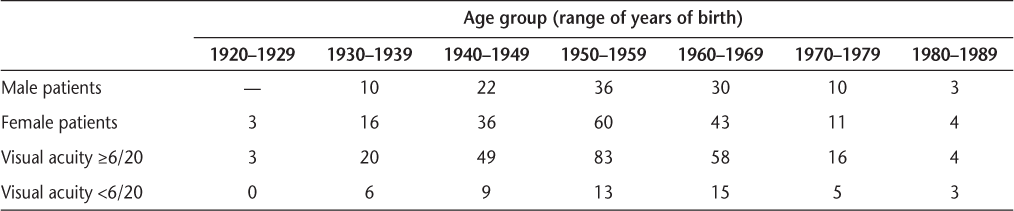
Visual Acuity
The findings concerning visual acuity are summarized in Table 1. The presence of functional low vision was defined as corrected visual acuity in the better-seeing eye of less than 6/20. There were 51 cases (24 males and 27 females) with functional visual loss. Most were born between 1940 and 1969. In the group with functional visual loss, there were 7 males and 9 females with corrected visual acuity in the better-seeing eye of less than the ability to count fingers at 2 meters.
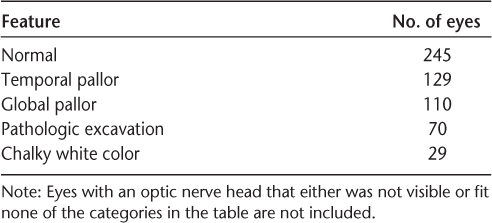
Changes of the Optic Nerve Head
The state of the optic nerve head (ONH) in 561 eyes of the 284 patients is summarized in Table 2. The ONH was found to be normal in 89 eyes in males and 156 eyes in females. A few eyes (not included in the table) had an ONH showing inferior pallor, and 2 eyes had an ONH showing drusen. In all eyes in this sample, the ONH had sharp borders.
State of the optic nerve head for patients in all age groups
Oculomotor Balance
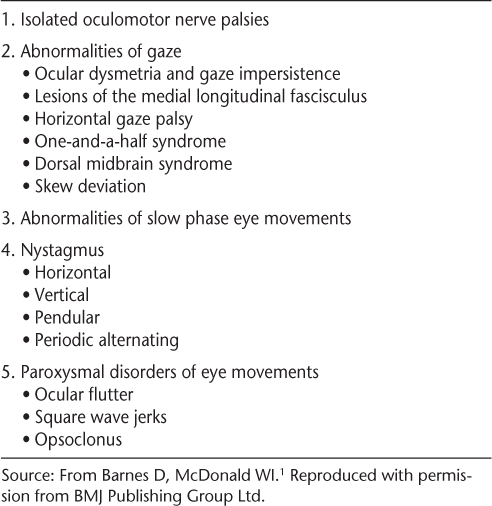
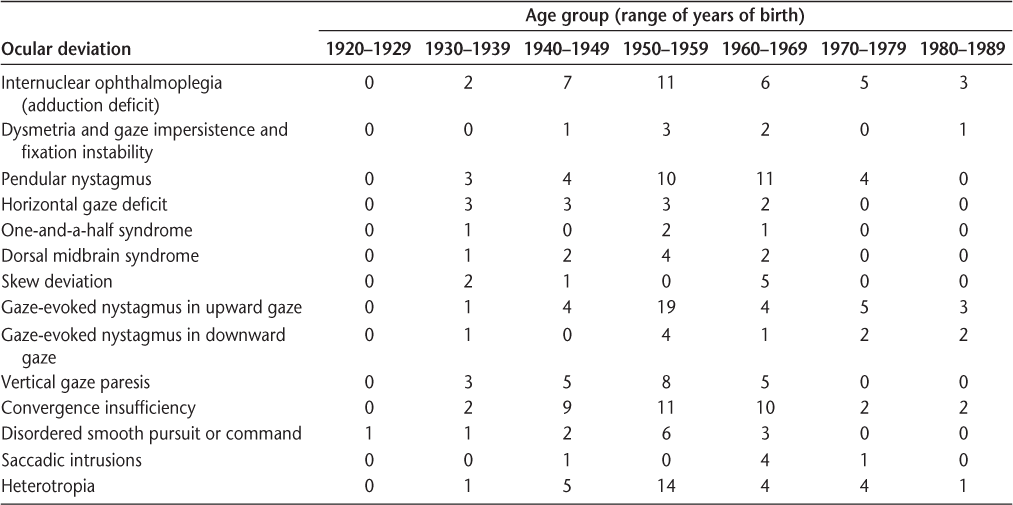
In 1992, Barnes and McDonald1 published a review of abnormalities of eye movements in MS. The article included a table with a simplified classification of eye movement abnormalities in MS (Table 3). Their table was used as a basis for a summary of eye movement abnormalities found in the current sample (Table 4).
