Publication
Research Article
Incorporation and Impact of a Clinical Pharmacist in a Hospital-Based Neurology Clinic Treating Patients with Multiple Sclerosis
Author(s):
Abstract
Background:
Clinical pharmacists are uniquely positioned to assist with the complexities of medication management for patients with multiple sclerosis (MS). The objective was to describe clinical pharmacy services provided, as well as provider satisfaction with and perceived impact of incorporating a clinical pharmacist in MS patient care.
Methods:
The study consisted of a retrospective medical record review and a provider survey conducted in an outpatient neurology clinic at an academic medical center. Between April 2017 and June 2018, electronic medical records of patients with documented interventions by a pharmacist were reviewed to describe clinical pharmacy services provided to patients with MS. A voluntary, anonymous survey was distributed to neurology providers to evaluate provider satisfaction with and perceived impact of clinical pharmacist involvement in MS patient care.
Results:
There were 64 patients identified with 378 documented interventions made by clinical pharmacists. Pharmacist interventions were mostly related to facilitating medication access (n = 208), pretreatment screening (n = 57), patient counseling (n = 51), and providing drug information (n = 43). All nine providers surveyed indicated that facilitating medication access, counseling patients, and managing drug interactions were moderately or very important clinical pharmacy services. Furthermore, all providers surveyed strongly agreed that pharmacist involvement decreased time to therapy initiation and provider time spent on medication management.
Conclusions:
Clinical pharmacists play an integral role in MS patient care, particularly with facilitating medication access. Prospective studies are needed to further evaluate the contribution of clinical pharmacists in MS patient care.
Multiple sclerosis (MS) is a complex neurologic disease that affects approximately 2.3 million patients worldwide.1 In the past decade, numerous disease-modifying therapies (DMTs) have been developed and have expanded MS treatment options. The DMTs reduce the number and severity of relapses, with the goal of delaying the development of disability. The American Academy of Neurology (AAN) provides guidance on which medications to consider for treatment, but the choice of therapy is ultimately determined by patient-specific factors. Thus, the AAN recommends that newly diagnosed patients have a dedicated provider visit to discuss specific treatment options.2
Advancements in treatment options for MS have drastically increased the time providers must allocate to medication management.3,4 Most DMTs are classified as specialty medications because of their cost, medication access restrictions, specialized administration training, and requirements for ongoing monitoring. With the cost of DMTs increasing at an exponential rate, coverage denials are occurring more frequently, often requiring multiple steps for medication approval.4 In addition to navigating through medication access materials, patient-specific drug interactions and comorbid conditions must be considered to ensure optimal use. These challenges take away valuable time that neurology providers spend on patient care activities and create a barrier to medication adherence.5 The complexity of this process and the substantial amount of time required for medication management necessitates the involvement of a medication expert, such as a clinical pharmacist, in MS patient care.3,5
Historically, there was no formal process dedicated to medication therapy management for patients with MS seen at the Grady Health System (GHS) neurology clinic (Atlanta, GA). Neurology providers rotated through the clinic on a biweekly basis. As a result, medication access requests or materials would go unaddressed until their next scheduled clinic day, leading to delays in treatment initiation for patients. Furthermore, due to significant patient volumes, follow-up visits were delayed for several months after the initial clinic visit. In 2017, clinical pharmacists were introduced into the GHS neurology clinic to overcome this barrier in patient care. This study aimed to evaluate the services provided by clinical pharmacists for patients with MS in an urban, academic, ambulatory care center as well as physicians’ perceptions of and satisfaction with a clinical pharmacist in this setting.
Methods
Study Design and Setting
This study was conducted in two parts: a retrospective medical record review and a provider survey conducted at a public academic health system that provides care to a largely underserved population in the Atlanta, Georgia, area. The study was approved by the institutional review board at Emory University (Atlanta) and the Research Oversight Committee at GHS, and a waiver of informed consent was granted for the medical record review.
