Publication
Research Article
International Journal of MS Care
Accessibility to Telerehabilitation Services for People With Multiple Sclerosis: Analysis of Barriers and Limitations
Author(s):
ABSTRACT
BACKGROUND
In multiple sclerosis (MS), telemedicine improves access to specialized medical care; however, barriers remain, including universal access and effective implementation. Focusing on telerehabilitation, ie, remotely delivered physical therapy, our goal was to identify barriers to telerehabilitation implementation and factors associated with patients completing telerehabilitation physical therapy treatment.
METHODS
Quantitative data included a review of electronic health records of patients with MS treated at the University of California San Francisco Physical Therapy Faculty Practice. We extracted demographic, clinical, and transit-related factors. For patients who scheduled an initial evaluation, we recorded the number of follow-ups, cancellations, completed physical therapy goals, and discharges. Qualitative data included interviews with 3 board-certified neurologic physical therapists and patients’ perspectives recorded in the subjective portion of physical therapy notes.
RESULTS
We identified 111 patients with at least 1 visit (in-person or telerehabilitation) to physical therapy (82 women; mean ± SD age, 54.2 ± 12.7 years). Patients with no disability (Expanded Disability Status Scale [EDSS] score, 0) were 73% less likely to schedule a follow-up appointment (in-person or telerehabilitation) than those with some disability (EDSS score, >0) (odds ratio, 0.27; 95% CI, 0.09–0.75; P = .012). Neurologic physical therapists identified reduced travel burden and scheduling flexibility as benefits of telerehabilitation vs in-person visits. Barriers to telerehabilitation included low technological literacy, cognitive impairment, and fall risk. Patients described scheduling conflicts and pain/illness as barriers to telerehabilitation.
CONCLUSIONS
Patients with no disability were least likely to complete physical therapy treatment via telerehabilitation. Although both benefits and barriers to completing physical therapy via telerehabilitation are present, the neurologic physical therapists were supportive of a hybrid model for physical therapy.
Neurologic physical therapy can address symptomatic concerns and improve overall quality of life for people with multiple sclerosis (MS).1 Despite these benefits, at least 36% of people with MS in the United States are not able to access necessary physical therapy evaluation and treatment.2 Among the many barriers in accessing specialized care (eg, driving distance to specialty clinics, numerous appointments, inadequate health insurance), the marked variability in MS-related functional impairments (eg, balance, gait, vision, fatigue) can make it even more challenging to attend traditional in-person medical visits.3,4
With high-speed internet and videoconferencing readily available, remotely delivered care via telerehabilitation has shown promise in bridging the gap between physical therapists and people with MS who have limited access to specialty care.5 Telerehabilitation is defined as the use of technology to provide access to rehabilitative care when distance separates patients and clinicians.6 Although telerehabilitation services were available before the SARS-CoV-2 pandemic, since March 2020, health care practitioners and patients have had to adapt to new models of care, and the adoption of telerehabilitation has greatly increased.7 Physical therapists have used videoconferencing, virtual communication software, and telephone visits to provide quality care while maintaining social distancing.7,8
Several studies have pointed to the advantages of telemedicine-based care for people with MS more broadly, including the potential to permanently alter the known health care model.6,9 For example, telemedicine can decrease the time before people with MS can access specialized heath care services (eg, neurologic rehabilitation experts) compared with standard in-person care.10,11 Televideo-enabled neurologic care for patients with MS decreases travel time,12,13 limits time off work,12,14 reduces caregiver burden,4,12 and improves access to care in rural areas.4,9,12 Telerehabilitation, more specifically, could allow for clinicians to more conveniently monitor patient progress14,15 and for better communication between physical therapists and people with MS.
However, although offering possible benefits in terms of improved access, telerehabilitation also faces a variety of obstacles that must be called out and addressed to support its expanded and sustained adoption. In fact, a systematic review of obstacles to adoption of telemedicine worldwide identified limitations in the technological literacy of staff, resistance to change, and cost of technology.16 Infrastructure barriers (eg, limited internet connection, lack of access to technology) also represent systemic barriers.17 Despite expanded use of technologies to deliver telerehabilitation, limited work has been conducted to consider its feasibility, acceptance, and usability among users (both people with MS and physical therapists).18
This study of a physical therapy practice has 2 aims: (1) to identify barriers to implementing telerehabilitation and in-person visits from the perspectives of people with MS and MS physical therapists and (2) to identify the demographic and clinical predictors for people with MS who successfully complete neurologic physical therapy treatment either in-person or via telerehabilitation.