Simplified classification of eye movement abnormalities in multiple sclerosis according to Barnes and McDonald1
Ocular deviations by age group
Nystagmus
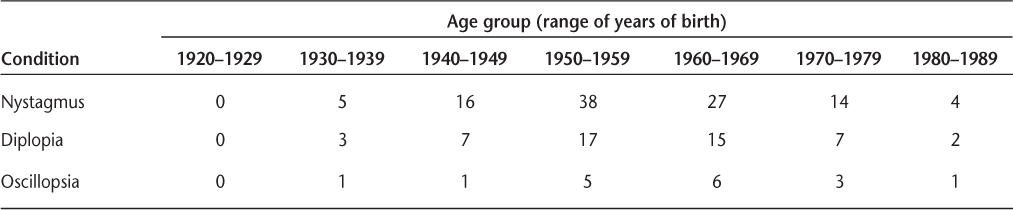
The findings for nystagmus are presented in Table 5. These findings result from a normal screening procedure at the time of the ophthalmologic examination, not from a thorough investigation, such as testing of induced nystagmus with vestibular and optokinetic stimuli. Therefore, the actual incidence of nystagmus would be much higher. In this sample, nystagmus was more frequent in males than in females and was most commonly seen in patients born between 1950 and 1969. Nystagmus present in the primary gaze was noted in 16 males and 12 females.
Cases of nystagmus, diplopia, and oscillopsia by age group
Diplopia
The number of patients who complained of diplopia at the time of examination is also presented in Table 5. The table does not distinguish between patients who had complained in the past of diplopia and those for whom diplopia was the first manifestation of MS.
Diplopia at distance could occur in all directions or in only one direction of gaze. Diplopia at distance was found to be present in 20 males, of whom 12 also had nystagmus. Diplopia at distance in only one direction of gaze was found to be present in 4 males. Diplopia at distance was found to be present in 31 females, of whom 13 also had nystagmus. Diplopia at distance in only one direction of gaze was found to be present in 2 females. Diplopia in cases where the visual acuity was less than 6/20 was noted in only 2 cases, 1 male and 1 female. Among the patients with diplopia, 18 had oculomotor abnormalities as an acute exacerbation or had experienced diplopia for a short time, and 28 had experienced diplopia for at least 3 consecutive years.
