Publication
Research Article
International Journal of MS Care
Strength Training to Improve Gait in People with Multiple Sclerosis
Author(s):
Abstract
Background:
There are mixed reports on the effectiveness of strength training to improve gait performance in people with multiple sclerosis (MS), yet the reasons for these inconsistent results are not clear. Therefore, a critical review was conducted to explore dosage, frequency, mode, position, and muscle targets of studies that have included strength training in people with MS.
Methods:
An electronic search was conducted through July 2017. Randomized controlled trials involving people with MS were included that implemented strength training with or without other interventions and assessed 1) strength in the lower extremities and/or trunk and 2) gait speed and/or endurance. Strength and gait results were extracted, along with exercise frequency, intensity, duration, mode, position, and muscle targets.
Results:
Thirteen trials met the inclusion criteria; nine used dosing consistent with recommended guidelines. Overall, six studies reported significant between-group strength improvements, and four reported within-group changes. Four studies reported significant between-group gait improvements for gait speed and/or endurance, and two reported within-group changes. Most exercises were performed on exercise machines while sitting, supine, or prone. The most common intervention target was knee extension.
Conclusions:
Studies generally improved strength, yet only two studies reported potentially meaningful between-group changes in gait. Future strength intervention studies designed to improve gait might consider dosing beyond that of the minimum intensity to improve strength and explore muscles targets, positions, and modes that are task-specific to walking.
Difficulty walking is one of the most commonly reported problems in people with multiple sclerosis (MS),1 and 10 years after diagnosis up to 93% of people with MS report limitations in their walking.2 Many systematic reviews have examined the efficacy of rehabilitation interventions in participants with MS; although there is evidence that physical therapy and exercise can improve activities and participation, including gait, there is not conclusive evidence that clearly favors a specific intervention or approach.3–7 This highlights an important clinical problem for those working with people who have MS: there are a variety of impairments and activity limitations to consider targeting to improve gait, and a variety of interventions to choose from that have only moderate-to-low evidence to support their efficacy.3
Of the modifiable impairments, muscle weakness contributes strongly to gait in people with MS, is highly prevalent, and can be widespread through the lower extremities and trunk.8–10 Strength training is considered one of the basic elements of exercise and physical activity for people with MS.11 Several systematic reviews have established the effectiveness of strength training to improve strength, but the effects on gait and mobility are not as consistent.4 10 12–16 There are several commonly proposed explanations for these inconsistent results, including rigor of design, heterogeneity of interventions and outcomes, and characteristics of enrolled samples (eg, disability level, MS type, and other contributors besides weakness).4 12–16 Another reason might include variability of exercise parameters such as frequency, intensity, and duration.3 Although there are evidence-based parameters for strength training in people with MS,11 17 it is possible that for strength training to improve function such as gait, it may need to be applied using parameters that are different from what is required to simply improve force production. A final and potentially important explanation that has received less consideration is that strength training studies to improve gait in people with MS may not include exercises with the appropriate intervention approach in terms of modes, positions, or muscle targets.18 Strength training using modes or positions that are not functional for gait, or are not targeted to muscle groups that are important for walking, may not improve gait even when strength improves.
Therefore, this review critically appraised the exercise parameters (intensity, frequency, and duration) and intervention approach (mode, position, and muscle targets) of individual strength training studies that measured both strength and gait performance outcomes with the goal of providing new perspectives and generating novel hypotheses on the topic of strength training to improve gait in people with MS. A better understanding of the application of strength training to improve gait could aid future study design and ultimately might help contribute to more consistent and meaningful improvements in gait.
Methods
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) was used as a guideline for conducting this critical review19; the protocol was registered on PROSPERO (CRD42017072642).
Eligibility Criteria
Randomized controlled trials were included if participants had a diagnosis of MS and interventions included strength training for the lower extremities and/or trunk. Strength training was defined as any intervention that applied exercises using external resistance or body weight with the purpose of improving strength. Because the primary objective of this study was not to assess the efficacy of strength training, strength training did not need to be the primary intervention of the included studies, but studies did have to include strength interventions and outcome assessments. In addition, studies did not need to have a primary outcome of improving gait, but studies were included if they measured gait speed and/or endurance outcomes. Finally, the comparator could include other active interventions or inactive control groups that did not receive intervention. Articles were excluded if 1) other populations were included and participants with MS were not analyzed separately or 2) they were not published in English.
Databases, Search Methods, and Risk-of-Bias Assessment
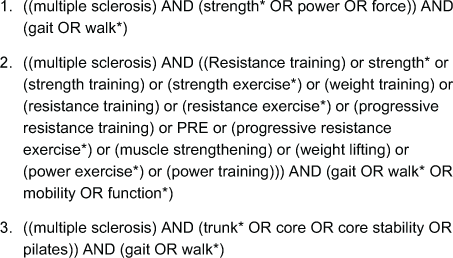
Electronic searches of the PubMed, PEDro (Physiotherapy Evidence Database), and Embase databases were conducted using combinations of the following search terms: multiple sclerosis, strength, power, force, resistance training, strength training, progressive resistance training, weight training, gait, walking, mobility, and function. In addition, the following Medical Subject Heading terms were searched on PubMed: multiple sclerosis, gait, resistance training, and weight training. The full search strategy conducted on the PubMed database is presented in Figure 1. In addition to primary searches, reference lists of relevant articles, including systematic reviews, were examined for additional relevant articles. Two authors (M.M.M. and S.G.) conducted searches and screened articles. Any disagreements on article selection were settled by a third author (M.S.), and where methods or reporting were not clear, attempts were made to contact primary authors. Risk of study bias was assessed (by M.M.M. and S.G.) using the PEDro scale and was validated using the PEDro database. Studies were not excluded based on PEDro scale score.
