Publication
Research Article
International Journal of MS Care
Addressing Physical Activity Behavior in Multiple Sclerosis Management
Abstract
Background:
Although physical activity (PA) is considered the most important nonpharmaceutical intervention for persons with multiple sclerosis (MS), less than 20% of people with MS are engaging in sufficient amounts to accrue benefits. Promotion of PA is most effective when combined with additional behavior change strategies, but this is not routinely done in clinical practice. This study aimed to increase our understanding of current practice and perspectives of health care providers (HCPs) in Canada regarding their use of interventions to address PA behavior in MS management. Investigating HCPs’ perspectives on implementing PA behavior change with persons with MS will provide insight into this knowledge-to-practice gap.
Methods:
Semistructured focus groups were conducted with 31 HCPs working with persons with MS in Saskatchewan, Canada. Based on interpretive description, data were coded individually by three researchers, who then collaboratively developed themes. Analysis was inductive and iterative; triangulation and member reflections were used.
Results:
Five themes were established: 1) prescribing, promoting, and impacting wellness with PA; 2) coordinating communication and continuity in practice; 3) timely access to relevant care: being proactive rather than reactive; 4) enhancing programming and community-based resources; and 5) reconciling the value of PA with clinical practice.
Conclusions:
The HCPs value PA and want more support with application of behavior change strategies to deliver PA behavioral interventions, but due to the acute and reactive nature of health care systems they feel this cannot be prioritized in practice. Individual- and system-level changes are needed to support consistent and effective use of PA behavioral interventions in MS.
There is growing evidence for the benefits,1 safety,2 and importance of being physically active in the management of multiple sclerosis (MS).3 These benefits extend beyond enhancing general health and well-being to include potential disease-modifying effects, supported by magnetic resonance imaging outcomes and research in MS animal models.4 Physical activity (PA) is considered the most important nonpharmaceutical intervention in the management of MS.5 Increasing one’s PA levels as part of everyday life, or through engagement in structured exercise, should be an essential component of a comprehensive management plan for persons living with MS.6 Current data indicate that persons with MS are far less active than age-matched healthy populations.7 Health care providers (HCPs) working with individuals with MS play an important role in the management of this chronic progressive and currently incurable disease. Studies focused on PA have shown that people with MS 1) have received mixed messages from HCPs about being active,8 2) do not feel that HCPs regularly promote engagement in PA,9 and 3) want advice from their HCP to optimize their PA behavior.10
Although important, educating clients about the importance of being physically active alone is not sufficient to change PA behavior in the face of a progressive neurodegenerative disease.11 A current theme in the literature is that initiatives to increase engagement in PA with neurologic populations should also include behavior change strategies,12 which are the active components of a behavior change intervention.13 A behavior change intervention is a coordinated set of strategies designed to target a specific behavioral pattern, such as PA.13 Behavior change strategies are ways to ensure optimal effectiveness of healthy lifestyle promotion and include components such as self-efficacy assessment, barrier identification, and problem solving, which combined can enhance intervention implementation.12 The inconsistent use of PA behavioral interventions by HCPs in routine care is an important contributor to the low levels of PA observed among people with MS.9
Having explored HCP needs in an American context, Learmonth et al14 propose that the lack of PA behavioral consultation might be explained by the unmet needs of HCPs. There is a need to modify and align preexisting conceptual frameworks15 for exercise promotion with people with MS across health care jurisdictions. In the Canadian health care system, viewpoints of HCPs currently working with persons with MS have not been elucidated and fully explored. Gathering input from HCPs themselves will highlight barriers that may be preventing the translation of PA behavior change research with people with MS into practice. This study aimed to investigate the current practices and perspectives of HCPs in their application of PA behavior interventions when working with persons with MS in a Canadian context. Intervention design based on current HCP needs and perspectives will positively affect the lives of people with MS. Findings from this study will be meaningful to all end users, including HCPs and persons with MS, in Canada and globally.
