Publication
Research Article
International Journal of MS Care
A Qualitative Study of Exercise and Physical Activity in Adolescents with Pediatric-Onset Multiple Sclerosis
Author(s):
CME/CNE Information
To access the article, post-test, and evaluation online, go to http://www.cmscscholar.org.Activity Available Online:
The target audience for this activity is physicians, physician assistants, nursing professionals, and other health care providers involved in the management of patients with multiple sclerosis (MS).Target Audience:
Learning Objectives:
1) Describe perceived barriers to physical activity participation for adolescents with pediatric-onset multiple sclerosis (POMS).
2) Identify preferred components of an intervention targeting physical activity in adolescents with POMS
Accreditation Statement:

In support of improving patient care, this activity has been planned and implemented by the Consortium of Multiple Sclerosis Centers (CMSC) and Delaware Media Group. The CMSC is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
The CMSC designates this journal-based activity for a maximum of 0.75 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.Physician Credit
The CMSC designates this enduring material for 0.75 contact hour (none in the area of pharmacology).Nurse Credit
Disclosures:
Editor in Chief of the International Journal of MS Care (IJMSC), has served as physician planner for this activity. He has disclosed relationships with Springer Publishing (royalty), Biogen (speakers' bureau), and Adamas Pharmaceuticals (contracted research).Francois Bethoux, MD,
has served as reviewer for this activity. She has disclosed no relevant financial relationships.Laurie Scudder, DNP, NP,
has disclosed no relevant financial relationships.E. Morghen Sikes, MS OTR/L,
has disclosed no relevant financial relationships.Emma V. Richardson, PhD,
has disclosed no relevant financial relationships.Robert W. Motl, PhD,
The peer reviewer for IJMSC has disclosed no relevant financial relationships.
The staff at IJMSC, CMSC, and Delaware Media Group who are in a position to influence content have disclosed no relevant financial relationships.
Note: Financial relationships for some authors may have changed in the interval between listing these disclosures and publication of the article..
Method of Participation:
Release Date: April 1, 2019
Valid for Credit Through: April 1, 2020
In order to receive CME/CNE credit, participants must:
1) Review the continuing education information, including learning objectives and author disclosures.
2) Study the educational content.
3) Complete the post-test and evaluation, which are available at http://www.cmscscholar.org.
Statements of Credit are awarded upon successful completion of the post-test with a passing score of >70% and the evaluation.
There is no fee to participate in this activity.
This educational activity may contain discussion of published and/or investigational uses of agents that are not approved by the FDA. CMSC and Delaware Media Group do not recommend the use of any agent outside of the labeled indications. The opinions expressed in the educational activity are those of the faculty and do not necessarily represent the views of CMSC or Delaware Media Group.Disclosure of Unlabeled Use:
Participants have an implied responsibility to use the newly acquired information to enhance patient outcomes and their own professional development. The information presented in this activity is not meant to serve as a guideline for patient management. Any medications, diagnostic procedures, or treatments discussed in this publication should not be used by clinicians or other health-care professionals without first evaluating their patients' conditions, considering possible contraindications or risks, reviewing any applicable manufacturer's product information, and comparing any therapeutic approach with the recommendations of other authorities.Disclaimer:
Abstract
Background:
Pediatric-onset multiple sclerosis (POMS) accounts for up to 5% of all multiple sclerosis (MS) cases. Of note, the existing literature regarding physical activity and POMS is sparse, and there is limited insight about the lived experiences of individuals with POMS regarding physical activity, including perceptions of its benefits, barriers, facilitators, and promotion.
Methods:
We conducted a qualitative exploration of physical activity perceptions and experiences and of preferences for a physical activity intervention in eight persons with POMS. Using semistructured interviews and interpretative phenomenological analysis, we crafted numerous themes that provide new knowledge of physical activity experiences and preferences in this population.
Results:
The adolescent participants believed that physical activity would be beneficial and important but further believed that it can often be boring and may worsen POMS symptoms. Participants described adequate symptom management, social support, time, and opportunity as facilitators of physical activity, and lack of social support, time, and opportunity as hindrances. The interviewees described that components of a future intervention should focus on education regarding specific exercises, outcomes, and safety during exercise and provide opportunities for social engagement with other individuals with POMS.
Conclusions:
This qualitative study provides novel findings regarding the perceptions and experiences of physical activity in POMS. An important step in crafting an understanding of physical activity behavior in POMS, this study serves to inform the development and delivery of physical activity behavioral interventions.