Complete search strategy for PubMed
Data Extraction and Synthesis
Information about sample size, power calculation, disability level of participants, length of follow-up, and other interventions was extracted from each study. In addition, data were extracted for 1) strength and gait outcomes used in each study; 2) reported results for strength and gait outcomes; 3) exercise parameters (strength training intensity, frequency, and duration); and 4) intervention approach (mode, position, and muscle targets) of each exercise. Each article was reviewed by two of us (M.M.M. and S.G.) independently. Data were extracted for postintervention measures only, because not all studies included a follow-up assessment. Data were extracted for between-group comparisons when available, but if not reported, data for within-group comparisons were extracted. Extracted data from the included studies are synthesized in the tables and summarized in the text. Data on exercise parameters were compared with frequency and intensity guidelines for strength training in people with MS of two to three times per week, one to four sets of 10 to 15 repetitions at 10 to 15 repetitions maximum.11 17 Results for changes in gait were also discussed in the context of meaningful or clinically important change. Based on the broad eligibility criteria, it was expected that there would be considerable heterogeneity between studies in terms of interventions (eg, including other interventions besides strength training) and outcomes (eg, strength or gait not the primary outcome), thus no meta-analysis was planned.
Results
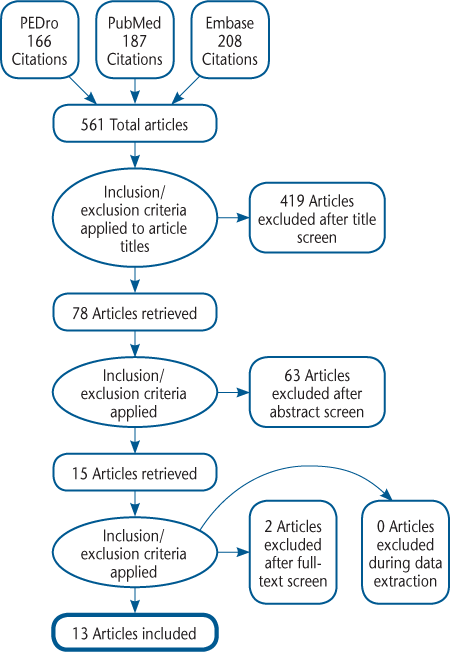
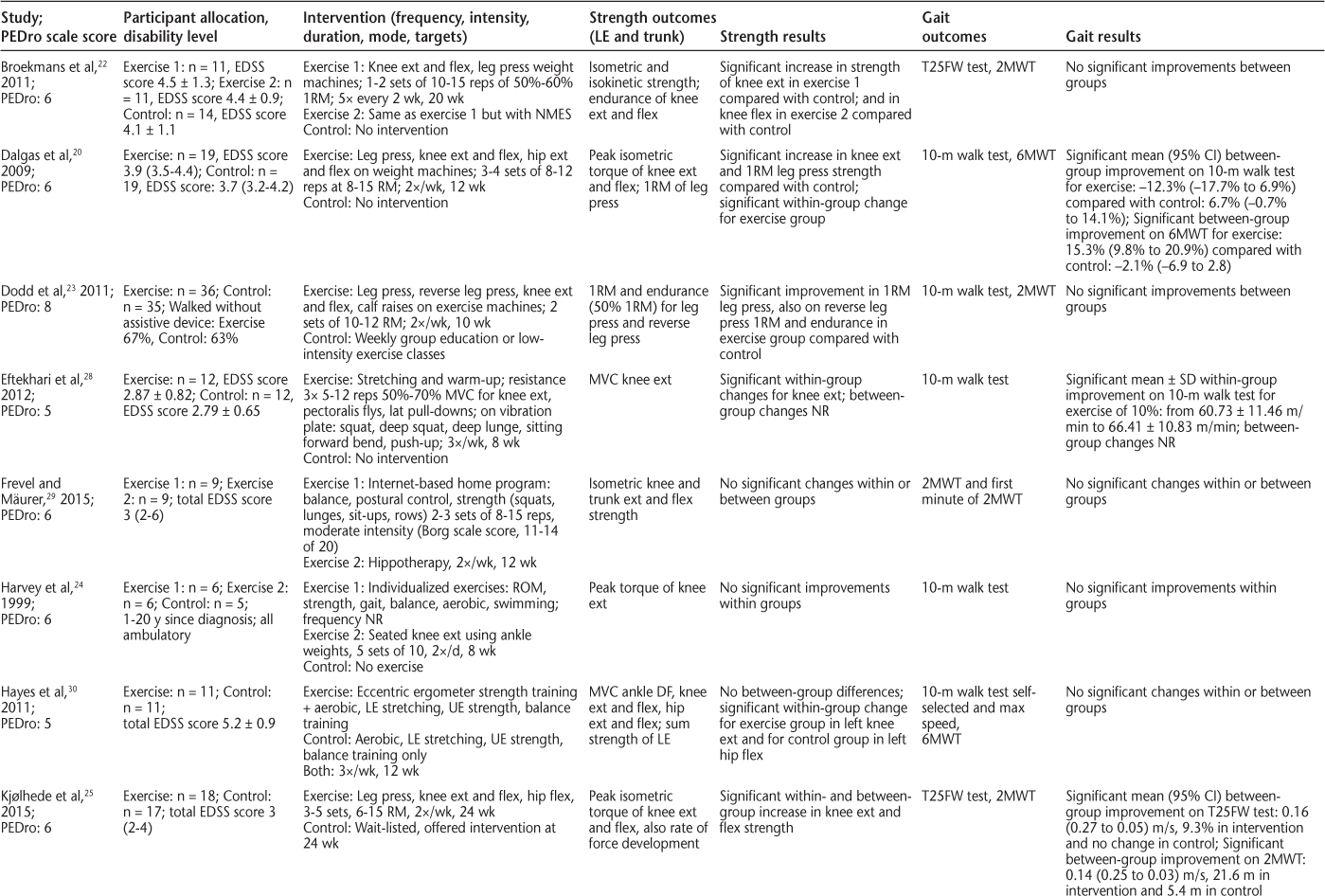
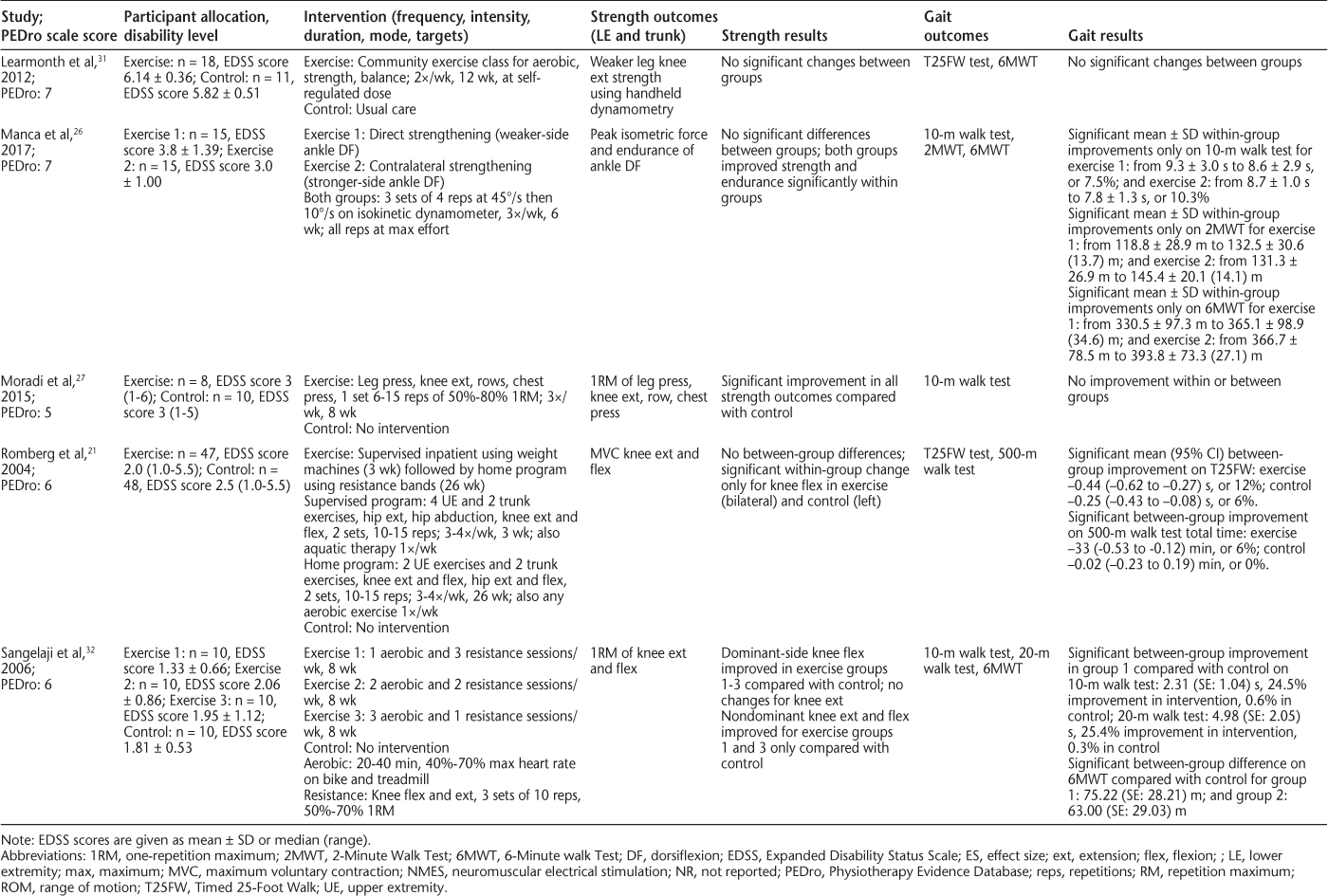