METHODS
With the approval of the University of California San Francisco (UCSF) institutional review board, we conducted an ambidirectional study19 with both retrospective and prospective elements. Electronic health record (EHR) data were collected from patients treated at the UCSF Physical Therapy Faculty Practice (PTFP), Mount Zion and Mission Bay centers, between April 1, 2020, and May 1, 2021. Patients were treated via telerehabilitation (using the UCSF information technology department–approved Zoom platform), in-person care, or a combination of in-person and telerehabilitation care. Physical therapists’ schedules included a mix of in-person and telerehabilitation visits each day. Of note, under expanded benefits from the Centers for Medicare & Medicaid Services, telerehabilitation is reimbursed at the same rate as in-person visits.20–22 Patients were adults with a neuroimmunology diagnosis: MS, neuromyelits optica spectrum disorder, or clinically isolated syndrome.
Predictive Variables
The following variables were extracted from the EHR: demographic variables (age, sex, employment status); clinical variables (Expanded Disability Status Scale [EDSS] score,23 disease-modifying therapies, comorbidities using the Charlson Comorbidity Index [CCI]); physical therapy-related variables (presenting symptom, symptom duration); and transit-related data (driving distance and time from home zip code, home zip code bike and transit score [calculated via Walk Score Research24] to reflect the quality of the cycling and public transit infrastructure).
Visit Characteristics
Adoption of telerehabilitation was calculated by the number of physical therapy referrals issued during routine care at the UCSF Center for MS and Neuroinflammation and, subsequently, the number of initial physical therapy appointments scheduled from these referrals. We recorded the number of follow-up physical therapy appointments (visits after initial evaluation) scheduled and attended, as well as no-show visits.
Completion of physical therapy treatment was defined as the number of patients who met the physical therapy goals set at their initial appointment and were formally discharged from care (as opposed to not returning to physical therapy). We aimed to identify factors (demographic, disease-related, physical therapy treatment, transit-related) predictive of completing physical therapy treatment.
Qualitative Analysis of Barriers and Facilitators to Telerehabilitation Implementation
EHR Review
From the EHR review, we recorded patients’ reported barriers to attending appointments and completing physical therapy treatment from the subjective portion of the physical therapy notes as well as from patient messages to their physical therapist, when available.
Semistructured Interviews
Two of us (A.G. [DPT, PhDc; female; graduate student] and V.B. [MS physical therapy; female; research assistant]) conducted semistructured interviews with 3 of the 5 board-certified neurologic physical therapists who treated people with MS at the UCSF PTFP during the defined study period. These physical therapists were selected via convenience sampling (available for interview and experience treating people with neurological disorders) and were interviewed via Zoom. All 3 therapists provided informed consent to participate in this study. Before the interviews, the authors and physical therapists had working professional relationships, and the therapists were familiar with this study team’s long-term research interests. The semistructured interviews included general professional perspectives on telerehabilitation and the perceived barriers to patients and physical therapists. There were 5 key subject areas: (1) overall experience with the shift from in-person visits to telerehabilitation after SARS-CoV-2 shelter-in-place guidance, (2) barriers to using telerehabilitation technology, (3) characteristics of patients that could support completion of physical therapy treatment, (4) perceived benefits of telerehabilitation compared with in-person rehabilitation, and (5) the anticipated future of telerehabilitation. Interviews were recorded and transcribed using Zoom software. Two of us (A.G. and V.B.) made notes during and after the interviews; they independently developed code lists for salient themes after 1 interview and then discussed and agreed on a consolidated list. This code was then applied to the remaining interviews. These data were then reviewed with the senior author (R.M.B.). The coded data were grouped into the 5 salient themes and described qualitatively due to the low overall number of observations. The Consolidated Criteria for Reporting Qualitative Research checklist25 was used to minimize bias in the qualitative analysis.
Statistical Analysis
In the quantitative analyses of telerehabilitation adoption and completion of physical therapy treatment in the present patient population, we analyzed possible demographic, disease-related, and transit-related predictors for completing physical therapy treatment using multiple linear regression and the LogWorth statistic to determine the contribution of each variable to the outcomes of interest.26 Odds ratios were used to identify relative odds of completing physical therapy treatment with respect to disability status (EDSS score, 0 vs >0) and comorbidity (CCI, 0 vs >0). Statistical analysis of the results and figure generation were conducted using JMP version 15 (SAS Institute Inc).