The multidisciplinary team at the GHS neurology clinic consisted of an attending physician, medical residents, two nurse practitioners, and a clinical pharmacist as of 2017. Five clinical pharmacists staffed the neurology clinic on a rotating basis. Responsibilities of the clinical pharmacist included both direct and indirect patient care activities. Neurology providers could refer patients for evaluation by a clinical pharmacist for treatment initiation or follow-up monitoring. On receiving the referral, the clinical pharmacist screened the patient to determine whether they could be managed via a telephone encounter or required an in-person clinic visit. In these encounters, clinical pharmacists could order and review pretreatment tests, assess the patient for adverse effects, and educate patients about their medication and disease state. If necessary, the clinical pharmacist resolved any medication access barriers and coordinated therapy initiation or continuation for clinic-administered medications. If problems with the patient’s treatment regimen arose, the clinical pharmacist contacted the neurology provider to discuss alternative treatment options. In addition, neurology providers informally consulted the clinical pharmacist for assistance with medication access materials, recommendations for therapy initiation or modification, and advice regarding drug interaction or adverse effect management. The clinical pharmacist also served as an accessible drug information resource to patients and providers and communicated with specialty pharmacies to facilitate medication access for patients.
Data Collection
Retrospective medical record review was used to describe the roles and responsibilities of the clinical pharmacist in MS patient care. All patients seen in the neurology clinic for MS management between April 1, 2017, and June 1, 2018, with documented interventions by a clinical pharmacist were included. Interventions were documented in patient electronic medical records as either direct patient care (clinic or telephone encounters) or indirect patient care. Interventions were placed into one of five categories: facilitating medication access, pretreatment screening, patient counseling, providing drug information, or other. The total number of clinical pharmacist interventions as well as the average number of interventions per patient in direct patient care encounters were recorded.
Provider Survey
A descriptive survey was developed by the authors to evaluate provider satisfaction with and perceived impact of incorporating a clinical pharmacist in MS patient care. The survey modeled previous studies assessing similar outcomes.6–8 A total of 17 questions were included, seven assessing providers’ perceived impact of the clinical pharmacist on patient care and ten assessing providers’ satisfaction with the clinical pharmacist (Table S1, published in the online version of this article at ijmsc.org). Both sections of the survey used a Likert-like scale for responses. The survey was advertised to all neurology providers via e-mail, during clinic, and during departmental meetings and was active for 30 days.
The survey targeted anonymous, voluntary responses from current providers in the GHS neurology clinic. Responses from providers not practicing in the neurology clinic before the incorporation of a clinical pharmacist were excluded. All participants provided written informed consent before survey completion. All researchers remained blinded to the survey participants.
Outcomes
The primary outcomes of this study were the number and type of clinical pharmacist interventions provided to patients with MS seen in an outpatient hospital neurology clinic and provider satisfaction with and perceived impact of incorporating a clinical pharmacist in MS patient care. Results are reported in a descriptive manner without the use of statistical tests.
Results
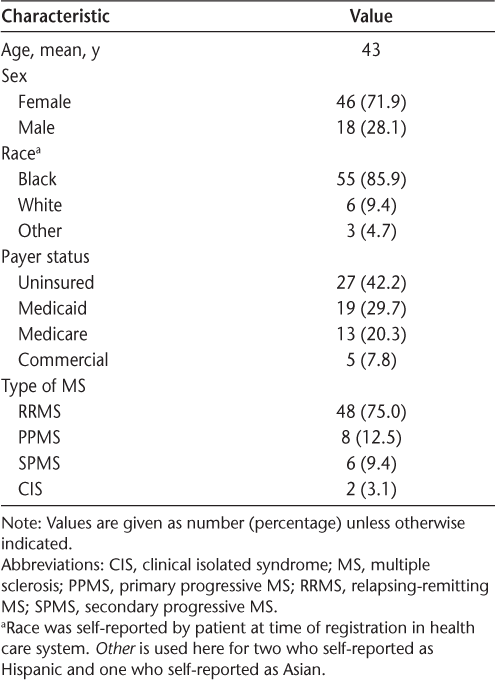
Demographic and clinical characteristics of the patients evaluated are shown in Table 1. Overall, 64 patients seen for MS management in the neurology clinic had a documented clinical pharmacist intervention during the study period. Most patients were female (71.9%) and Black (85.9%), and the most common type of MS was relapsing-remitting MS (75.0%). Twenty-seven patients (42.2%) were uninsured. For the provider survey, 13 survey responses were received. Of these, four were excluded because the provider was not present in the neurology clinic before incorporating a clinical pharmacist. Nine total survey responses were included from three attending physicians, two medical fellows, three medical residents, and one nurse practitioner.