Five hundred sixty-one articles were identified via electronic search of the three databases through July 2017 (Figure 2). After applying the eligibility criteria and removing duplicates, a total of 13 articles20–32 met the eligibility criteria (Table 1). No additional studies were identified after reviewing reference lists from the included articles or other relevant systematic reviews. Two authors provided clarity on protocols.20 21 Seven studies had at least one arm that included only strengthening,20 22–27 and six studies included strengthening with other interventions,21 28–32 most commonly aerobic exercise, stretching, and balance21 29–32 but also combined with a vibration plate.28 Nine studies were performed primarily in a supervised outpatient setting20 22 23 25–28 30 32; three included primarily home exercise programs,21 24 29 and one involved a community exercise class.31 Disability level varied across the studies, but most participants were ambulatory for at least 100 m with or without an assistive device (Expanded Disability Status Scale [EDSS] score <6.0) except in the study by Learmonth et al,31 in which the mean ± SD EDSS score in the intervention group was 6.14 ± 0.36. Dodd et al23 and Harvey et al24 did not report disability using the EDSS, but all of their participants were reported to be ambulatory. Sample sizes ranged from 17 to 95 participants; two studies were powered to detect changes in gait,21 23 and three for strength changes.20 25 26 The median PEDro score was 6 (range, 5–8). Full risk-of-bias assessment is presented in Table 2.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram
Characteristics of studies and main results for strength and gait outcomes (page 1 of 2)
Characteristics of studies and main results for strength and gait outcomes (page 2 of 2)
Risk of bias in individual studies based on PEDro scale scores and on presence or absence of a priori sample size calculation