RESULTS
Description of Patients and Visits
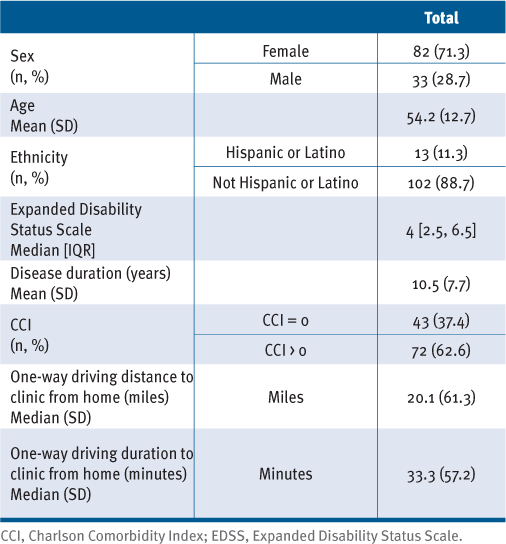
During the selected period (April 1, 2020, to May 1, 2021), 111 patients with demyelinating disease (109 with MS and 1 each with neuromyelits optica spectrum disorder and clinically isolated syndrome) were referred to the UCSF PTFP and scheduled for an initial visit: 82 (74%) were women; mean ± SD age was 54.2 ± 12.7 years, and median EDSS score was 4.0 (interquartile range, 2.5–6.5) (TABLE S1, available in the online version of this article at IJMSC.org). The 3 most common primary symptoms were impaired static/dynamic balance, decreased strength, and impaired gait/mobility. The initial evaluation was in-person (n = 20) or via telerehabilitation (n = 91). After the initial evaluation, 100 patients (90%) scheduled a follow-up appointment. Of the total follow-up appointments scheduled, 31% were canceled, and 60 visits were attended (15 in-person, 45 telerehabilitation). A total of 26 patients (23%) were discharged from physical therapy, of whom 20 (17%) met all their physical therapy goals, completing treatment. Patients who did not meet physical therapy goals (n = 10 [16%]) and did not schedule follow-up appointments were not formally discharged from physical therapy care. Twenty-four patients (20.8%) were still being treated at the time of data collection.
Quantitative Analyses
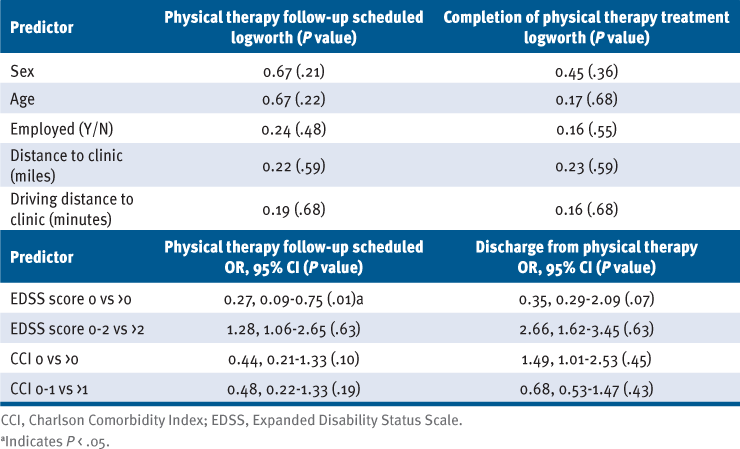
Completion of physical therapy treatment was not found to be associated with demographic, disease-related, or transit-related factors (TABLE 1). However, patients with no disability (EDSS score, 0) were 73% less likely to schedule a follow-up appointment (in-person or telerehabilitation) than those with some disability (EDSS score, >0) (odds ratio, 0.27; 95% CI, 0.09–0.75; P = .012).
Demographics
Qualitative Analyses
EHR Review
Communication between patients and the PTFP was available for 30 of 111 patients (27%). Most patients sent 1 message to the PTFP (n = 14), with 8 patients sending 2 or more messages. Patients cited the following barriers to attending telerehabilitation appointments: conflicts with other medical appointments (n = 11), illness and pain (n = 10), personal conflicts (eg, sick child, work conflict, vacation) (n = 9), preference to see a local physical therapist (n = 4), difficulties with the telerehabilitation platform/technological concerns (n = 4), and preference to wait until vaccinated against COVID-19 to attend an in-person visit (n = 3).
Interviews With Physical Therapists
Interviews with neurologic physical therapists revealed several major themes. For the therapists, the shift from in-person to telerehabilitation during shelter-in-place guidelines occurred with relatively few administrative or financial obstacles. Both patients and physical therapists were flexible because of the emerging public health guidelines, and the transition to telerehabilitation did not result in major lapses in care. One physical therapist noted, “Once patients had their primary care and other appointments over Zoom, it was pretty easy to convince them that virtual physical therapy [was] also really valuable.” Having provided televideo visits using the approved Zoom technology for several years, UCSF was able to rapidly expand this capability to accommodate larger patient volumes. Telerehabilitation could be administered using instruments (eg, computers, tablets, personal smartphones) that are relatively easy to deploy with little burden to either patients or providers.