Pediatric-onset multiple sclerosis (POMS) accounts for up to 5% of all multiple sclerosis (MS) cases1 and typically exhibits a relapsing-remitting clinical course. The condition manifests as sensory alterations, optic neuritis, brainstem signs (ie, double vision, weakness, ataxia), and/or changes in walking patterns.2 Individuals with POMS often present with mental and physical fatigue,3 cognitive impairment,4 5 and depression.6 Concerningly, POMS is associated with persistently higher relapse rates compared with adult-onset MS,7 8 and permanent disability occurs approximately 10 years earlier chronologically than with adult-onset MS.2 Such observations underscore the importance of early disease identification for initiating immediate medical treatment through disease-modifying therapies and therapeutic rehabilitation strategies.9
Physical activity has been identified as an important rehabilitation strategy for managing the manifestations of POMS.10 Physical activity is defined as any movement of the body based on skeletal muscle contraction resulting in a substantial increase in energy expenditure over resting levels.11 Of note, exercise is a specific, structured form of physical activity undertaken for improvement or maintenance of physical fitness. There is evidence that higher levels of physical activity are associated with lower T2 lesion volume, relapse rates, and fatigue in POMS.12 13 Unfortunately, there is evidence of low rates of physical activity participation in POMS (ie, approximately 10 min/d of moderate-to-vigorous physical activity),13 and those with POMS engage in less moderate-to-vigorous physical activity than controls14 and youth with other demyelinating conditions (ie, acute disseminated encephalomyelitis, monophasic acquired demyelinating syndrome).12 13 Some research suggests that self-efficacy and exercise goal setting are correlates of higher levels of physical activity, whereas functional disability is a correlate of lower levels of physical activity in POMS.13 15
To date, the existing literature provides a limited picture of physical activity in POMS and has relied solely on quantitative methods. Consequently, there is limited insight regarding experiential knowledge of physical activity and its perceived benefits, barriers, facilitators, and promotion in this subsection of MS. These gaps support the need for a qualitative inquiry to be conducted as an important step in crafting a broad, but indepth, understanding of physical activity in POMS that can inform the development and delivery of physical activity behavioral interventions.
The present study involved a qualitative exploration of physical activity in POMS. Such an exploration will allow us to build a comprehensive picture of current perceptions and experiences of this health behavior. Such a foundation will then allow for the creation and implementation of interventions targeting physical activity and exercise promotion relevant to older youth with POMS. To that end, the present study had two primary aims regarding older children and adolescents with POMS: 1) to improve our understanding of perceptions, beliefs, barriers, and facilitators regarding physical activity and 2) to identify preferred components of interventions targeting physical activity. To achieve the aims of this study, we sought to answer three research questions in a sample of individuals with POMS: What are common perceptions of physical activity? What are experiences with physical activity? What is required to implement an effective behavior change intervention targeting physical activity?
Methods
This study was approved by the institutional review board of the University of Alabama at Birmingham.
Philosophical Assumptions and Design
This research was guided by an interpretive phenomenological paradigm rooted in constructionist epistemology and relativist ontology. Interpretive phenomenology seeks to explore a phenomenon based on how it is perceived by individuals in a specific situation (ie, individuals diagnosed as having POMS and personal experiences related to physical activity and exercise) and further seeks to understand and interpret the phenomenon through shared knowledge and experiences.16 Constructionist epistemology posits that this knowledge is constructed through cultural, environmental, and social influences as opposed to created in the individual's mind,16 and relativist ontology stipulates that there are multiple realities and ways of understanding this knowledge.17
In addition, we chose interpretive phenomenological analysis in an effort to craft an empirical experiential foundation for driving forth interventions informed by older youth with POMS for older youth with POMS.
Sampling Procedure and Participants
To be included in this study, participants were required to be aged 10 to 17 years, have a clinical diagnosis of POMS, be fluent in English, be able to access or attend an interview, and agree to be recorded during this interview (participants and parents both agreed). Staff at a local POMS center acted as gatekeepers and compiled a list of eligible participants from the center's patient population. Eligible individuals received a flyer and an information sheet describing the study via the US Postal Service and were directed to contact researchers by phone if interested. The center identified 21 eligible children and adolescents with POMS.
Data Collection
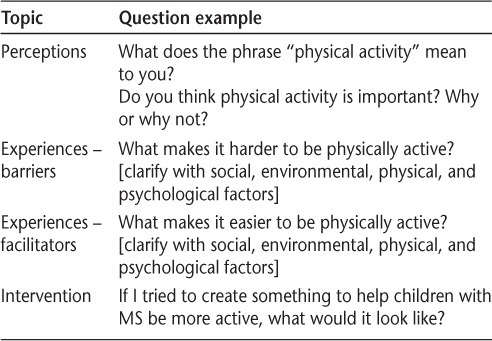
We used semistructured interviews to collect data. Semistructured interviews allow researchers to ensure that topics of interest are covered but permit participants freedom to discuss what is important and meaningful to them, thereby allowing participants to construct personal insights that constitute qualitative data.18 The flexibility of this method allowed us to alter the sequence of questions and probes to suit each participant, permitting each person to tell their own story.19 Interviews were completed online via video conferencing software (seven participants) or in person (one participant). The interview script consisted of 35 open-ended questions with a series of closed and open-ended probes for elaboration and clarification as necessary (Table 1). Occasionally, spontaneous probes were used to elicit additional information when scripted probes were inadequate. Informed consent was verbally obtained at the start of each interview with parents present. Participants had the opportunity to have parents involved in the interview, but all opted to have their parents step out. If the interview question was unclear, participants were encouraged to request rephrasing of the question for clarity. Questions were not phrased to be intrusive or uncomfortable, but participants were reminded of their right to refuse to answer any question and withdraw from the study at any time. Participants received a $25 gift card for participating. Interviews were transcribed by a professional transcription service unaffiliated with the investigators within 24 hours of interview completion. All identifying data were anonymized in line with ethical practice.