The following ocular deviations were found in the group with diplopia:
6 instances of sixth cranial nerve palsy;
2 instances of incomplete third cranial nerve palsy;
1 instance of sixth cranial nerve palsy associated with bilateral internuclear ophthalmoplegia (INO) and gaze-evoked nystagmus of both eyes in the upward gaze;
1 instance of sixth cranial nerve palsy associated with gaze-evoked nystagmus of both eyes to the left;
1 instance of unilateral INO;
2 instances of bilateral INO;
3 instances of bilateral INO associated with gaze-evoked nystagmus of both eyes in the upward gaze;
3 instances of bilateral INO associated with gaze-evoked nystagmus of both eyes in the upward and downward gaze;
1 instance of bilateral INO associated with gaze-evoked nystagmus of both eyes in the upward and downward gaze and vertical and rotatory nystagmus;
1 instance of horizontal gaze palsy;
4 instances of one-and-a-half syndrome;
9 instances of dorsal midbrain syndrome;
2 instances of saccadic intrusions;
2 instances of disordered smooth pursuit;
2 instances of diplopia in the presence of fatigue;
1 instance of photophobia that hindered screening examination;
2 instances of poor cooperation;
1 instance of bilateral INO associated with gaze-evoked nystagmus of both eyes in the upward and downward gaze, pendular nystagmus, and fixation instability;
1 instance of horizontal pendular nystagmus associated with Horner syndrome;
1 instance of conjugated pendular nystagmus associated with skew, gaze-evoked nystagmus of both eyes in the upward gaze, and exotropia;
1 instance of pendular nystagmus associated with fixation instability;
1 instance of jerk nystagmus in the gaze to the right and left associated with fixation instability and gaze impersistence;
2 instances of fixation instability associated with failure to maintain any gaze;
1 instance of skew.
Oscillopsia
Findings for oscillopsia are also presented in Table 5. Oscillopsia is a shaking field of vision that may be due to certain forms of nystagmus.2 In this sample, oscillopsia was present in 7 males and 10 females. In 4 cases there was visual acuity of the better eye of less than 6/20.
Changes in the Uveal Tract
Two female patients (born between 1950 and 1969) had signs of bilateral active uveitis: fibrous tissue in the vitreous, phlebitis in the equatorial area of the retina, snowballs in the midperiphery of the retina, posterior synechiae, early cataract, and white dots on the endothelium of each cornea.
Some patients had evidence of old uveitis. One patient with a history of sepsis due to osteomyelitis of the heel had an area of scar tissue in the retina and choroid, accompanied by floaters in the vitreous of one eye. Another patient with a history of surgery of the left hip because of severe septic arthritis was observed to have sequelae in the vitreous of his right eye, which showed a Marcus Gunn pupil. The posterior pole of that eye was covered with a fibrovascular membrane, which enlarged up to the equator at 6 o'clock and up to the equator at 12 o'clock. Another patient showed temporal pallor of both ONHs and, in one eye, several punched-out scar lesions in the choroids of the four quadrants. This patient had no history of sepsis. A fourth patient showed synechiae between the posterior surface of the iris and the anterior capsule of the lens. He had a macular scar in one eye. Another patient was known to have Fuchs iridocyclitis.
Trigeminal Neuralgia
A total of 19 patients—6 males born between 1930 and 1969 and 13 females born between 1920 and 1979—were found to have trigeminal neuralgia.
Facial Nerve Palsy
A total of 65 patients—28 males and 37 females born between 1930 and 1979—were found to have facial palsy.
Discussion of Findings
Visual Acuity
The categorization of patients shown in Table 1 is somewhat artificial, but it still conveys that the great majority of patients in this sample retain visual acuity of more than 6/20 in the better eye. Following are some considerations to be aware of:
Patients may have fluctuating vision, with difficulty seeing counting fingers one week and the ability to see better than 6/20 the following week. This is probably due to fatigue.
In some cases, visual acuity of one eye improves when the head is tilted to one side or when the clinician takes more time to measure it. This phenomenon is also seen in the presentation of Ishihara plates: the plates may be recognized after sufficient screening time.
It can be difficult to measure visual acuity accurately: patients may not cooperate during the examination because of aphasia, communication problems, speech defects, or attention deficit. Occasionally, tremor of the head is most troublesome.
Amblyopia (lazy eye) or poor vision due to an accident that has no connection with MS is occasionally the reason for poor vision.