Methods
Research Team
The research team consisted of four physiotherapist (PT) researchers trained in Canada (S.O., K.E.M.) and Australia (S.J.D., S.M.). We acknowledge that our ways of knowing are grounded in a Eurocentric, biopsychosocial paradigm, which is integrated throughout all aspects of this research project. As a team of physiotherapy researchers, we wanted to bring the perspectives of persons with MS as one way of ensuring that this research project is relevant and meaningful not only to researchers and clinicians but also to people with MS who will be affected by this work. Therefore, we have explicitly enhanced the role of people with MS in the design, data collection, and analysis of this research by including two individuals with MS in a research advisory committee guiding this project. This research advisory committee also consisted of nonphysiotherapy researchers, including a behavior change specialist and a front-line MS physician, providing further breadth and diverse perspectives into all aspects of this research project.
Design
Interpretative description, an applied qualitative research approach, was the method used in this study.16 A key feature of interpretative description is the integration of knowledge development in relation to clinical experiences such that new insights informing clinical practice can be obtained.16 Our researchers and advisory committee brought diverse perspectives, lived experiences, and knowledge to inform this project. Interpretative description acknowledges that the professional and personal experiences of researchers inform the interpretation and presentation of results in the current care context.16
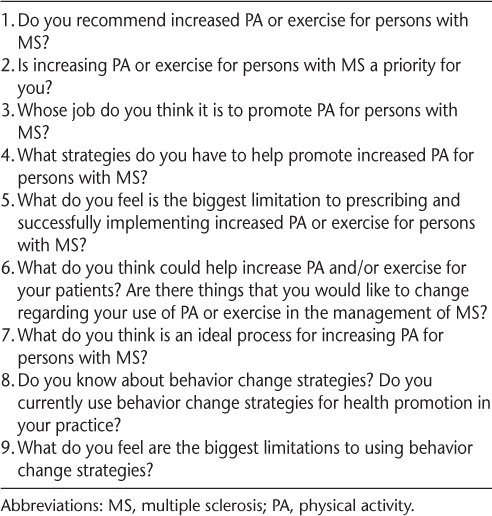
Focus groups were used for data collection to encourage rich interaction between participants.17 Interaction can facilitate sharing ideas, explaining participant lived realities, identifying problems or barriers, sparking discussions, and highlighting potential solutions to identified barriers. A semistructured interview guide (Table 1) was developed by us and was reviewed and refined based on the input of an advisory committee. This study was approved on ethical grounds by the research ethics boards of the University of Saskatchewan, Regina Qu’Appelle Health Region and Prince Albert Parkland Health Region.
Sample question guide from semistructured focus groups
Participants and Recruitment
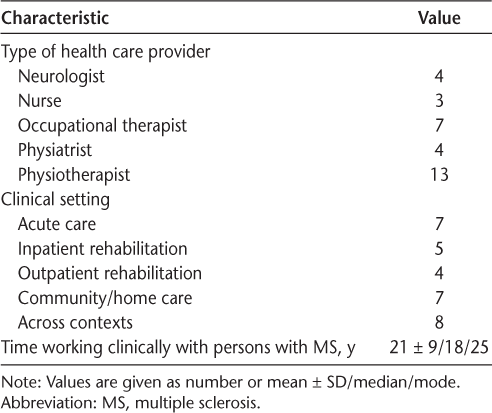
Participants were HCPs working in the publicly funded Canadian health care context and were recruited using purposive convenience sampling. Recruitment flyers were posted in the main health regions across Saskatchewan to recruit from a variety of HCPs across clinical settings (eg, acute care, inpatient rehabilitation, outpatient rehabilitation, and community/home care). Interested participants contacted a researcher (S.J.D.). For study inclusion, participants had to be an HCP and have worked with persons with MS in Saskatchewan for a minimum of 1 year. For participant demographic characteristics, see Table 2.
Demographic characteristics of the 31 study participants
Data Collection and Analysis
Data collection and analysis were inductive and iterative. Consistent with an interpretative approach, researchers kept field notes and journaled on impressions after each meeting. Minor modifications to the semistructured interview guide were made accordingly throughout the data collection process.