Examples of questions from interview
Data Analysis
Interpretative phenomenological analysis involves using an iterative and reciprocal hermeneutic circle.20 This involved first reading and rereading the transcribed interviews and making initial notes. After this step, the first author (E.M.S.) inductively crafted experiential themes and began to search for clusters that coherently reflected participants' experiences. The first author labeled these clusters based on participant-reported descriptors. After establishing these clusters, this author further identified superordinate groups and then categorized experiential group themes within the superordinate groups. Tables were created with organized lists including themes and original sources of thematic information. This stage involved connecting themes and attempting to harmonize interrelationships and organization of those themes. These tables evolved as this author continued to assess and interpret the experiential data. This author worked to identify convergent and divergent patterns in reported experiences from these themes and then revisited initial notes to confirm or reassess introductory thoughts and emergent themes. This circular development continued throughout the analysis process and was repeated for each interview transcript. After the analysis was completed, this author wrote up the themes and translated them into an intelligible and consistent realist tale of the common perceptions and experiences of physical activity and intervention preferences of participants diagnosed as having POMS.
Qualitative Rigor
The first author (E.M.S.) implemented a relativist approach to quality assessment.17 According to Smith and Caddick,21 there is an open-ended list of criteria for evaluating the rigor of qualitative research, and not all the components apply to all qualitative traditions. From this list, the researchers included substantive contribution, width, credibility, and transparency. We endeavored to substantially contribute to the knowledge base of exercise and physical activity research for youth with neurologic diseases (ie, POMS) by addressing a gap in knowledge concerning this population's experience with exercise. We addressed width by encouraging discussion and conversation to cover a wide range of topics regarding physical activity, including quotations from participants, as well as allowing interviews to end naturally without time pressures or suggestions to end. We addressed credibility by developing familiarity with the culture of the participants and by verbally reflecting on the meaning of participant answers during the interview. We maintained transparency by retaining an audit trail and by using a “critical friend” to analyze the research process and weigh in on interpretation of participant report.17
Results
Participants and Interviews
Of the 21 eligible individuals, parents of 11 of them made contact with the researchers and informed consent was completed for 8 adolescents to participate in the study. The mean age of participants was 15 (range, 14–17) years. All the participants were female and resided in Georgia (n = 3), Florida (n = 2), Alabama (n = 2), and Tennessee (n = 1). Disease duration ranged from less than 1 year to 5 years. See Table 2 for the sample's demographic information.
Demographic characteristics of sample
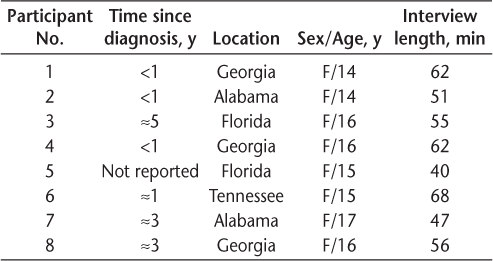
Overall, there were 441 recorded minutes of interviews. The interviews lasted 40 to 68 minutes (mean length, 55 minutes). This yielded 191 pages of transcribed interview data that were analyzed using interpretive phenomenological analysis.
After the application of interpretive phenomenological analysis, the following themes were crafted: 1) perceptions of physical activity and exercise, 2) experiences of physical activity, and 3) physical activity intervention preferences.
Perceptions of Physical Activity
Participants discussed both positive and negative perceptions regarding exercise and physical activity for POMS.
Positive Perceptions
All eight participants believed that physical activity yields positive outcomes, including management of POMS symptoms and prevention of secondary diseases. Participants reported learning about the benefits of physical activity from neurologists or family members (ie, a well-informed parent). Participant 4: “And my mom reads a bunch of stuff like MS studies online, she says that exercise is so important and it can really help, you know. So I think definitely, if there… there's a lot of risk being taken if you don't exercise, especially as you get older.”
The participants believed that physical activity helps manage POMS and its symptoms (ie, pain, stiffness, spasticity, lesion volume, and fatigue). Participant 8 stated, “It helps us get better and stuff like that, I mean it's not going to make our lesions go away, but it's going to help them like, start to like, decrease and stuff like that.”
The adolescents in this study further indicated the belief that physical activity improves mood and well-being. Participant 3 remarked, “I think if I stayed in bed, I would think of all the bad things about MS and not really getting up and actually enjoying the day. I would think about … I would go into depression again and I do not want that to happen. I'll get sad because I'm thinking of all the bad things that's happening, and I just do not like that at all.”
The participants believed that physical activity promotes a healthy body and prevents disease and comorbid conditions (ie, diabetes and obesity). Participant 4 said, “There's so many things that can go wrong if you're not physically active. I think the main things like diabetes, if you just eat way too much and you don't do anything about it.”