Changes of the Optic Nerve Head
Recurrent attacks of optic neuritis irreversibly destroy fibers of the optic pathway. If the process of optic neuritis is sufficiently destructive, the ONH will lose its normal pink color and become pale, first in the temporal sector. In advanced cases a chalky white disk will appear. Another ONH characteristic in MS is a pale disk with a pathologic excavation. Pallor and excavation of the ONH have many causes, and the appearance of the ONH alone cannot differentiate the origin of optic neuropathy. It is necessary to take the whole person into consideration.
An excavated ONH is one of the characteristics of glaucoma, a common cause of blindness.3 Elevated intra-ocular pressure is another characteristic of glaucoma, but this was found in only a few cases. In this sample, very few patients were known to have glaucoma. Furthermore, the diagnosis of glaucoma is not always easy. The most important characteristic of glaucomatous cupping is the vertical elongation of the cup and a corresponding nerve fiber bundle visual field defect. Many of the patients in this sample have major handicaps, such as instability of the torso and neck, paresis of the lower and/or upper extremities, and cognitive impairment. In such cases, searching for a fiber bundle visual field defect by means of a static automatic perimeter is pointless.
Other causes of a pale excavated ONH are ischemic disorders, transsynaptic degeneration, and traumatic, compressive, hereditary, toxic, and infectious optic neuropathy.3 In this sample, 1 patient had Leber hereditary optic neuropathy, 1 patient had a tumor of one of the optic nerves, and a few somewhat younger patients had cerebral infarction or thrombosis of a venous sinus. Many of these patients have complications from osteoporosis (a well-known consequence of insufficient activity) and from falls, with some having broken their wrist up to ten times or having suffered skull fractures. Indirect injuries may be caused by forces transmitted through the bones of the skull or by stretching of the optic nerve. There may be a toxic effect of medication. Some of these patients suffer from such great pain that they seek relief through drinking alcohol or smoking, even using cannabis or heroin.
Dysfunction of the autonomic nervous system is quite common, possibly leading to severe hypotension or hypertension, gastroparesis or gastrointestinal problems that may need surgical correction and cause malabsorption, breathing difficulties, renal failure, and so on. Other diseases that may appear include thyroid problems, Crohn disease, psychiatric illness, chronic fatigue, and anomalies of the spinal canal, which may require multiple surgical procedures. All of these problems can contribute to failure of the function of the optic nerve. The ONH pallor is often not only a consequence of demyelination.
Oculomotor Balance
Abnormalities of eye movements are frequently observed in MS patients. These abnormalities may lead to visual failure and eyestrain. Some patients present with severe disruption of the normal coordination of eye movements and serious complaints related to eyestrain. These problems may disappear after several months. However, some patients do not experience improvement in ocular motility with time. The results of examination of ocular deviations may vary from week to week, leading to inconsistency in the findings of different examiners. Such variability may be due to a change in medication regimen, fatigue, or the Uhthoff phenomenon.4 5
Nystagmus
According to Zee,6 nystagmus is probably the most common ocular motor abnormality in patients with MS. Various types of nystagmus may be seen in MS. Gaze-evoked, central vestibular, dissociated, and pendular nystagmus are the most common. Sometimes a nystagmus present in the primary gaze is detected only during indirect ophthalmoscopy of the fundus or when viewing the eye through a video camera of a computerized automated perimeter for the period of testing the visual field. According to Barnes and McDonald,1 downbeat nystagmus is much less common in MS than upbeat nystagmus. The findings of the present study are consistent with their report.
Diplopia
In 16 patients in this study, the medical record showed that diplopia was the initial demyelinating event. Investigation of heterophoria or heterotropia by means of a Maddox groove or the classic tests for diplopia such as a Hess screen test are not always valid for these cases,7 for the following reasons:
Patients often have difficulties sustaining attention and estimating spatial intervals during the examination.
Patients may have visual field defects or changes of the ONH that indicate the presence of visual field defects.