Two of the researchers (S.J.D. and K.E.M.) conducted semistructured focus groups at each participating location. Focus group meetings lasted 43 to 68 minutes, with group size ranging from three to eight participants. One week after each focus group, participants were invited to share any further reflective responses. Participants were also invited to review the original transcript from their focus group and provide any additional reflections or insights.18
After clarifying member reflections, transcripts were independently analyzed by three researchers (S.J.D., S.O., and K.E.M.) using whole data immersion. Preliminary codes were then discussed as a group. Using the preliminary code, three researchers (S.J.D., S.O., K.E.M.) independently reviewed the transcripts again before further group discussion designed to share and resolve any discrepancies. Transcripts were then imported into NVivo 11 (QSR International Pty Ltd, Melbourne, Australia) for formal coding and analysis. Transcripts were reread numerous times to review interpretations, and similarly coded segments were compared to ensure consistently applied coding.19 Through comparative and iterative analyses, codes were added and adjusted as needed. The researchers (S.J.D., S.O., K.E.M.) discussed and labeled five resulting themes informed by their clinical research perspectives.
Triangulation was used both in data generation (member reflections of focus group transcripts) and in the data analysis process (three researchers independently coding). Notes about research and decision-making processes were kept to ensure a thorough analytical process20 in which the quality and nature of findings were congruent with the research process.
Results
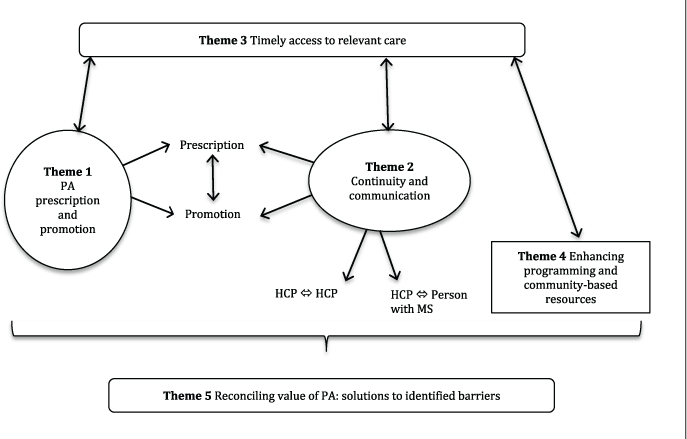
Five interconnecting themes were identified and labeled (Figure 1). These themes depict the experiential reality of HCPs working with people with MS in Saskatchewan regarding interventions addressing PA behavior.
Results: Five interconnecting themes
Prescribing, Promoting, and Impacting Wellness with PA
The HCPs noted that there was a difference between promotion and prescription of PA. They acknowledge that saying one should be exercising (promotion) and implementing a program to actually meet this advice (prescription) are two very different things. Neurologist 1: “I think it’s hard to get people to do it. It’s hard to monitor. It’s important for them, but not my priority. Right now I guess we can just continually tell people it’s a good idea. I can’t actually tell them what to do. We need everyone to promote, but someone specific to prescribe, monitor, and problem solve.” Certain HCPs (PTs and exercise specialists) were suggested by most participants as being the ideal professionals to fill the prescriber role. The PTs affirmed this statement but also admitted that there are numerous barriers to being able to successfully implement a PA behavior change intervention for persons with MS (elaborated on in more detail in later themes). Participants felt that implementation success is enhanced when all members of the health care team promote PA (see dialogue later herein). The consensus was that everyone needs to promote the message, but in particular neurologists and family doctors, and that promoters need to take a more active role in referring onward to prescribers. Neurologists and family doctors were seen as influential promoters and the HCPs that persons with MS most regularly see. PT3: “We all have to be on the same team. It’s everyone on the team’s job to promote physical activity if we want it to work.” Occupational therapist 1: “Yeah, the whole team, really.” PT4: “Yeah it can’t be just us, because if every-one’s not being consistent and saying the same things, it’ll be too hard to do it all on our own.” Occupational therapist 1: “Well if you get one person on that team, particularly a physician, not promoting that, they’re the ones that tend to be listened to.”
It was recommended that promoters should be more aware of existing resources or community experts (if any) in MS PA prescription and use them as part of their promotion. Prescription should be individualized, expert informed, monitored, and supported over time. As one physiatrist noted, “physicians need to recommend it. But I don’t think that physicians need to prescribe. They don’t have the expertise, or the time, or the resources even. We need prescribers.” Monitoring and providing ongoing support were recognized as particularly challenging by the different HCPs. PT12: “I don’t know how much my patients are actually doing it. I don’t monitor it—I don’t have time.”