Demographic and clinical characteristics of the 64 patients evaluated
Clinical Pharmacy Services Provided to Patients with MS
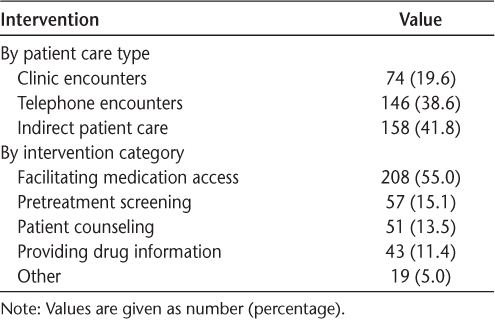
Of 378 documented interventions made by clinical pharmacists, 220 (58.2%) were made through direct patient care encounters, with an average of three to four interventions made per patient (Table 2). Facilitating medication access accounted for more than half of the pharmacist interventions (55.0%), which included activities such as completing prior authorizations for insured patients or patient assistance program applications for uninsured patients, recommending DMT modification based on patient coverage, contacting the patient to ensure that the necessary medication access materials have been completed, or communicating with the patient’s specialty pharmacy. Fifty-seven interventions (15.1%) involved pretreatment screening, including laboratory monitoring, medication review for drug or disease state interactions, and conducting prenatal or immunization screening. Providing patient counseling (13.5%) and serving as a drug information resource to patients and providers (11.4%) were other common interventions made by clinical pharmacists (Table 2).
Description of the 378 clinical pharmacist interventions
Provider Perceived Impact of Clinical Pharmacy Services on MS Patient Care
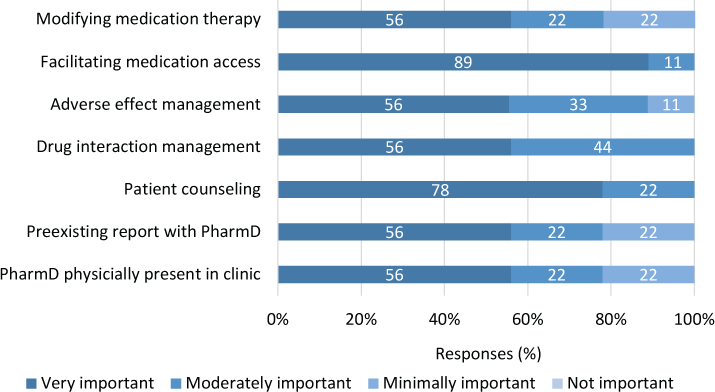
All providers surveyed reported that facilitating medication access, managing drug interactions, and providing patient counseling were moderately or very important services provided by clinical pharmacists in MS patient care (Figure 1). Providers indicated that the most impactful clinical pharmacy service provided to patients was facilitating medication access, with 89% of providers indicating that this was very important to patient care. No services evaluated were deemed not important to MS patient care. However, 22% of providers indicated that having a preexisting rapport with the clinical pharmacist before their involvement and having the pharmacist physically present in the clinic was of minimal importance to clinical pharmacy impact.