Bone health was mentioned by two participants. Both stated they were taking medications that caused bone deterioration and that a neurologist had suggested that light physical activity could counteract this adverse effect. These participants believed that physical activity would benefit bone health and maintain bone density. Participant 6 remarked, “The treatment is really strong that I'm on, and it's really havoc on my bones… they suggest lots of water, vitamin D to make my bones a lot stronger, and light exercising, extremely light exercising. Like, walking up the block and back, and maybe some jumping jacks and a light jog.”
Negative Perceptions
The most commonly described negative belief regarding physical activity was symptom worsening. The participants reported believing that exercise could cause worsening of symptoms and relapse. Pain, vision loss, headaches, sensory disturbances, and dizziness were the most commonly reported symptoms that adolescents with POMS believed may worsen after strenuous activity. This seemingly resulted in a common element of fear; participant 6: “[I] always get nervous that if I do too much, I'm going to end up in a relapse or something, so I haven't really researched on my own like how to work out correctly for MS.”
Several participants described physical activity as “boring” and “hard.” Participant 4 said, “It's hard. Because it's just easier to sit there and watch Netflix. Who wants… unless you somehow love that stuff, which I don't. My dad is a freak and somehow loves to exercise, but … I mean why go outside and run and lose your breath and get all sweaty when you can sit inside and eat chips in the air conditioning.”
Experiences of Physical Activity
Barriers
Barriers to physical activity were categorized into three primary groups: 1) POMS symptoms, 2) lack of social support, and 3) lack of opportunity and time (Figure 1).
Barriers to physical activity for youth with pediatric-onset multiple sclerosis
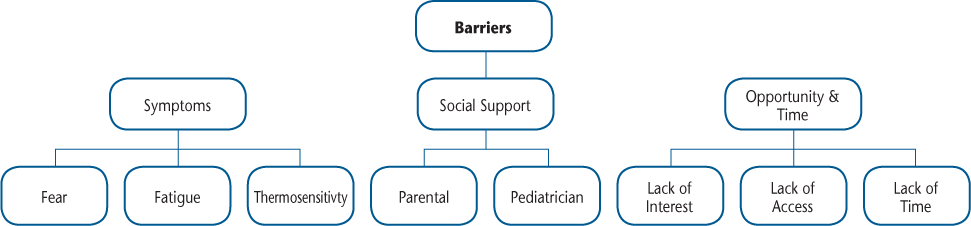
POMS Symptoms. As mentioned previously in the Results section, fear of inducing a relapse or worsening symptoms was identified as an influential barrier for physical activity in this group. The participants reported various POMS symptoms as barriers, and this reinforced the belief that physical activity worsens symptoms. Participant 6 stated, “After I've had treatment, it literally makes me feel like, if I try to walk on my own or without assistance or an aid, that all my bones in my body are going to snap or break.” Participant 8 remarked, “Weight lifting, I used to do it before I got diagnosed, but now I can't because I shake too badly, and I don't have grip inside my hand no more because of the numbness.”
All the participants stated that fatigue is a primary barrier to engagement in physical activity, and this included physical fatigue and mental or cognitive fatigue. Participant 5 noted, “I get tired. I always seem tired and I don't want to do anything.”
All eight participants reported thermosensitivity as a hurdle preventing adequate physical activity. Participant 6 said, “Because, when I'm in the sun, I get extremely hot, I get overheated, and I can't tolerate the sun at all. It affects my vision, and I can't do it anymore.”
Lack of Social Support. The lack of social support was a barrier for physical activity engagement among many of the participants. Some stated that having friends who were inactive reduced motivation to be active themselves. Participant 2 stated, “If I don't have anyone to talk to, why would I want to do something?”
Interestingly, three participants described parental involvement as a hindrance to physical activity, as parents prevented them from exercising due to fears of symptom worsening. Participant 4 said, “‘But I want to go outside, mom,’ and she's like ‘no you can't, I don't want anything happening, so.’” In one case, the participant's physician requested a reduction in exercise and physical activity due to fall risk. Participant 8: “My pediatrician told me to quit sports until they could find out what was going on. They kind of just said, they just told me to quit.”
Lack of Opportunity and Time. The perception of limited access to interesting and desirable activities interfered with physical activity engagement for the participants. Participant 4: “I really like lifting weights, but I'm not old enough to go to the gym or something, and I don't have any equipment at my house.”
Participants deemed lack of time to be a major barrier to exercise and physical activity. Participant 1 said, “At times, I feel like there's not enough time because school, I would say school and homework and stuff like that. I would say there's not enough time in a day.”
Facilitators
Facilitators to physical activity were categorized into three groups: 1) symptom management, 2) social support, and 3) opportunity (Figure 2).