Participants felt that prescribers need to increase their use of behavior change strategies to facilitate an individualized process that is meaningful to people with MS. In one neurologist’s experience, “it’s really easy to get someone excited about it, but it’s very different when they wake up in the morning and they’re tired as hell and they actually need to motivate themselves. I don’t know how to.” Overall, the priority of PA as a component of wellness in the management of MS was there in theory, and it seems as though the role of PA in the management of MS is valued, but addressing PA behavior is not a consistent part of routine practice. As summed up by PT9, “we need everyone to promote, but someone specific to prescribe, monitor, and problem solve.” This quotation highlights the importance of including behavior change strategies with PA interventions.
Coordinating Communication and Continuity in Practice
All the participants valued the role of PA in the management of MS; however, several noted that there were times when inconsistent messaging was being delivered from diverse HCP team members to people with MS. Mixed messaging regarding PA creates confusion and barriers to implementation success. Physiatrist 3: “The family doctor had said, ‘stop exercising.’ The way they told it to me. They were told to stop exercising completely, and ahhh that can’t be right or that’s incredibly outdated thinking. But it still happens.” The need for consistent messaging, training, and updating among practicing clinicians as well as improved communication between HCPs and persons with MS was viewed as essential. Physiatrist 1: “We need to dismiss fears around exercising and the fact that it’s not causing harm. We need expert informed and more consistent access, otherwise it won’t be sustainable.”
There was a strong need to improve communication between HCPs across health care contexts. PT4: “There seems to be a lack of communication between neurologists and the physiatrist. I don’t understand the history behind that.” Participants expressed concern as to how to make sure messages, knowledge of options, and client experience are more consistent. They expressed concern with the absence of a consistent pathway for persons with MS and felt that a lack of continuity means people with MS are often left to be their own self-advocates (and/or look to other less-trained individuals who may not fully understand the intricacies of MS to safely support or prescribe exercise to people with MS). Several participants were unaware of existing resources such as MS nurses, new diagnosis packages through the MS Society, existing guidelines for PA in mild-to-moderate MS, or even the most recent evidence for PA effectiveness in the management of MS. Physiatrist 1: “You have to know what’s available.” Neurologist 1: “I definitely don’t.” Physiatrist 2: “I think historically there have been better community connections. I don’t always feel like I’m up to speed. It would be great if we could know about what’s going on in the community or had a way of staying on top of it.”
When considering communication, participants described the need for a way to stay up to date with the scientific evidence and best practice guidelines. Across all disciplines there was a lack of awareness of what resources do exist paired with the belief that there was also a lack of resources (elaborated on in theme 4).
Timely Access to Relevant Care: Being Proactive Rather than Reactive
The view that current practice lacks emphasis on promoting, prescribing, and monitoring PA behavior was consistent across disciplines and health care contexts and was attributed to a lack of time, access, and resources. As one nurse said, “there are just a lack of resources in the community and health region, and barriers. Real barriers and we need someone to help them [people with MS] problem solve.” Regarding time, HCPs expressed concerns with the infrequency of visits to the MS speciality clinic (eg, only annually or biannually), long waitlists (for rehabilitation services), lack of follow-up, and the short length of time they are able to spend with persons with MS. Concerning which HCP could best prescribe exercise for people with MS, physiatrist 1 thought that “physiotherapy is ideal, but … our system is stretched from the physio perspective, and there are other things that physios need to do.” This suggests that there are barriers at the health system level.
Many HCPs expressed that their interactions with persons with MS were based around triaging problems and treating in a reactive manner, for example, prescribing a new wheelchair or assistive device, or addressing a recent onset of foot drop: PT11: “Our system is too reactive. Someone has foot drop and now we will put on a brace. I’m not saying that’s not important, it absolutely is with the progressive nature of MS. They usually have a waitlist for that appointment too and as their assistive needs change they become less active while they wait. But then, I think there is such a need to have a proactive element. Time to get them more active and more rehab before they start to progress.” This quotation is one of many representing the HCPs’ concerns with timely access to relevant care.