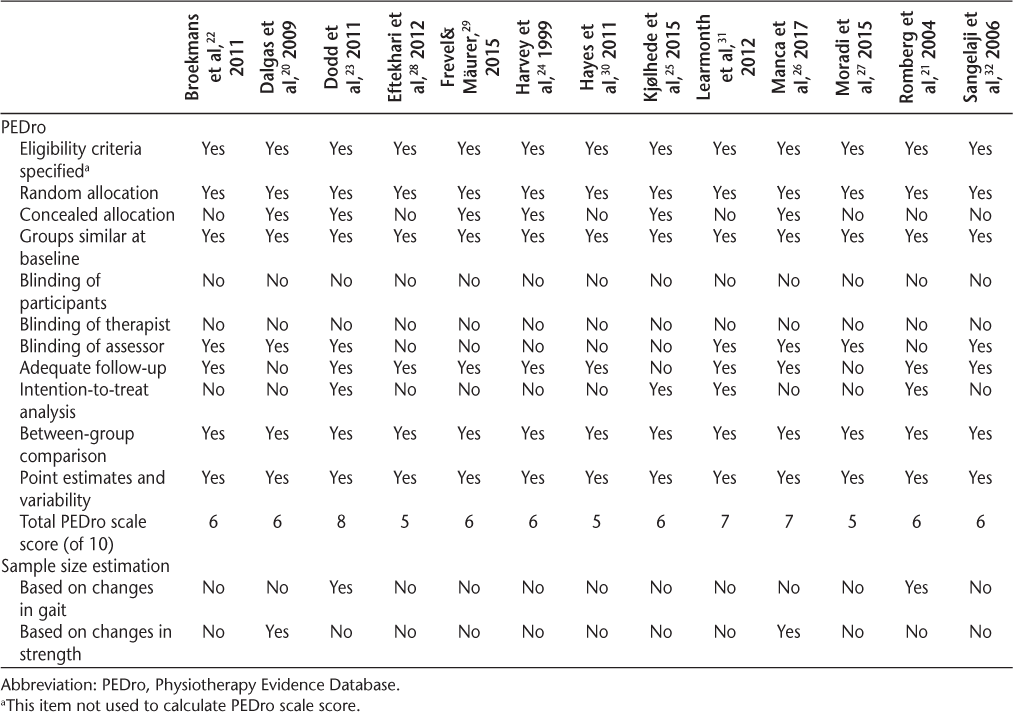
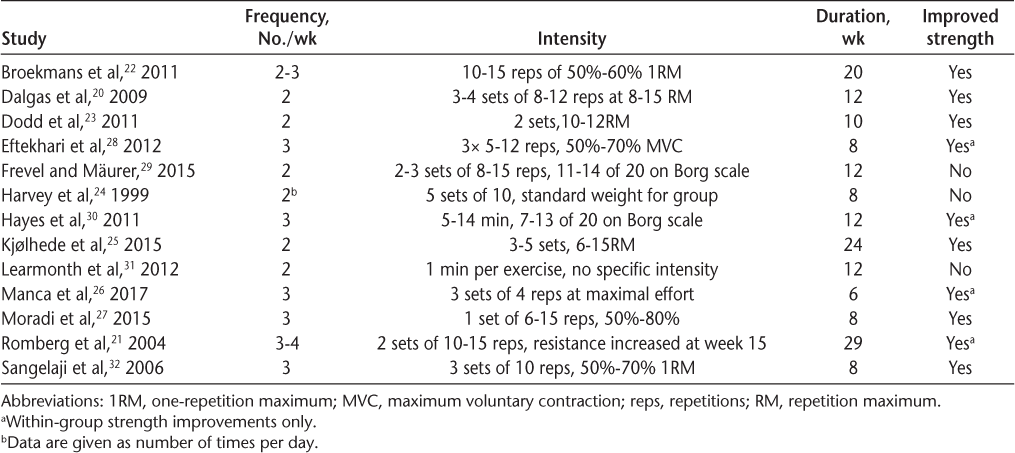
Exercise Parameters: Intensity, Frequency, and Duration
Regarding dosing, eight studies reported intensity that used progressive resistance based on assessment of maximal number of repetitions of each participant,20–23 25 27 28 32 and one study progressed exercise based on maximal effort on an isokinetic dynamometer.26 Meanwhile, two studies used rate of perceived exertion for progression criteria,29 30 and two used a standard group prescription that did not individually progress resistance.24 31 All the studies had participants perform exercises two to three times a week except that by Harvey et al,24 in which exercises were performed twice daily. Duration of intervention was between 6 and 29 weeks. Exercise parameters for each study are presented in Table 3.
Exercise parameters of frequency, intensity, and duration by individual study
Intervention Approach
Mode and Position
Seven studies used traditional weight machines for strength training,20 22 23 25 27 28 32 and one study trained on the same isokinetic dynamometer used to assess strength outcomes.26 Three studies used body weight to provide resistance28 29 31 (one in addition to weight machines28), one study used cuff weights,24 one used both resistance bands and weight machines,21 and one used a seated lower extremity ergometer.30 Six studies included strengthening exercises in standing,20 21 25 28 29 31 and all the studies included exercises in positions other than standing. Of the nonstanding positions, seated exercise was used in 12 studies,20–28 30–32 and the supine and/or prone position was used in three studies.23 25 29 The intervention approach for each study is presented in Table 4.