Provider perceived impact of clinical pharmacist involvement (n = 9)
Provider Satisfaction with Clinical Pharmacy Services
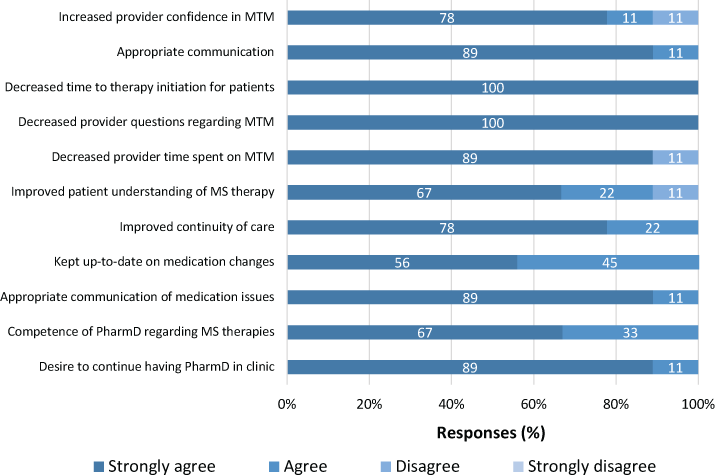
All providers strongly agreed that involving a clinical pharmacist in MS patient care decreased the number of questions they received regarding medication management and decreased time to therapy initiation (Figure 2). In addition, providers agreed or strongly agreed that the clinical pharmacist was competent in selecting treatment options and improved continuity of care for their patients. All providers surveyed reported that they desired to continue having clinical pharmacist assistance with their patients with MS.
Provider satisfaction with clinical pharmacist involvement (n = 9)
Discussion
Specialty medications, such as DMTs used in MS treatment, are associated with increased clinical complexity. As a result, a high level of care must be dedicated to medication therapy management for patients with MS. Disease and specialty care management programs aimed at improving medication adherence, disease awareness, and adverse effect management for patients with MS have been described previously in the literature.3,9–11 Studies evaluating the effects of these programs have found that pharmacists and support staff working in specialty pharmacies lead to improved adherence to MS treatment regimens.3,9,11 However, these studies included an integrated specialty pharmacy model that requires substantial time and resources to build that may not be feasible for all health care systems. Furthermore, most patients included in these studies had functional prescription insurance coverage. In addition to financial barriers in obtaining medications for uninsured patients, these patients face socioeconomic factors that affect health care quality. In a survey conducted by Iezzoni and colleagues,12 36.8% of uninsured patients reported having never taken their MS medications compared with 21.2% with health insurance. The findings from this study are unique because they describe clinical pharmacy services provided to a largely uninsured patient population with MS in a hospital-based setting without an integrated specialty pharmacy. Furthermore, this study provides insight into the role of a clinical pharmacist directly integrated into a multidisciplinary team of providers in a neurology clinic.
This study is the first, to our knowledge, to evaluate clinical pharmacy services provided in MS patient care as well as provider satisfaction with and perceived impact of clinical pharmacist involvement. Because of the underserved patient population at our institution, facilitating medication access accounted for most pharmacist interventions, which likely contributed to the decreased time to therapy initiation for patients reported by providers. Pretreatment screening, including laboratory monitoring and initial patient assessment, also accounted for a significant amount of pharmacist interventions, as did patient counseling and serving as a drug information resource. Providers felt that clinical pharmacist involvement was an important part of MS patient care, particularly facilitating medication access, providing patient counseling, and managing drug interactions. Overall, providers were satisfied with clinical pharmacist involvement and desired to continue to have a pharmacist in the neurology clinic.