Regarding access, participants reported a lack of specialists for MS and lack of opportunity to have advanced practice in MS care. Nurse 1: “It would be really nice to be able to refer to a specific MS expert, resource, or exercise program.” At the time of the study, little was known about the provincial geographic distribution of people with MS, but participants reported limitations in MS specialty care even in urban settings. Rural services are needed. A limited number of MS nurses and no rehabilitation services dedicated to patients with MS throughout the province were also reported resource concerns.
PT2 said, “If I have time I’ll promote exercise, but I don’t monitor adherence because I don’t have time or there’s no time for follow-up.” Long waitlists and access and resource issues contribute to the reactive nature of the health care system. A change in services should consider the needs of persons with MS so that the system is relevant to both the person with MS and the HCP.
Enhancing Programming and Community-Based Resources
The HCPs pointed out that compared with the other neurologic or chronic disease populations they work with, MS is underserved. PT1: “Well what we’re forced to do is try and take our MS population and plug it into community-based programs that don’t exist. We have such limited services right now.”
Along the lines of the lack of resources and access described in theme 3, the underserved component was highlighted by multiple HCPs expressing concern that they have nothing to refer their clients to. Many participants were unaware of what, if any, community resources exist. As stated by PT6, “… there’s the MS clinic … above and beyond that, I don’t think we know what other resources there are.” And PT4: “after their acute stay, they fall off the radar and there’s very poor follow-up generally.”
The HCPs desire a provincial MS-specific pathway that considers community resources and/or more accessible outpatient services for people with MS. PT1: “Why can’t we have a seamless pathway to move through from diagnosis to support in the community, which would require more support in the community?” A model that builds and/or borrows from other chronic diseases, such as the “live well” program (for arthritis, diabetes, cardiac, stroke), was suggested. Nurse 3: “Why can’t we just have an MS-specific program there with flexible hours that people can attend with expert input? We have nothing compared to cardiac rehab.” Physiatrist 4: “We should have and need more resources like other chronic diseases.”
Reconciling Value of PA with Clinical Practice: Solutions to Identified Barriers
There was a clear message that HCPs value PA, yet it is not being prioritized in practice, for seemingly diverse reasons. Physiatrist 3: “I think we can do better at educating and providing hope. I don’t think people think about exercise as being healthy for the brain. We can do better at counseling to find what they like and monitoring it. Just putting more effort in, rather than just saying exercise.”
Similarly, participants knew what behavior change strategies were but were not able to give tangible examples of their use in clinical practice. Education and goal setting were the examples given by HCPs of types of behavior change strategies given. PT3: “I guess it would help if I could implement behavior change strategies with their physical activity, but what does that mean— what would it look like?” There was desire to learn more about how to implement behavior change strategies for healthy lifestyle behaviors, including PA. Skepticism was noted about the ability to change practice, even with increased knowledge of behavior change strategies, in the current system. Perhaps there should be a priority to change the current health service delivery for people with MS based on comments suggesting that Saskatchewan, having one of the highest rates of MS worldwide, should have state-of-the-art MS care.
Potential solutions were offered to improve the use of behavior change strategies and successful implementation of PA for persons with MS. These included an MS-specific clinical pathway; a website or some sort of updated system to communicate the availability of resources and how to access them; more MS nurses and MS-specific rehabilitation specialists; a method to support better integration of existing evidence and resources, such as the local branch of the MS Society; and creating more resources both in terms of PA community classes but also educational and referral material for PA promoters. Physiatrist 2: “Ideally we would have to have a way that we could influence them to carry on activity. More follow-up, more expertise, more options, coaching. There’s no one answer.” PT2: “We need a re-shift in focus on behalf of the health region, ministry, everybody—they could reduce the burden so much by focusing on prevention more in acute care and early diagnosis.”