Photophobia and actual pain during some eye movements can hinder effective examination.
Some of the study participants developed bedsores because of a complicated bone fracture or tail bone injury.
In some cases the test showed that the angle of squint changed nearly every second.
Some of these patients have difficulty focusing on an object, and this may be the main problem, resulting in inadequate gaze holding. A cover test is not possible because the patient cannot maintain fixation during the test.
Isolated oculomotor nerve palsies can cause diplopia. Some cases of horizontal diplopia presented as sixth nerve palsy. One 38-year-old woman presented with acute cranial third nerve palsy with large pupil, accommodation problems, and diplopia mimicking a compressive lesion in the subarachnoid space. Initially the diplopia was monocular, but subsequently exotropia and head tilt with binocular diplopia became apparent.
Patients with MS may present with diplopia due to INO. Many cases are mild and are not identified during the screening examination.8 Bilateral INO is often present, and INO may be combined with another deficit such as horizontal or vertical gaze palsy or skew. Disordered smooth pursuit and a corresponding abnormality of optokinetic nystagmus are found in more than 50% of patients with MS, according to Barnes and McDonald.1 In the current study, disordered smooth pursuit was the major abnormality found in 13 patients. Problems with voluntary saccades and pursuit do not always result in complaints.
In some cases, patients complain of diplopia when in fact visual acuity is poor, and the patient's perceived double vision is due to the poor vision itself rather than a deviation of muscular balance.
Medication, such as 4-aminopyridine, may cause these problems, either by itself or through an overdose or a change in dose. In such cases, consultation with the treating neurologist is required.
Oscillopsia
Oscillopsia is not always present in patients with nystagmus or saccadic intrusions due to MS. Some patients complain of itching and tearing, diplopia (especially when fatigued), neck pain, reduced depth perception, blurred vision, or vertigo. Some patients have become accustomed over many years to seeing a “moving world” and find the problem not worth mentioning. Oscillopsia varies from patient to patient. It may be more pronounced in one eye than in the other. It may be present in all directions of gaze, only for near tasks, only when looking up or down at distance, only when tilting the head to one side, only in the periphery of the visual field, or only in a certain position (eg, lying down). A smooth movement may be seen as a shaking movement, and a shaking field of vision may appear when exercising, taking a shower, or walking. In one patient in this study, the head and eyes began to shake when the eyes, showing a fast horizontal pendular nystagmus in the primary position, moved away from the primary position.
Changes in the Uveal Tract
The frequency of uveitis in this sample was low. However, because it can lead to blindness, regular examinations by an ophthalmologist to detect this condition are important. Visual failure is often overlooked in MS patients because their other neurologic deficits demand more attention. If signs of uveitis are present, steroid and atropine eye drops are prescribed.9 Ophthalmologists should be careful not to overprescribe atropine medication. One patient presented with a marasmus-like cachexia, and intoxication due to atropine can lead to delirium.
Trigeminal Neuralgia
Trigeminal neuralgia in MS patients may be severe, and treatment may require more than one type of medication. In this study, trigeminal neuralgia was the initial neurologic deficit in 3 patients.
Facial Nerve Palsy
Most of the cases of facial nerve palsy in this study were mild, with no patients requiring surgical correction. Facial palsy was the initial neurologic deficit in 3 of the patients. Myokymia of the lower eyelid was the initial demyelinating event in 1 case.
How to Help MS Patients with Ocular Problems
Patients with MS, and often their primary caregivers or neurologists as well, tend to attribute all ocular problems to the MS. Regardless of the cause of the problems, there are many ways to help these patients. If refractive errors are discovered, they should be corrected. Some patients with fairly good visual acuity, normal ONHs, and normal motility balance seek help because of a specific problem such as not seeing a computer screen well enough. If their eyeglass prescription is correct, this problem can often be solved by using a larger screen. Some patients obtain relief from headaches with the use of Fresnel prisms that correct small-angle esotropia or exotropia.