There are several limitations of this study that warrant consideration. To gain a clear assessment of providers’ opinions of clinical pharmacy services, we included only providers who were present both before and after incorporating a clinical pharmacist. This resulted in a small sample size of providers surveyed who were familiar with a small sample of specific clinical pharmacists at our institution, which could have resulted in some bias in survey responses. Although the survey was based on previous studies evaluating similar outcomes,6–8 there was no formal process followed in survey development, and the customized nature of the survey tool may not be generalizable to other institutions. Second, we were able to capture only interventions that were documented in the electronic medical records of patients seen in the neurology clinic. Time constraints limiting documentation of interventions may have resulted in an under-representation of services provided. Finally, because of the retrospective nature of this study, future prospective studies are needed to evaluate the effect of clinical pharmacists on cost savings, patient satisfaction, and medication adherence.
In conclusion, involving a medication expert such as a clinical pharmacist in the multidisciplinary care of patients with MS is necessary to achieve optimal patient outcomes. Clinical pharmacists serve as patient advocates by facilitating medication access and providing counseling. They also decrease provider workload by serving as easily accessible drug information resources. Providers report high satisfaction with pharmacist involvement in MS patient care and perceive that clinical pharmacy services have a positive effect in this setting.
PRACTICE POINTS
Due to the complexity of medications used in MS treatment, clinical pharmacists play an integral role in the multidisciplinary team by facilitating medication access, providing patient education and follow-up monitoring, and serving as a drug information resource for neurology providers.
Neurology providers in this study reported high satisfaction with clinical pharmacist involvement and perceived that clinical pharmacists had a positive effect on MS patient care.
Financial Disclosures
The authors declare no conflicts of interest.
References
National Multiple Sclerosis Society. What is MS? Accessed December 14, 2018. http://www.nationalmssociety.org/about-multiple-sclerosis/index.aspx
Rae-Grant A, Day GS, Marrie RA, . Practice guideline: disease-modifying therapies for adults with multiple sclerosis: report of the guideline development, dissemination, and implementation subcommittee of the American Academy of Neurology. Neurology. 2018; 90: 777– 788.
Hanson RL, Habibi M, Khamo N, . Integrated clinical and specialty pharmacy practice model for management of patients with multiple sclerosis. Am J Health Syst Pharm. 2014; 71: 463– 469.
Hartung DM, Bourdette DN, Ahmed SM, . The cost of multiple sclerosis drugs in the US and the pharmaceutical industry: too big to fail? Neurology . 2015; 84: 2185– 2192.
Anderson SS, Philbrick AM. Improving multiple sclerosis care: an analysis of the necessity for medication therapy management services among the patient population. J Manag Care Spec Pharm. 2014; 20: 254– 261.
Pezzino NC, Marciniak MW, Smith MG, . Physician-reported factors that encourage collaboration with community pharmacists. J Am Pharm Assoc. 2017; 57( 3S): S279– S283.e2.
Splawski J, Horner D, Tao K. A survey of staff perceptions of an emergency medicine pharmacist program in a community hospital: a brief report. Ann Emerg Med. 2017; 69: 308– 314.
Truong H, Kroehl ME, Lewis C, . Clinical pharmacists in primary care: provider satisfaction and perceived impact on quality of care provided. SAGE Open Med. 2017; 5: 1– 9.
Groeneweg M, Forrester SH, Arnold B, . One-year outcomes of an integrated multiple sclerosis disease management program. J Manag Care Spec Pharm. 2018; 24: 458– 463.
Tan H, Yu J, Tabby D, . Clinical and economic impact of a specialty care management program among patients with multiple sclerosis: a cohort study. Mult Scler. 2010; 16: 956– 963.
DuChane J, Clark B, Staskon F, Miller R, Love K, Duncan I. Walgreens Connected Care: impact of managed therapy on adherence to medications used to treat multiple sclerosis and related comorbid conditions. Int J MS Care. 2015; 17: 57– 64.
Iezzoni LI, Ngo LH, Kinkel RP. Working-age persons with multiple sclerosis and access to disease-modifying medications. Mult Scler. 2007; 13: 534– 546.