Intervention approach by individual study: strength targets, positions, and modes
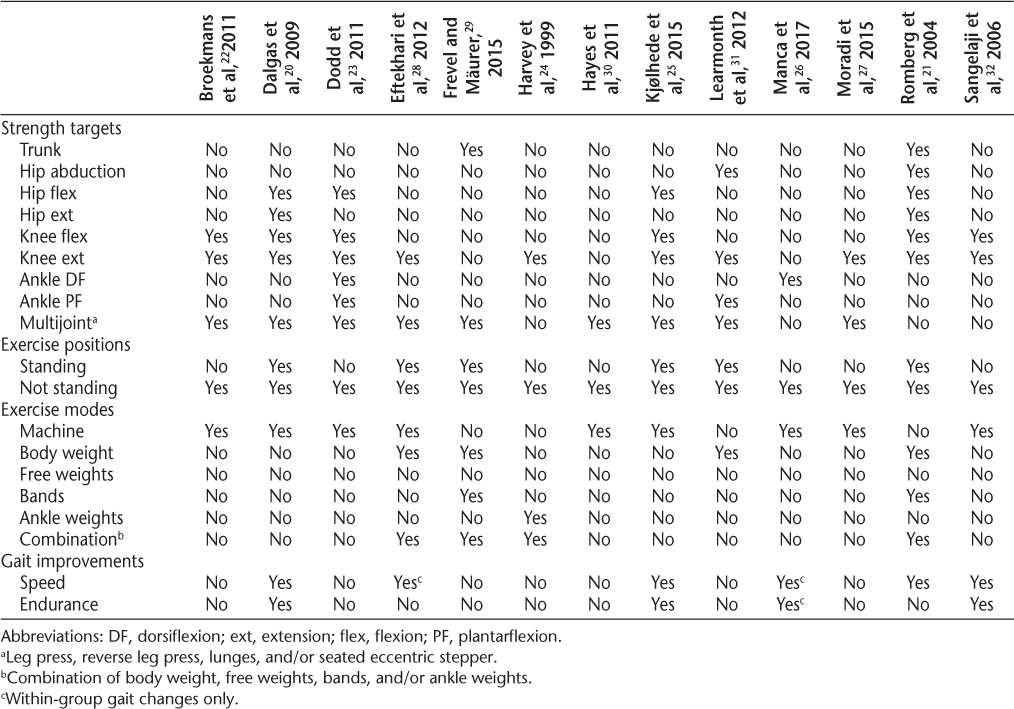
Muscle Targets
Knee extension strength was the most common muscle strength target, with ten studies explicitly isolating the knee extensors for strength training.20–25 27 28 31 32 Knee flexion was targeted in six studies.20–23 25 32 Hip flexion and extension were targeted in three studies20 21 25; ankle plantarflexion,23 31 hip abduction,21 31 and the trunk21 29 were each targeted in two studies; and one study targeted ankle dorsiflexion only.26 Several multijoint exercises also were used: leg press was used in five studies,22 20 23 25 27 squats or lunges in three studies,28 29 31 and reverse leg press in one study.23 The protocol by Hayes et al30 was also multijoint, involving eccentric strengthening in a seated position with movements similar to leg press and reverse leg press. Seven of the studies targeted one to three lower extremity and/or trunk exercises,22 24 26 27 29 30 32 and six studies used between four and six exercises.20 21 23 25 28 31 Finally, seven studies included at least one upper extremity exercise in addition to lower extremity exercise.21 25 27–31 Muscle targets by individual study are presented in Table 4.
Strength and Gait Outcomes
Ten studies measured strength using computerized, electromechanical, fixed, or handheld dynamometry to assess maximal force20–22 24–26 28–31; one of these studies also assessed one-repetition maximum (1RM),20 and two also assessed muscle endurance.22 26 One study assessed only 1RM and endurance,23 and two studies assessed only 1RM.27 32 The most common strength outcome was knee extension, assessed by 11 studies,20–22 24 25 27–32 followed by knee flexion (seven studies),20–22 25 29 30 32 and leg press (three studies).20 23 27 Two studies assessed ankle dorsiflexion,26 30 one assessed hip extension and flexion,30 one reverse leg press,23 one trunk extension and flexion,29 and one upper extremity muscle groups.27 Only three studies measured strength in more than two lower extremity or trunk muscle groups.20 29 30
Twelve studies measured gait speed: eight used the 10-meter walk test20 23 24 26–28 30 32; four, the Timed 25-Foot Walk (T25FW) test21 22 25 31; one, the 500-meter walk test in addition to the T25FW test21; and one, the 20-meter walk test in addition to the 10-meter walk test.32 Nine studies measured gait endurance: four used the 2-Minute Walk Test (2MWT)22 23 25 29; four, the 6-Minute Walk Test (6MWT)20 30–32; and one, both the 2MWT and the 6MWT.26
Regarding strength, six of the included studies reported significant improvements in strength for the intervention arm compared with a control group,20 22 23 25 27 32 and an additional four studies reported significant within-group changes for the strength intervention group in at least one muscle.21 26 28 30 Of the seven studies that had an intervention arm that exclusively performed strength training exercises, six reported significant improvements in strength20 22 23 25–27; and of the six studies that included other interventions along with strength training, four reported improved strength.21 28 30 32
Regarding gait outcomes, three of the included studies reported significant between-group differences in both gait speed and endurance,20 25 32 one study reported between-group changes in gait speed only,21 one study reported within-group changes in gait speed and endurance,26 and one reported within-group changes in gait speed only.28 Significant changes in the included studies for the intervention group ranged from 9.3% to 12% for the T25FW test,21 25 7.5% to 24.5% for the 10-meter walk test,20 26 28 32 and 6% for the 500-meter walk test.21 On the 2MWT, significant changes within the intervention group ranged from 13.7 to 21.6 m,25 26 and on the 6MWT, changes ranged from 27.1 to 81.2 m.20 26 32 Table 1 reports between or within-group changes for studies that reported significant changes in gait.