If patients present with symptoms due to acute optic neuritis or any acute deviation of normal eye movement, treatment with intravenous steroids is warranted.10 11 Other causes of neuritis such as vitamin deficiency, aneurysm, side effects of medication, alcohol abuse, neuromyelitis optica, Leber disease, infectious and inflammatory disease, and systemic and metabolic disorders should always be considered by examination of blood and urine and magnetic resonance imaging of the brain and cord.12 A number of patients in this study took medication for epilepsy such as levetiracetam, gabapentin, pregabalin, and lamotrigine, all of which may cause diplopia or other vision problems. Patients with MS also often have depression or bladder dysfunction. Medications for these conditions often have anticholinergic side effects and cause dry eye, accommodation problems (which can be corrected with glasses), and mydriasis. Light flashes may be caused by medications such as venlafaxine. Inhibitors of acid secretion in the stomach, such as omeprazole, may cause depression of the visual field.
Some MS patients with poor visual acuity have dysfunction of the extremities. In these cases, it does not make sense to prescribe visual aids that are held in the hand to magnify images, either nearby or at a distance. These patients can be taught to work with computers adapted for patients with functional low vision and multiple disabilities. Special computer mice and speech technology devices are available. Tremor is a major handicap in some cases.
Some patients have a disturbance of the tear film and the surface layer of the cornea due to poor blinking, chronic kerato-blepharo-conjunctivitis, or medication side effects. Blepharitis and dry eye should be treated appropriately. Poor blinking may allow problems to become chronic.
Educating MS patients about the Uhthoff phenomenon is important. Patients must understand that heat, exercise, fever, and psychological stress can bring about temporary symptoms such as worsening vision, diplopia, and oscillopsia, and should be instructed to avoid such circumstances whenever possible.5
Some patients in this study with diplopia obtained relief through the use of Fresnel prisms (correcting large-angle exotropia), wearing glasses that diminished contrast acuity (when the angle of deviation was constantly changing), or occlusion (if the prisms were not helpful). Occlusion of one eye was sometimes refused for cosmetic reasons and because of cognitive problems. In patients with visual acuity better than 6/20 who have lost the ability to fixate, the medication memantine is quite helpful.
Nystagmus and uncontrolled eye movements can be extremely troublesome. Patients may experience saccadic intrusions as even more problematic than their tetraparesis. Medications such as gabapentin or memantine can be helpful, but such medications are not always appropriate.13–15 People with MS already tend to take many medications to control spasticity, neurogenic pain, depression, bladder dysfunction, fatigue, and nausea. Renal failure is sometimes present.
Photophobia can be severe, and appropriate sunglasses may help. For some patients, even an examination of the pupil is not possible.
In rare cases, patients with visual acuity of less than 3/60 deny any need for help or the existence of visual problems. These patients should be referred to a neurologist. They may have cataracts due to aging or the use of medication such as steroids. In some hospitals MS is treated with high-dose steroids on a regular basis. Only in 1 case was surgical treatment necessary to improve visual acuity. In 1 case, congenital cataracts prevented visualization of the ONH, but the patient did not want cataract surgery. In another case, cataract surgery was delayed because of the patient's poor general condition.
Finally, the common problem of fatigue in MS patients should be addressed. Factors involved in fatigue in this population include medications, sleep disturbances, depression, abnormal nerve conduction, lack of exercise, and the disease itself.16
Conclusion
The majority of MS patients in this sample in each age group retained visual acuity of more than 6/20 in the better eye. The ONH was found to be normal in many patients. Both localized and diffuse patterns of ONH pallor were seen. Pathologic excavation of the ONH was also noted. In cases of pallor of the ONH, many factors besides demyelination may contribute to the optic nerve dysfunction. The eye movement abnormalities found in this group of MS patients were similar to those previously reported and included nystagmus, diplopia, and oscillopsia, with 2 cases of active uveitis encountered. Many steps can be taken to help MS patients with the wide variety of ocular complaints found in this population.