Discussion
This study provides insight from a Canadian health care context and confirms that PA behavior is currently not being addressed in the routine management of MS. The findings of this study suggest that HCPs are aware of the importance of addressing PA behavior but are not able to prioritize and successfully implement PA changes with persons with MS in the current health care system. Consistent with previous literature, it is not the approach of our health care system to focus on proactive lifestyle and wellness interventions.21 This is perhaps a component driving the complexity of why PA prescription is not prioritized, even among HCPs who believe in it and some who are well versed in it. Successful implementation of PA interventions includes using behavior change strategies to facilitate the process of prescription.6,10 The proposed solutions from this study support the need for consistent messaging and promotion across disciplines with opportunities for follow-up to monitor adherence and allow ongoing expert support.22 With the progressive and variable nature of MS, this ongoing support enables the access to care needed to adapt programs in an individualized client-oriented manner. Operating in an acute care paradigm with competing priorities and limitations in access and treatment time, HCP interventions are often focused on reactive impairment–specific issues (eg, prescribing walking aids and assistive devices, dealing with pressure sores) as opposed to prevention.
The perspective that the health care system is reactive in nature is not unique to MS care23 but seems to be a driving factor in HCP delivery of MS care in Saskatchewan. With advancements in disease and symptom management options, the critical question is how do we streamline the delivery of MS care within health facilities and within communities to meet the broad and diverse needs of persons with MS. A general shift of focus to prevention and better lifestyle management for this chronic disease is needed because there seems to be great value in this type of care for persons with MS.24 Who owns this responsibility is an important question. Extrinsic barriers do exist that need to be addressed with health care system change, but training at the individual level is an important component of supporting HCPs in taking ownership over addressing PA behavior change.25
Consistently voiced was the lack of resources to successfully address PA behavior. The HCPs feel that their time is prioritized to “put out fires,” yet most agree that increasing PA levels for people with MS would target and enhance many treatment priorities (eg, fatigue, balance, and function). Overall there is a reported lack of the time, follow-up, and/or resources to prescribe/monitor PA in a way that is meaningful to persons with MS. Financial barriers were apparent, with repeated reference to long waitlists, lack of follow-up, understaffing, and a small number of HCPs with expertise in MS care, all of which are costly resources. Budget cuts are now a reality of the health care system; however, the present study’s findings also mentioned a lack of several low-cost resources as a barrier to promoting PA management options. Lack of localized informational material on PA resources for people with MS, client-specific material for PA, and a list of who and/or what HCPs can refer to to meet individualized PA goals were among those mentioned. Most HCPs expressed the desire to learn more about behavior change strategies—perhaps unique for neurodegenerative diseases.
Although systemic and resource barriers exist, there are other chronic disease models (such as cardiovascular disease and arthritis) that can provide potential models to inform community programs for people with MS.26 Community-based alternatives could be used to decrease the cost of care,27 but there also need to be community resources that exist and can be customized to the local needs of people with MS. From the HCP perspective in this study, an ideal community resource should be structured, be expertise informed, have a social and support element, be ongoing, be accessible, and involve elements of behavior change to encourage out-of-session/program maintenance.
The present findings are applicable in a Canadian context but may also be relevant to further refining frameworks15 outside of Canada. A recently revised conceptual model of exercise promotion through the patient-provider interaction in MS suggests three hierarchical yet interactive layers: provider preparation, patient-provider interaction, and patient behavior change.22 Interestingly, the present findings reveal similarities with this model, providing further evidence that improving communication and consistency of messaging across HCPs and health care contexts is a low-cost, and potentially cost-saving, solution that should be a priority to enhance the overall management of MS, including PA interventions. However, HCPs in the present study also expressed that it is everyone’s job to promote exercise, and the PT’s and/or exercise specialist’s role to prescribe. The effectiveness of such a model would require all HCPs to become active promoters and to know of and refer to prescribers, further emphasizing the importance of communication and consistent messaging.
Successful implementation of a conceptual model for exercise promotion requires more resources, time, and expertise and the establishment of a long-term structured program provided in the community. There also needs to be a way for HCPs to keep up to date with this information. In a Canadian context there is currently no system in place to train incoming HCPs, a reported lack of opportunity to have advanced practice in MS, and also no provincially shared pathway for MS clinical care. This expands beyond the scope of PA, but the reality is that MS care overall needs to be improved to enhance management and lifestyle interventions, including PA.