Of the ten studies that improved strength between or within groups, nine used frequency and intensity consistent with guidelines for people with MS,20–23 25–28 32 and six reported gait improvements between or within groups.20 21 25 26 28 32 The three studies that did not improve strength also did not improve gait.24 29 31 In terms of intervention approach, of the six studies that improved gait, four targeted muscles in addition to the knee,20 21 25 28 and one did not target knee muscles at all26; four studies implemented strength training in a standing position20 21 25 28; and two used modes other than weight machines.21 28
Finally, of the five studies that were powered for gait and/or strength changes, four reported significant improvements in both strength and gait,20 21 25 26 and one reported significant strength changes only.23 In addition, of the six studies that improved gait, four included at least 15 participants in the intervention arm20 21 25 26; and of the seven studies that did not improve gait, five had fewer than 15 participants in the intervention arm.22 24 27 29 30
Discussion
This review summarized the results of randomized controlled trials that included strength training, both with and without other interventions. Studies were included that assessed both strength and gait performance outcomes in people with MS, and a critical analysis was performed on the exercise parameters (intensity, frequency, and duration) and intervention approach (mode, position, and muscle target) used in those studies. The goal of a critical review is often to generate new hypotheses or perspectives on a topic.33 The results of this review highlighted the areas of exercise parameters and intervention approach that provide novel insights into the application of strength training and may, at least partially, explain why strength training has not resulted in consistent improvements in gait.
With respect to exercise parameters, nine20–23 25–28 32 of the ten studies that reported strength improvements used intensities and frequencies that were, at minimum, within the recommended parameters of progressive resistance training for people with MS.11 17 Duration of training is not included in the recommended guidelines, but all the studies had a duration consistent with minimum duration for strengthening in healthy populations.34 Although strength improved in studies that used appropriate exercise parameters, it could be that intensity needs to be higher to improve gait performance. In older adults, where strength training has been found to be the single most effective exercise intervention to improve gait speed, intensity is between 70% and 80% 1RM (or up to 7- to 8-repetition maximum).35 Only three studies included in this review progressed to intensities this high,20 25 27 and although no definitive conclusions can be made on only these three trials, all did improve both gait speed and endurance. In two recent prospective cohort trials, higher-intensity strength training in people with MS seemed to be well-tolerated and was associated with improvements in gait speed36 and endurance.37 Future studies should investigate the efficacy of higher-intensity strength training on gait and further explore the dose-response relationship in randomized controlled trials.
With respect to intervention approach, strength training in the included studies was primarily performed on weight machines in sitting, supine, and prone positions—none of which is a functional, task-specific position needed for walking.18 The most common strengthening exercise was seated open chain knee extension performed on a weight machine. The findings from this review are in agreement with a previous review on strength training in a variety of neurologic conditions, including MS, that also found an overwhelming focus on knee strengthening in nonstanding positions using weight machines and a lack of consistent gait improvements.18 Owing to the heterogeneity of approaches of the included studies, this review was not able to make conclusions about which muscle targets, positions, or modes are best to improve gait performance. Knee extension and flexion strength have been reported to be strongly associated with gait,38 39 and this may help explain why most trials focused on these muscles; however, only one study explicitly justified its approach.23 Independent of the position or mode in which it is strengthened, knee extension might not be a particularly important muscle for strengthening for people with MS who are already ambulatory, and, therefore, likely have sufficient lower extremity extensor strength to maintain standing. Furthermore, knee flexion strength might have a stronger correlation to gait speed than knee extension and, therefore, may be a more important target of intervention,38 39 but only six studies included in this review targeted knee flexion.20–23 25 32 Previous literature on the association of strength to gait also supports the importance of strength in ankle plantarflexion and dorsiflexion, hip flexion and extension, and trunk flexion to gait performance,40–44 yet these muscles were rarely targeted in the included studies. Future studies should continue to investigate the relationship of strength in lower extremity and trunk muscles to gait in people with MS because this would help better inform strength intervention trials. In addition, studies should provide rationale for their intervention choices and should consider strength training approaches that are more relevant to walking.
Many of the studies included in this review had small sample sizes, and very few performed sample size calculations. Although the primary objective of this review was not to evaluate the effectiveness of strength training on gait, it could be that the overall lack of power calculations and small sample sizes at least in part explain why there were not significant gait outcomes. However, the results of this review do support those of previous reviews that highlight the lack of consistently meaningful gait speed and endurance outcomes, even when gait and strength are improved significantly.12–16 In people with MS, change in T25FW time of at least 20% is considered meaningful.45 No study reported significant gait speed changes of 20% on the T25FW test, although Sangelaji et al32 reported changes in the 10-meter walk test distance that exceeded 20% in the primary resistance training group compared with controls. Gait speed does have the possibility of a floor effect, especially in people with MS who have lower disability,46 whereas gait endurance may have better responsiveness in people with MS.47 Clinically meaningful changes from the patient perspective after intervention have been reported to be 21.6 m on the 6MWT and 9.6 m on the 2MWT.47 Based on these criteria, four of the included studies reported potentially important changes in gait endurance.20 25 26 32
Strength training is one part of the recommended guidelines for physical activity and exercise in people with MS, along with aerobic training.11 Despite the current literature being inconclusive about the effects of strength training on gait, reductions in strength are consistently associated with gait dysfunction, and strength training still has the potential to be an important intervention to improve gait in people with MS. Overall, studies that included strength training as an intervention, either alone or combined with other interventions, tended to dose in a manner consistent with recommended guidelines. However, despite the strength improvements found in most included studies, very few studies reported potentially meaningful changes in gait. To address this, future studies should be adequately powered to detect changes in gait, continue to explore higher-intensity strength training, and examine the dose-response relationship of strengthening on gait outcomes. Finally, more trials are needed that investigate strength training in muscles other than the knee, and task-specific, functional approaches to intervention should be developed based on best available evidence and relevance to gait.