Facilitators to physical activity for youth with pediatric-onset multiple sclerosis
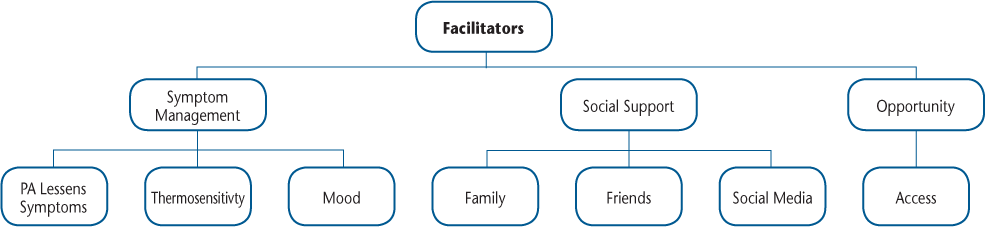
Symptom Management. Participants indicated that adequate management of thermosensitivity facilitated physical activity involvement. Participant 3: “Well, I have a cooling vest, and my mom buys this neck thing, you put it in water and it stays cool for hours. So, I put that around my neck. Lots of water, keep myself hydrated, and the park has water rides where you can cool off, so that's a plus as well. We try not to go at certain times, maybe we'll go in the morning, so when the sun is down a little bit or maybe at 7:00 to closing time so it won't be as hot for me.”
Some participants described physical activity as the most effective tool in managing POMS-related symptoms, as long as the participants recognized personal “limits” and stayed within individual ability levels. Again, participant 3: “If I stay in bed, it's more of drowsy, and if you stay in bed you're not moving your joints so they can get very, very stiff, and it gets painful. If I don't move my legs, or bend my legs, maybe every 30 minutes, they pop out of place. So, if I stay in bed, it actually gets worse when you're staying in bed than when you're actually up and moving.”
In addition, participants were more likely to engage in physical activity when it helped them manage, improve, or stabilize their mood, as many of them reported having difficulty maintaining a stable mood after diagnosis of POMS. Participant 8 remarked, “[Exercise] makes me feel good at the end of it, and even though I know that I'm like super tired, it lets me know that I can still do simple things. It makes me feel really good, like I can go climb like Mount Everest if I wanted to.”
Social Support. Social support played an important role in physical activity engagement for this group, as noted by all eight participants who reported that active friendships were helpful in encouraging physical activity behavior. Many participants indicated walking with friends as a time to engage in socializing and conversation. Participant 8 stated, “If friends were doing it with me and stuff like that. It doesn't really change it, but it's just a nice thing to be able to have somebody else.”
Active families encouraged physical activity, and adolescents with active parents or siblings reported engaging in more activity themselves, either with or without direct family involvement. Just as some participants reported parents or physicians as a hindrance to physical activity, there were some participants who reported that parents and physicians strongly encouraged activity participation. Participant 4 stated, “But for the past week or so, my mom has really pushed it because it's been a couple of months, haven't done anything, ‘get off your butt,’ so I started… I've been…I decided to do 20 minutes a day, I go out and play basketball.”
Support and encouragement via social media played an influential role in physical activity participation. Participant 3 said, “I use Instagram a lot, and exercise is one of the things that's mainly on my Discover page. That makes me want to do exercise more, because of that. I also have an [online] MS friend, and we are on a kind of challenge to lose a certain amount of weight by this certain time, so we kind of push each other like that.”
Opportunity. Having several facilities or spaces to be physically active facilitated involvement, such as sports at school or close living proximity to a gym or parks. Several participants reported living near a well-lit park or walking trail, and this encouraged them to engage in higher levels of physical activity, as did having access to a large yard or equipment at home (ie, basketball goal or swimming pool). Participant 4 said, “We have a huge front yard, so sometimes, especially during Thanksgiving, my brothers and my dad go out and play football… There's a lot of things around me to support exercising, so there's really no excuse.” Participant 6 remarked, “I like how there is multiple options, like if you don't feel like swimming today then you can get on the treadmill and you can walk, or you can do sit ups or crunches, or you can, there doesn't always have to be tied down to specifically one thing you can do to lose weight or get active.”
Physical Activity Intervention Preferences
Participants indicated a desire for an individualized approach to physical activity promotion. Participants described interest in a method of intervention that addressed personal, social, environmental, and physical needs (ie, a tailored intervention). Although this preference for individualization was commonly stated, similar themes emerged and can be categorized into two primary points: knowledge acquisition and social engagement (Figure 3).
Intervention preferences for youth with pediatric-onset multiple sclerosis
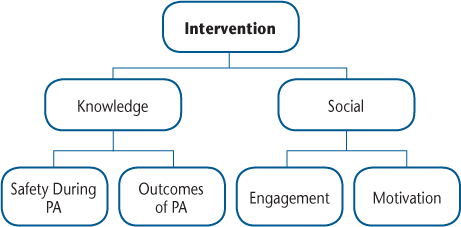
Knowledge Acquisition
The participants described an interest in learning about two particular concepts: 1) safe exercises for POMS and 2) outcomes of physical activity and exercise for POMS.
Knowledge of Specific Exercises. Participants described a desire to know specific exercises tailored to individuals with POMS. Participant 8: “Like, what things we could like, participant in that wouldn't like, tire us all the way out.”
Participants expressed a desire to learn more about safety during physical activity, especially regarding symptom management and prevention of symptom worsening. Participant 4 said, “I think it would be helpful to know [how to exercise safely] because there's probably information about how to be safe when there's nothing going on, but when you have multiple sclerosis, you probably should know like, the heat, or the pain, or something, try to prevent anything from happening.” Participant 6 noted, “I would love to know how to work out correctly for MS, so that I could like, when I'm in the YMCA, and I don't feel like swimming one day, and I feel like going in there and working out, how to do it correctly, for me. Without hurting myself or without ending up being in the hospital.”