PracticePoints
People with MS may have a variety of ocular complaints, many of which are manifestations of the disease.
Among the ocular problems found in this population are poor visual acuity, abnormalities of the optic nerve head, nystagmus, diplopia, and oscillopsia.
The ophthalmologist can help MS patients by identifying refractive errors, helping them combat fatigue, and checking for uveitis, a rare but serious condition that can lead to blindness if left untreated.
Acknowledgments
The author is grateful to Prof. Dr. Dirk De Ridder, Chairman of the Nationaal MS Centrum, and to Drs. Marianne Charlier, Marie C. Deville, Marie B. D'Hooghe, Stephan Ilsbroukx, Piet Ketelaer, Tom Meurrens, Guy Nagels, Anoek Symons, Katia Van Laere, and An Van Nunen for the opportunity to see and examine their patients.
References
Barnes D, McDonald WI. The ocular manifestations of multiple sclerosis. 2. Abnormalities of eye movements. J Neurol Neurosurg Psychiatry. 1992; 55: 863–868.
Biousse V Newman J. Abnormal visual perceptions: hallucinations and illusions. In: Biousse V. Neuro-Ophthalmology Illustrated. New York, NY: Thieme; 2009:261–268.
Roodhooft JM. Nonglaucomatous optic disk atrophy and excavation in the elderly. Bull Soc belge Ophtalmol. 2003; 287: 45–49.
Barnes D, McDonald WI. The ocular manifestations of multiple sclerosis. 1. Abnormalities of the afferent visual system. J Neurol Neurosurg Psychiatry. 1992; 55: 747–752.
Frohman EM, Greenberg BM. Pearls: multiple sclerosis. Semin Neurol. 2010; 30: 97–102.
Zee DS. Nystagmus in multiple sclerosis. Bull Soc belge Ophtalmol. 1983; 208: 211–217.
Roodhooft JM. Screen tests used to map out ocular deviations. Bull Soc belge Ophtalmol. 2007; 305: 57–67.
Frohman EM, Frohman TC, Zee DS, McColl R, Galetta S. The neuro-ophthalmology of multiple sclerosis. Lancet Neurol. 2005; 4: 111–121.
Roodhooft JM. Ocular problems in early stages of multiple sclerosis. Bull Soc belge Ophtalmol 2009; 313: 65–68.
Biousse V, Newman J. Optic neuropathies. In: Biousse V. Neuro-Ophthalmology Illustrated. New York, NY: Thieme; 2009:172–236.
Graves J, Balcer LJ. Eye disorders in patients with multiple sclerosis: natural history and management. Clin Ophthalmol. 2010; 4: 1409–1422.
Miller DH, Weinshenker BG, Fillipi M, et al. Differential diagnosis of suspected multiple sclerosis: a consensus approach. Mult Scler. 2008; 14: 1157–1174.
Van Nechel C. Les anomalies oculomotrices dues aux medicaments. Bull Soc belge Ophtalmol. 2007; 304: 179–184.
Kalla R, Spiegel R, Wagner J, Rettinger N, Jahn K, Strupp M. Pharmacotherapie zentraler nystagmusformen. Nervenartz. 2008; 79: 1377–1385.
Solaro C, Uccelli MM. Pharmacological management of pain in patients with multiple sclerosis. Drugs. 2010; 70: 1245–1254.
Kos D, Kerckhofs E, Nagels G, D'Hooghe MB, Ilsbroukx S. Origin of fatigue in multiple sclerosis: review of the literature. Neurorehabil Neural Repair. 2008; 22: 91–100.
Financial Disclosures: The author has no conflicts of interests to disclose.
This work was presented at the 16th Annual Conference of Rehabilitation in Multiple Sclerosis (RIMS) in Turku, Finland, on May 13, 2011.