The 3 physical therapists all reported that the format of the telerehabilitation sessions was the same as the in-person format: sessions consisted of a subjective interview, assessment of range of motion and functional movement, and exercise demonstration and practice.
Two of the physical therapists noted patient barriers to using telerehabilitation technology, and these included poor internet connection, inexperience with video call platforms, limited technological literacy, and the need for an interpreter. One physical therapist mentioned, “Simply being able to access the Zoom platform and position the camera can be a limitation to treating someone.”
Predictors of Physical Therapy Follow-up and Discharge
With respect to the features that supported patients’ ability to receive telerehabilitation care, the therapists cited several patient-, home-, and disease-related factors. First, technological literacy was relevant because substantial time could be wasted troubleshooting rather than engaging in care. “So much time can be wasted figuring out the Wi-Fi network and pointing the camera in the right direction,” a physical therapist mentioned. In addition, a flexible schedule was cited as a positive factor, although this was not clearly relevant to receiving televideo vs in-person care. “It tends to be retired patients and those who work from home who like [telerehabilitation] and attend the most appointments,” a physical therapist noted. The primary home factor noted was enough space to move safely. For patients with more severe physical or cognitive limitations, the presence and support of a caregiver in the home were also noted. Importantly, “The caregiver has to be someone who is comfortable providing support and who is familiar with the patient’s needs. Not all are.”
With respect to functional status, lack of severe balance or mobility impairments that would preclude patients from moving without specialized attention or support (eg, unsafe assistive device use resulting in high fall risk) was noted as a situation in which care could be comparably delivered via telerehabilitation. Of note, a physical therapist mentioned, “Though fall risk might limit the scope of our session, there is still plenty we can do seated and it’s a great time to provide patient education.” The primary symptom for physical therapy referral was also a factor influencing the success of telerehabilitation. For example, physical the therapists felt that vestibular symptoms or facial paralysis are readily treatable via telerehabilitation, partially due to the fact that they require less specialized equipment or tactile input. Conversely, patients with balance and gait impairments, or who are otherwise at risk for falls, can be safety concerns and may not be appropriate for telerehabilitation. “Depending on the level of impairment, I might be able to work on balance from a seated position, but what they really need is to practice standing,” a physical therapist said in reference to modifications for telerehabilitation. These patients may also not experience as much benefit from telerehabilitation compared with in-person access to specialized equipment (eg, a patient who requires use of a ceiling harness for mobility training).
Although not related to telerehabilitation in particular, in contrast to more vague goals (eg, “I want to walk better”), the creation of attainable goals (eg, “I would like to be able to walk my dog for 1 mile”) was identified as a key factor in enhancing patient motivation. This factor was more common in patients who completed their physical therapy goals and were discharged from care because they would be more likely to adhere to a plan of care provided exclusively via telerehabilitation. Explicit and shared goal-setting may be particularly important in nurturing patient motivation from a distance.
Conversely, some factors were identified as representing specific barriers to telerehabilitation visits, leading to at least some, perhaps initial, in-clinic physical therapy treatment. Specifically, the need for human contact and tactile cues was noted for patients with either cognitive impairments or those who spoke languages other than English. For these patients, auditory cues alone via telerehabilitation might be insufficient to provide high-quality physical therapy: “Sometimes I find that verbal cues [aren’t] enough; we need to do tactile demonstration and external feedback and sometimes that is really hard to do over telerehabilitation,” a physical therapist said.
Cognitive impairment was noted as a barrier for 2 reasons. First, it can preclude use of telerehabilitation technology. Second, people with MS with cognitive impairments often have difficulties with concentration or are unable to attend to a task; video conference makes redirection challenging. Therefore, patients without substantial cognitive impairments were identified as more likely to benefit from telerehabilitation. However, a physical therapist mentioned, “If someone who is cognitively impaired has a really awesome caregiver, you can still have a great session. A caregiver who is really engaged and is comfortable making sure the patient is safe can make it possible to treat someone with cognitive impairment over Zoom.”