Knowledge of Outcomes of Physical Activity and Exercise. Participants communicated an interest in learning and understanding outcomes of physical activity and exercise for individuals with POMS. Participant 4: “Definitely why it's good. That's like saying, ‘why should I do this worksheet if it's not going to be for a grade,’ so it's like…know definitely why is exercise important, and what can it do for MS or something.”
Social Engagement
Participants overwhelmingly thought that a group targeting physical activity and exercise should include other people with POMS:
Or other kids with MS, because you kind of have the same… even though it's terrible, you have something in common, you have the same goals in common, which is like, to get healthier. I think because if you can all relate on something, then you can become friends quicker and everything, and you get along better. [Why is it important to have friends with MS?] Because then you're not alone. Because it's not just you with some rare disease, and you don't know anybody else who's got it. (Participant 4)
[Who should be in the group?] MS people, obviously. And, just people close to my age, you know. Because it is… and even adults, just everyone who has MS who has never found the voice inside of them to speak up and say hey I have MS, yes I'm critically sick. And no, it doesn't define me but some days, it does. (Participant 6)
Discussion
This qualitative study investigated the perceptions and experiences of physical activity in older youth with POMS. We further examined preferences for a behavior change intervention targeting physical activity for POMS. The participants reported both positive and negative beliefs about physical activity and its benefits, experienced similar barriers and facilitators to physical activity, and described similar preferences for an intervention targeting physical activity.
The participants believed that physical activity would be beneficial and important for POMS. This aligns with a previous review stating that most youth believe that physical activity is important and that participation in physical activity can improve health and fitness.22 23 The participants further believed that physical activity can often be boring and may worsen their MS symptoms. Unfortunately, these negative beliefs are common in adolescents. Boredom was the most commonly reported barrier to physical activity for youth with cystic fibrosis,24 and other evidence indicates that healthy adolescent girls believed that physical activity was boring.25 26 This finding suggests that finding enjoyable methods for physical activity is essential to increasing activity engagement and inspiring lifelong habits of routine physical activity for children and adolescents.22 In addition, fear of symptom exacerbation is common in adults with MS.27 These beliefs and fears are valid, and steps must be taken to counteract the negative beliefs to increase levels of physical activity for POMS. To do so, adolescents must be able to identify activities of interest, recognize their activity limitations, and set activity goals that fall within those limitations. By facilitating engagement in enjoyable and achievable activities in the present, we lay the foundation for continued physical activity engagement throughout life.
Facilitators of physical activity were described as adequate symptom management, social support, time, and opportunity. Social support is frequently mentioned by adolescents, particularly girls, as a facilitator to physical activity.25 26 28–30 In addition to this commonly experienced facilitator, the group with POMS felt that symptom management strongly influenced their ability to participate in physical activity. In particular, symptoms of thermosensitivity and fatigue hindered physical activity and exercise. This is aligned with reports about adults with MS such that self-efficacy related to symptom management is associated with physical activity.31 For example, those with MS who managed their symptoms effectively also reported engaging in higher amounts of physical activity, and those who were inactive reported lower self-efficacy regarding symptom management. This information reflects the need for evidence-based strategies to increase self-efficacy relating to symptom management, and strategies to manage POMS symptoms, thus increasing ability to engage in physical activity.
Regarding perceived barriers, the interviewees described that symptoms of POMS and lack of social support, time, and opportunity hindered the ability to participant in adequate or desired amounts of physical activity. Other qualitative inquiries reflect that healthy teenagers perceive barriers similar to those reported by this sample (ie, mood, tiredness, lack of free time, lack of access to activities).32 33 In addition to these, the present sample identified POMS-related symptoms (ie, fatigue, mood, thermosensitivity, sensory alterations) as a major barrier to physical activity. This finding is aligned with previous research investigating barriers to physical activity in youth with cystic fibrosis such that cystic fibrosis symptoms hindered physical activity.24 Adults with MS report that symptoms, particularly fatigue and thermosensitivity, strongly influence physical activity engagement.27 34 Researchers and clinicians must adequately address disease-specific symptoms in addition to those experienced by the general population to support and motivate physical activity for individuals with POMS. Furthermore, the fear of difficulty initiating a physical activity program acted as a barrier to participation. For example, some of the participants thought that they would injure themselves by initiating an exercise program above their current level of ability. This aligns with previous research suggesting that perceived skill and ability along with perceptions of mastery influenced physical activity engagement for healthy adolescents.32 35 Researchers and clinicians should articulate that physical activity does not require strenuous movement or pain and can be started moderately and increased as tolerance improves. We suggest the development of guidelines for exercise in POMS to ensure safety and improve knowledge related to building exercise tolerance.