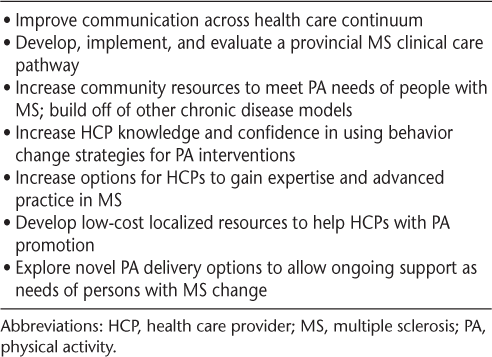
Key suggestions to enhance MS care and address PA behavior in the management of MS based on the findings in this study are summarized in Table 3. There is a need for more resources, but what good are those resources if no method of communicating their availability exists and if access to HCPs is limited? Health care providers need to be active promoters of PA, but there needs to be a system in place to increase HCP awareness of resources in addition to ensuring that resources are meeting the needs of persons with MS prioritizing a client-centered approach to chronic disease management. However, to support immediate individual-level change we encourage HCPs working with people with MS to look for ways to incorporate PA behavioral interventions into their current practice, look for other HCPs to create a referral network between promoters and prescribers, and become familiar with any existing community resources to support exercise behavior for people with MS.
Key suggestions, based on findings, to enhance MS care and address PA behavior in MS management
Limitations and Future Research
This study included a variety of HCPs from across the province but did not have general medical practitioners. Future research investigating communication and pathways among HCPs should involve general medical practitioners because they are seen as influential in PA promotion (theme 1). The HCPs prioritize PA in theory, but there is a gap in perspective and practice. Physical activity and behavior change should be one and the same, but theory and practice are often different. There is a need for future studies to explore these concepts in more depth. Future research should also consider interventions targeting HCPs but not without consideration of implementation, such as a participatory health research process or an integrated knowledge translation method to enhance communication. As solutions are identified, they can also be incorporated into care pathways and health system priorities, addressing both individual- and system-level change.
This qualitative account of HCPs’ current perspectives and practice has shown that HCPs value PA and want more information on behavior change strategies and their use to be more effective in changing PA behavior for persons with MS. Unfortunately, due to the acute and reactive nature of the health care system, HCPs feel that they cannot prioritize this in practice. Both system- and individual-level change are needed to support consistent and effective use of PA behavior interventions in the ongoing management of MS.
PRACTICE POINTS
Addressing physical activity (PA) behavior in a manner that is meaningful, relevant, and appropriate for persons with MS is not a routine part of MS care; reasons are complex, and changes are needed at both the individual health care provider (HCP) level and the health care system level.
Increasing HCPs’ knowledge, confidence, and skills in using behavior change strategies for PA interventions and increasing opportunities to gain expertise and advanced practice in MS would affect individual-level change.
Novel delivery options to allow ongoing support from HCPs as the needs of persons with MS change and enhanced community design may mitigate access issues as a component of system-level change.
New resources to facilitate PA promotion and prescription should be created in partnership with diverse HCPs and across health care contexts.
Financial Disclosures
The authors declare no conflicts of interest.
References
Motl RW, Sandroff BM. Benefits of exercise training in multiple sclerosis. Curr Neurol Neurosic Rep. 2015; 15: 62.
Pilutti LA, Platta ME, Motl RW, et al. The safety of exercise training in multiple sclerosis: a systematic review. J Neurol Sci. 2014; 343: 3– 7.
Baird JF, Sandroff BM, Motl RW. Therapies for mobility disability in persons with multiple sclerosis. Expert Rev Neurother. 2018; 18: 493– 502.
Motl RW, Sandroff BM. Exercise as a countermeasure to declining central nervous system function in multiple sclerosis. Clin Ther. 2018; 40: 16– 25.
Vollmer TL, Benedict R, Bennett S, et al. Exercise as prescriptive therapy in multiple sclerosis: a consensus conference white paper. Int J MS Care . 2012; 14: 2– 16.
Durstine JL, Gordon B, Wang Z, et al. Chronic disease and the link to physical activity. J Sport Health Sci. 2013; 2: 3– 11.
Kinnett-Hopkins D, Adamson B, Rougeau K, et al. People with MS are less physically active than healthy controls but as active as those with other chronic diseases: an updated meta-analysis. Mult Scler Relat Disord . 2017; 13: 38– 43.