Limitations
Critical reviews often synthesize diverse sources of evidence rather than answering a clinical question, and this review included a heterogeneous group of studies, many of which included other interventions besides strength training. Importantly, some studies did not include strengthening as a primary intervention and were not powered to detect changes in strength or gait. Owing to this heterogeneity, a meta-analysis was not performed, and this is a limitation of this review. In addition, the inclusion of other interventions in addition to strength training also could have influenced results of individual trials, and improvements in those trials cannot be directly attributed solely to strength gains.
Another limitation was that the included studies applied the same strengthening intervention to participants regardless of baseline strength and disability level. It could be that for some participants strength, gait, or both was not sufficiently impaired, and, therefore, improvements were either not measurable or possible. Last, this review included only gait performance outcomes, and although that is one of the most important tasks for people with MS, it may be that strengthening has a different effect on other functional tasks important for mobility, including stairs, sit to stand, or dynamic gait. Other gait outcomes, such as self-report measures or direct measures of physical activity, might be more responsive to strengthening.
Conclusion
The studies included in this review generally showed improved strength, yet few reported potentially meaningful between-group changes in gait. Future strength intervention studies designed to improve gait might consider dosing beyond that of the minimum intensity to improve strength and exploring muscles targets, positions, and modes that are task-specific to walking.
PRACTICE POINTS
In studies that implemented strength training and measured gait outcomes, this review found a trend toward major improvement in strength outcomes but not in gait performance as measured by speed and endurance.
This review found that studies including strength training for people with MS, either alone or combined with other rehabilitation interventions, are typically prescribed in a manner consistent with current guidelines and can improve strength. However, to improve gait, future studies might consider exploring higher intensities or frequencies.
This review found that strength training exercises most often focused on the knee and were performed on weight machines in a sitting position. This may be a reason strength training has not resulted in consistent improvements in gait, and future studies are needed that investigate muscle targets, positions, and modes of exercise that are functionally relevant to gait.
Financial Disclosures
The authors declare no conflicts of interest.
References
Minden SL, Frankel D, Hadden L, Perloff J, Srinath KP, Hoaglin DC. The Sonya Slifka Longitudinal Multiple Sclerosis Study: methods and sample characteristics. Mult Scler. 2006;12:24–38.
Van Asch P. Impact of mobility impairment in multiple sclerosis 2: patients' perspectives. Eur Neurol Rev. 2011;6:115–120.
Asano M, Dawes DJ, Arafah A, Moriello C, Mayo NE. What does a structured review of the effectiveness of exercise interventions for persons with multiple sclerosis tell us about the challenges of designing trials? Mult Scler. 2009;15:412–421.
Pearson M, Dieberg G, Smart N. Exercise as a therapy for improvement of walking ability in adults with multiple sclerosis: a meta-analysis. Arch Phys Med Rehabil. 2015;96:1339–1348.e7.
Platta ME, Ensari I, Motl RW, Pilutti LA. Effect of exercise training on fitness in multiple sclerosis: a meta-analysis. Arch Phys Med Rehabil. 2016;97:1564–1572.
Padgett PK, Kasser SL. Exercise for managing the symptoms of multiple sclerosis. Phys Ther. 2013;93:723–728.
Khan F, Amatya B. Rehabilitation in multiple sclerosis: a systematic review of systematic reviews. Arch Phys Med Rehabil. 2017;98:353–367.
Mañago MM, Hebert JR, Schenkman M. Psychometric properties of a clinical strength assessment protocol in people with multiple sclerosis. Int J MS Care. 2017;19:253–262.
Hoang PD, Gandevia SC, Herbert RD. Prevalence of joint contractures and muscle weakness in people with multiple sclerosis. Disabil Rehabil. 2014;36:1588–1593.
Jørgensen M, Dalgas U, Wens I, Hvid LG. Muscle strength and power in persons with multiple sclerosis: a systematic review and meta-analysis. J Neurol Sci. 2017;376:225–241.
Latimer-Cheung AE, Martin Ginis KA, Hicks AL, et al. Development of evidence-informed physical activity guidelines for adults with multiple sclerosis. Arch Phys Med Rehabil. 2013;94:1829–1836.e7.
Cruickshank TM, Reyes AR, Ziman MR. A systematic review and meta-analysis of strength training in individuals with multiple sclerosis or Parkinson disease. Med (Baltimore). 2015;94:e411.
Latimer-Cheung AE, Pilutti LA, Hicks AL, et al. Effects of exercise training on fitness, mobility, fatigue, and health-related quality of life among adults with multiple sclerosis: a systematic review to inform guideline development. Arch Phys Med Rehabil. 2013;94:1800–1828.e3.
Snook EM, Motl RW. Effect of exercise training on walking mobility in multiple sclerosis: a meta-analysis. Neurorehabil Neural Repair. 2009;23:108–116.
Rietberg MB, Brooks D, Uitdehaag BM, Kwakkel G. Exercise therapy for multiple sclerosis. Cochrane Database Syst Rev. 2005;(1):CD003980.
Kjolhede T, Vissing K, Dalgas U. Multiple sclerosis and progressive resistance training: a systematic review. Mult Scler. 2012;18:1215–1228.
Dalgas U, Stenager E, Ingemann-Hansen T. Multiple sclerosis and physical exercise: recommendations for the application of resistance-, endurance- and combined training. Mult Scler. 2008;14:35–53.
Williams G, Kahn M, Randall A. Strength training for walking in neurologic rehabilitation is not task specific: a focused review. Am J Phys Med Rehabil. 2014;93:511–522.
Moher D, Shamseer L, Clarke M, et al. Preferred Reporting Items for Systematic Review and Meta-analysis Protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1.
Dalgas U, Stenager E, Jakobsen J, et al. Resistance training improves muscle strength and functional capacity in multiple sclerosis. Neurology. 2009;73:1478–1484.
Romberg A, Virtanen A, Ruutiainen J, et al. Effects of a 6-month exercise program on patients with multiple sclerosis: a randomized study. Neurology. 2004;63:2034–2038.