The interviewees described that components of a future intervention should focus on education regarding specific exercises, outcomes, and safety during exercise and provide opportunities for social engagement with other individuals with POMS. Indeed, the participants valued support and interaction with other youth with POMS when considering an exercise program. This aligns with previous research with adults with MS in that participants reported that socializing with others with MS was beneficial and enjoyable.34 36 Other research further supports this notion, with individuals with muscular dystrophy, MS, motor neuron disease, and Parkinson disease reporting that they preferred exercising with people with the same or other disabilities.37 Owing to the rarity of POMS, distance is often a significant barrier to creating and maintaining these relationships. A Web-based intervention with individuals diagnosed as having POMS could facilitate these desirable relationships among youth.
Limitations
Participant response bias (ie, presentation bias) represents one potential limitation and may have resulted in exaggerated or underestimated reports of experiences related to physical activity. The interviewer discussed this concern before the start of each interview and assured the participant that there is no right answer, and further provided verbal support and encouragement for participant responses regardless of response. The small sample size may be considered a limitation in some qualitative methods, but interpretative phenomenological analysis is an analytical technique that involves a close, rich, indepth examination of each case. As such, sample sizes are typically ten or fewer and purposively homogeneous to allow researchers to note convergence and divergence across participant accounts.18
Some qualitative methods posit member checking and peer debriefing as primary strategies for assessing rigor, but our epistemological position states that knowledge is crafted within the relationship developed by the researcher and the participants and, furthermore, that reality is multiple and subjective rather that one unifying truth. Thus, member checking with participants or cross-checking with colleagues (ie, peer debriefing) goes against our epistemological and ontological position. Instead, we implemented a relativist approach to quality assessment that aligned with our positions of a relativist ontology and constructionist epistemology.
Future Research
The present results paint an important picture and map for future research. We believe that these data support the following important research directions. There is a need for evidence-based strategies to increase self-efficacy relating to symptom management and strategies to manage POMS symptoms, thus increasing engagement in physical activity. Steps should be taken to counteract negative beliefs to increase levels of physical activity for POMS. To do so, adolescents should be able to identify activities of interest, recognize activity limitations, and set activity goals that fall within those limitations. By facilitating engagement in enjoyable and achievable activities in the present, we lay the foundation for continued physical activity engagement throughout life. Researchers and clinicians should adequately address disease-specific symptoms in addition to those experienced by the general population to fully motivate those with POMS to engage in physical activity. Future interventions targeting physical activity should focus on described barriers and beliefs in addition to the requested information relating to specific exercises, outcomes of physical activity, and safety during physical activity, as well as highlighting the requested social engagement in youth with POMS.
Conclusion
Collectively, the group of adolescents with MS described herein provided rich information, permitting a deeper understanding of the lived experience and perception of physical activity, along with information regarding preferences and desires for a future intervention targeting physical activity. This information will be essential for targeting physical activity as a health behavior for optimizing quality of life and participation among persons with POMS.
PRACTICE POINTS
There is increasing focus on health behaviors, particularly physical activity, in pediatric-onset MS (POMS) yet little understanding of approaches for changing physical activity levels.
Adolescents with POMS in this study reported that physical activity would be important and beneficial but further believed that it is often boring and may worsen POMS symptoms. They described social support, symptom management, time, and opportunity as factors influencing physical activity engagement.
Future interventions should take steps to counteract negative beliefs, reaffirm positive beliefs, and facilitate engagement in enjoyable and achievable activities for youth with POMS.
Acknowledgments
The authors thank the research staff at the Center for Pediatric Onset Demyelinating Disease for acting as gatekeepers and facilitating recruitment of the participants.
References
Chitnis T, Glanz B, Jaffin S, Healy B. Demographics of pediatric-onset multiple sclerosis in an MS center population from the northeastern United States. Mult Scler. 2009;15:627–631.
Boiko A, Vorobeychik G, Paty D, Devonshire V, Sadovnick D. Early onset multiple sclerosis: a longitudinal study. Neurology. 2002;59:1006–1010.
Carroll S, Chalder T, Hemingway C, Heyman I, Moss-Morris R. “It feels like wearing a giant sandbag”: adolescent and parent perceptions of fatigue in paediatric multiple sclerosis. Eur J Paediatr Neurol. 2016;20:938–945.
MacAllister WS, Belman AL, Milazzo M, et al. Cognitive functioning in children and adolescents with multiple sclerosis. Neurology. 2005;64:1422–1425.
MacAllister WS, Boyd JR, Holland NJ, Milazzo MC, Krupp LB. The psychosocial consequences of pediatric multiple sclerosis. Neurology. 2007;68(suppl 2):S66–S69.
Parrish JB, Weinstock-Guttman B, Smerbeck A, Benedict RH, Yeh EA. Fatigue and depression in children with demyelinating disorders. J Child Neurol. 2013;28:713–718.
Gorman MP, Healy BC, Polgar-Turcsanyi M, Chitnis T. Increased relapse rate in pediatric-onset compared with adult-onset multiple sclerosis. Arch Neurol. 2009;66:54–59.
Benson LA, Healy BC, Gorman MP, et al. Elevated relapse rates in pediatric compared to adult MS persist for at least 6 years. Mult Scler Relat Disord. 2014;3:186–193.
Kavaliunas A, Manouchehrinia A, Stawiarz L, et al. Importance of early treatment initiation in the clinical course of multiple sclerosis. Mult Scler. 2017;23:1233–1240.