Learmonth YC, Motl RW. Physical activity and exercise training in multiple sclerosis: a review and content analysis of qualitative research identifying perceived determinants and consequences. Disabil Rehabil. 2016; 38: 1227– 1242.
Richardson E, Barstow EA, Motl RA. A narrative exploration of the evolving perception of exercise among persons with multiple sclerosis. Qual Res Sport Exerc Health . 2018; 11: 119– 137.
Learmonth YC, Adamson BC, Balto JM, et al. Multiple sclerosis patients need and want information on exercise promotion from healthcare providers: a qualitative study. Health Expect. 2017; 20: 574– 583.
Motl RW, Pekmezi D, Wingo BC. Promotion of physical activity and exercise in multiple sclerosis: importance of behavioral science and theory. Mult Scler J Exp Transl Clin. 2018; 4: 2055217318786745.
Casey B, Coote S, Hayes S, et al. Changing physical activity behavior in people with multiple sclerosis: a systematic review and meta-analysis. Arch Phys Med Rehabil . 2018; 99: 2059– 2075.
Michie S, Johnston M. Theories and techniques of behavior change: developing a cumulative science of behavior change. Health Psychol Rev . 2012; 6: 1– 6.
Learmonth YC, Adamson BC, Balto JM, et al. Investigating the needs and wants of healthcare providers for promoting exercise in persons with multiple sclerosis: a qualitative study. Disabil Rehabil. 2018; 40: 2172– 2180.
Motl RW, Barstow EA, Blaylock S, et al. Promotion of exercise in multiple sclerosis through healthcare providers. Exerc Sport Sci Rev. 2018; 46: 105– 111.
Thorne S. Interpretive Description: Qualitative Research for Applied Practice . 2nd ed. Routledge; 2016.
Rigg KK, Cook HH, Murphy JW. Expanding the scope and relevance of health interventions: moving beyond clinical trials and behavior change models. Int J Qual Stud Health Well-being . 2014; 9: 24743.
Smith B, McGannon KR. Developing rigor in qualitative research: Problems and opportunities within sport and exercise psychology. Int Rev Sport Exerc Psychol . 2018; 11: 101– 121.
Hewitt-Taylor J. Use of constant comparative analysis in qualitative research. Nurs Stand . 2001; 15: 39– 42.
Tracy S. Qualitative quality: eight “big-tent” criteria for excellent qualitative research. Qual Inq . 2010; 16: 837– 851.
Kadu MK, Stolee P. Facilitators and barriers of implementing the chronic care model in primary care: a systematic review. BMC Fam Pract . 2015; 16: 12.
Richardson EV, Barstow E, Fifolt M, Motl RW. Evaluation of a conceptual model regarding exercise promotion through the patient-provider interaction in multiple sclerosis: health care provider perspectives [published online ahead of print December 25, 2018]. Qual Health Res . doi: 10.1177/1049732318819453.
Turner S, Goulding L, Denis JL, et al. Major system change: a management and organisational research perspective. In: Raine R, Fitzpatrick R, Barratt H, et al. Challenges, Solutions and Future Directions in the Evaluation of Service Innovations in Health Care and Public Health. Southampton, UK: NIHR Journals Library; May 2016. Health Services and Delivery Research, No. 4.16, Essay 6.
Null G, Pennesi L, Feldman M. Nutrition and lifestyle intervention on mood and neurological disorders. J Evid Based Complementary Altern Med . 2017; 22: 68– 74.
Institute of Medicine (US) Roundtable on Evidence-Based Medicine; Yong PL, Saunders RS, Olsen LA, eds. Missed prevention opportunities. In: The Healthcare Imperative: Lowering Costs and Improving Outcomes: Workshop Series Summary. National Academies Press (US); 2010. https://www.ncbi.nlm.nih.gov/books/NBK53914/.
Pio CSA, Chaves G, Davies P, Taylor R, Grace S. Interventions to promote patient utilization of cardiac rehabilitation: Cochrane systematic review and meta-analysis. J Clin Med . 2019; 8: 189.
OHTAC OCDM Collaborative. Optimizing chronic disease management in the community (outpatient) setting (OCDM): an evidentiary framework. Ont Health Technol Assess Ser . 2013; 13: 1– 78.