Broekmans T, Roelants M, Feys P, et al. Effects of long-term resistance training and simultaneous electro-stimulation on muscle strength and functional mobility in multiple sclerosis. Mult Scler. 2011;17:468–477.
Dodd KJ, Taylor NF, Shields N, Prasad D, McDonald E, Gillon A. Progressive resistance training did not improve walking but can improve muscle performance, quality of life and fatigue in adults with multiple sclerosis: a randomized controlled trial. Mult Scler. 2011;17:1362–1374.
Harvey L, Smith AD, Jones R. The effect of weighted leg raises on quadriceps strength, EMG parameters and functional activities in people with multiple sclerosis. Physiotherapy. 1999;85:154–161.
Kjolhede T, Vissing K, de Place L, et al. Neuromuscular adaptations to long-term progressive resistance training translates to improved functional capacity for people with multiple sclerosis and is maintained at follow-up. Mult Scler. 2015;21:599–611.
Manca A, Cabboi MP, Dragone D, et al. Resistance training for muscle weakness in multiple sclerosis: direct versus contralateral approach in individuals with ankle dorsiflexors' disparity in strength. Arch Phys Med Rehabil. 2017;98:1348–1356.e1.
Moradi M, Sahraian MA, Aghsaie A, et al. Effects of eight-week resistance training program in men with multiple sclerosis. Asian J Sports Med. 2015;6:e22838.
Eftekhari E, Mostahfezian M, Etemadifar M, Zafari A. Resistance training and vibration improve muscle strength and functional capacity in female patients with multiple sclerosis. Asian J Sports Med. 2012;3:279–284.
Frevel D, Mäurer M. Internet-based home training is capable to improve balance in multiple sclerosis: a randomized controlled trial. Eur J Phys Rehabil Med. 2015;51:23–30.
Hayes HA, Gappmaier E, LaStayo PC. Effects of high-intensity resistance training on strength, mobility, balance, and fatigue in individuals with multiple sclerosis: a randomized controlled trial. J Neurol Phys Ther. 2011;35:2–10.
Learmonth YC, Paul L, Miller L, Mattison P, McFadyen AK. The effects of a 12-week leisure centre-based, group exercise intervention for people moderately affected with multiple sclerosis: a randomized controlled pilot study. Clin Rehabil. 2012;26:579–593.
Sangelaji B, Kordi M, Banihashemi F, Nabavi SM, Khodadadeh S, Dastoorpoor M. A combined exercise model for improving muscle strength, balance, walking distance, and motor agility in multiple sclerosis patients: a randomized clinical trial. Iran J Neurol. 2016;15:111–120.
Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Inf Libr J. 2009;26:91–108.
Wernbom M, Augustsson J, Thomeé R. The influence of frequency, intensity, volume and mode of strength training on whole muscle cross-sectional area in humans. Sports Med Auckl NZ. 2007;37:225–264.
Van Abbema R, De Greef M, Craje C, Krijnen W, Hobbelen H, Van Der Schans C. What type, or combination of exercise can improve preferred gait speed in older adults? a meta-analysis. BMC Geriatr. 2015;15:72.
Kierkegaard M, Lundberg IE, Olsson T, et al. High-intensity resistance training in multiple sclerosis: an exploratory study of effects on immune markers in blood and cerebrospinal fluid, and on mood, fatigue, health-related quality of life, muscle strength, walking and cognition. J Neurol Sci. 2016;362:251–257.
Karpatkin HI, Cohen ET, Klein S, Park D, Wright C, Zervas M. The effect of maximal strength training on strength, walking, and balance in people with multiple sclerosis: a pilot study. Mult Scler Int. 2016;2016:5235971.
Thoumie P, Lamotte D, Cantalloube S, Faucher M, Amarenco G. Motor determinants of gait in 100 ambulatory patients with multiple sclerosis. Mult Scler. 2005;11:485–491.
Broekmans T, Gijbels D, Eijnde BO, et al. The relationship between upper leg muscle strength and walking capacity in persons with multiple sclerosis. Mult Scler. 2013;19:112–119.
Fritz NE, Marasigan RE, Calabresi PA, Newsome SD, Zackowski KM. The impact of dynamic balance measures on walking performance in multiple sclerosis. Neurorehabil Neural Repair. 2015;29:62–69.
Newsome SD, Wang JI, Kang JY, Calabresi PA, Zackowski KM. Quantitative measures detect sensory and motor impairments in multiple sclerosis. J Neurol Sci. 2011;305:103–111.
Wagner JM, Kremer TR, Van Dillen LR, Naismith RT. Plantarflexor weakness negatively impacts walking in persons with multiple sclerosis more than plantarflexor spasticity. Arch Phys Med Rehabil. 2014;95:1358–1365.
Zackowski KM, Wang JI, McGready J, Calabresi PA, Newsome SD. Quantitative sensory and motor measures detect change overtime and correlate with walking speed in individuals with multiple sclerosis. Mult Scler Relat Disord. 2015;4:67–74.
Freund JE, Stetts DM, Vallabhajosula S. Relationships between trunk performance, gait and postural control in persons with multiple sclerosis. NeuroRehabilitation. 2016;39:305–317.
Kieseier BC, Pozzilli C. Assessing walking disability in multiple sclerosis. Mult Scler. 2012;18:914–924.
Phan-Ba R, Pace A, Calay P, et al. Comparison of the timed 25-foot and the 100-meter walk as performance measures in multiple sclerosis. Neurorehabil Neural Repair. 2011;25:672–679.
Baert I, Freeman J, Smedal T, et al. Responsiveness and clinically meaningful improvement, according to disability level, of five walking measures after rehabilitation in multiple sclerosis: a European multicenter study. Neurorehabil Neural Repair. 2014;28:621–631.