Yeh EA, Kinnett-Hopkins D, Grover SA, Motl RW. Physical activity and pediatric multiple sclerosis: developing a research agenda. Mult Scler. 2015;21:1618–1625.
Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 1985;100:126–131.
Grover SA, Aubert-Broche B, Fetco D, et al. Lower physical activity is associated with higher disease burden in pediatric multiple sclerosis. Neurology. 2015;85:1663–1669.
Grover SA, Sawicki CP, Kinnett-Hopkins D, et al. Physical activity and its correlates in youth with multiple sclerosis. J Pediatr. 2016;179:197–203.e2.
Kinnett-Hopkins D, Grover SA, Yeh EA, Motl RW. Physical activity in pediatric onset multiple sclerosis: validating a questionnaire for clinical practice and research. Mult Scler Relat Disord. 2016;10:26–29.
Sawicki C, Grover S, Kinnett-Hopkins D, et al. Self-efficacy and functional disability as barriers to physical activity participation in pediatric multiple sclerosis (P4.023). Neurology. 2015;84(suppl):P4.023.
Burr V. Social Constructionism. 3rd ed. New York, NY: Routledge; 2015.
Smith B, Sparkes AC. Qualitative Research Methods in Sport, Exercise and Health: From Process to Product. New York, NY: Routledge; 2013.
Smith JA. Interpretive phenomenological analysis in sport and exercise: getting at experience. In: Smith B, Sparkes A, eds. Routledge Handbook of Qualitative Research in Sport and Exercise. New York, NY: Routledge; 2016:219–229.
Gratton C, Jones I. Analyzing Data II: Qualitative Data Analysis, Research Methods for Sport Studies. New York, NY: Routledge; 2004:217–227.
Rapport F, Wainwright P. Phenomenology as a paradigm of movement. Nurs Inquiry. 2006;13:228–236.
Smith B, Caddick N. Qualitative methods in sport: a concise overview for guiding social scientific sport research. Asia Pac J Sport Soc Sci. 2012;1:60–73.
Borra ST, Schwartz N, Spain CG, Natchipolsky M. Food, physical activity, and fun: inspiring America's kids to more healthful lifestyles. J Am Diet Assoc. 1995;95:816–823.
Rees R, Kavanagh J, Harden A, et al. Young people and physical activity: a systematic review matching their views to effective interventions. Health Educ Res. 2006;21:806–825.
Swisher AK, Erickson M. Perceptions of physical activity in a group of adolescents with cystic fibrosis. Cardiopulm Phys Ther J. 2008;19:107–113.
Mabry IR, Young DR, Cooper LA, et al. Physical activity attitudes of African American and white adolescent girls. Ambulatory Ped. 2003;3:312–316.
Whitehead S, Biddle S. Adolescent girls' perceptions of physical activity: a focus group study. Eur Phys Educ Rev. 2008;14:243–262.
Kayes NM, McPherson KM, Taylor D, Schlüter PJ, Kolt GS. Facilitators and barriers to engagement in physical activity for people with multiple sclerosis: a qualitative investigation. Disabil Rehabil. 2011;33:625–642.
Moore JB, Jilcott SB, Kindal A, et al. A qualitative examination of perceived barriers and facilitators of physical activity for urban and rural youth. Health Educ Res. 2010;25:355–367.
Saxena R, Borzekowski DLG, Rickert VI. Physical activity levels among urban adolescent females. J Pediatr Adolesc Gynecol. 2002;15:279–284.
Springer AE, Kelder SH, Hoelscher DM. Social support, physical activity and sedentary behavior among 6th-grade girls: a cross-sectional study. Int J Behav Nutr Phys Activity. 2006;3:8.
Plow MA, Resnik L, Allen SM. Exploring physical activity behaviour of persons with multiple sclerosis: a qualitative pilot study. Disabil Rehabil. 2009;31:1652–1665.
Humbert ML, Chad KE, Spink KS, et al. Factors that influence physical activity participation among high- and low-SES youth. Qual Health Res. 2006;16:467–483.
Thompson AM, Rehman LA, Humbert ML. Factors influencing the physically active leisure of children and youth: a qualitative study. Leisure Sci. 2005;27:421–438.
Learmonth YC, Marshall-McKenna R, Paul L, Mattison P, Miller L. A qualitative exploration of the impact of a 12-week group exercise class for those moderately affected with multiple sclerosis. Disabil Rehabil. 2013;35:81–88.
Parish LE, Treasure DC. Physical activity and situational motivation in physical education: influence of the motivational climate and perceived ability. Res Q Exerc Sport. 2003;74:173–182.
Dodd KJ, Taylor NF, Denisenko S, Prasad D. A qualitative analysis of a progressive resistance exercise programme for people with multiple sclerosis.. Disabil Rehabil. 2006;28:1127–1134.
Dawes H, Barker K, Bateman J, et al. Long-term Individual Fitness Enablement (LIFE) study: report to the Department of Health. http://anthonytravis.biz/ltnc/download_files/final%20reports/LIFE_Study_SUMMARY.pdf. Published November 2010. Accessed December 5, 2018.