The perceived benefits of telerehabilitation vs in-person visits included reduced patient travel burden and improved scheduling flexibility. The reduction of travel time was noted by the 3 physical therapists as especially beneficial for patients who are unable to drive or travel independently, as well as for those who have full-time jobs and/or dependents. Telerehabilitation allowed patients to practice exercises in their homes, supervised by physical therapists. It also gave the therapists an understanding of the patients’ general home layouts and circumstances, as well as potential safety concerns present in their environments. One physical therapist endorsed the benefits of examining home environments, stating, “One really nice thing about [telerehabilitation] is getting a glimpse into a patient’s home which you normally wouldn’t get. You can provide suggestions for their bed or stairs set-up to help them reach their goals.” In addition, physical therapists noted that whereas in-person visits are focused on movement quality and analysis, telerehabilitation allows more time for explanation and education, the foundations of successful rehabilitation, particularly for those with neurologic conditions.27
Finally, with respect to the future of telerehabilitation, the physical therapists interviewed indicated that a hybrid in-person/telerehabilitation model would be ideal for care, supporting an in-clinic to in-home continuum of care. One physical therapist said, “I think having [telerehabilitation] as an option is great to provide patient education and [for] patients who need some help tailoring their home program,” and another mentioned, “In between in-person sessions, [telerehabilitation] visits can be helpful so patients don’t have to come in as often.” Telerehabilitation allows for more flexible scheduling, is beneficial for providing education and counseling, and can improve access for those with higher disability and in areas geographically distant to specialized MS physical therapy care; however, some objective measures (eg, Berg Balance Scale) need to be completed in person and are critical for measuring patient progress toward goals, supporting a hybrid model of care. In addition, for patients with cognitive and visual impairments, verbal cues provided via telerehabilitation may be insufficient, and tactile support in-person may be beneficial.
DISCUSSION
This study, leveraging data on the adoption and completion of MS physical therapy treatment via telerehabilitation in the initial response to the COVID-19 pandemic at a large, urban medical center, contributes insights into telerehabilitation barriers and facilitators for people with MS. These include both patient-related factors (eg, disability level, employment) and therapist perspectives on designing safer, more effective, and more accessbile hybrid models for physical therapy care.
Interestingly, only 17% of insured people with MS completed all recommended sessions and met their treatment goals. Although we explored a variety of patient-, disease-, and transit-related factors, only increasing EDSS status was associated with meeting physical therapy goals. For patients with no disability (EDSS score, 0), scheduling and attending any type of physical therapy appointment may have represented less of a priority in the face of other personal and professional obligations, if the value of prophylactic rehabilitation care was not well established or appreciated. Other additional and nonexclusive barriers to treatment completion likely include systemic barriers, such as limited insurance coverage and low insurance reimbursement for physical therapists.
The practicing physical therapists’ preferences were for a hybrid MS rehabilitation model, with the optimal balance of in-person and telerehabilitation-enabled care determined based on a variety of patient-specific factors. The physical therapists suggested that an initial in-person visit may be warranted in persons with cognitive impairments to help provide nonverbal feedback and tactile cues, but other strategies to support home-based delivery may be used. A stepwise set of measures before beginning exercises was suggested to optimize safety during telerehabilitation for patients at greater risk for falls or with cognitive impairment: (1) obtaining an emergency telephone number for someone who can rapidly assist the patient if needed, (2) restricting the patient’s space with physical supports, (3) teaching the patient and/or caregiver fall prevention strategies (eg, using external supports such walls and chairs), and (4) asking the patient and/or caregiver to perform a home safety evaluation (eg, checking for loose rugs, uneven ground). Finally, physical therapists should learn redirection strategies that help people with cognitive impairments to return their attention to the rehabilitation activities.
Other areas that need to be addressed include patient technological literacy (eg, asking patients to attend an educational webinar on the use of the communication platform) and instructional clarity (ie, to support patient comprehension at all cognitive levels, perhaps with the assistance of a caregiver). Some of the barriers identified may also be relevant to reducing the risk and improving the effectiveness of the interventions.
Limitations
The major limitation of this study was the retrospective data collection. In the future, quantitative and qualitative studies should investigate patient-, clinician-, and organization-level implementation barriers, especially for selected (eg, advanced disability) and underrepresented (eg, minority, rural) patient populations. Patient reports were collected from the subjective portion of physical therapy clinical notes, which may not have been exhaustive. Nonetheless, we believe that these pragmatic findings can inform the approach to MS telerehabilitation in other centers.
Although inclusion of qualitative data augments this analysis by providing exploratory insights regarding barriers and facilitators to telerehabilitation, the study design was not rooted in a specific qualitative method; the study would likely have been strengthened by discussion of data saturation, returning transcripts to physical therapists for comment, and obtaining feedback from physical therapists on the findings.
These results support the expanded use of telerehabilitation for MS care. A recent study from our institution suggests that implementation of telerehabilitation to orthopedic populations during shelter-in-place guidelines was feasible, and both patients and physical therapists were highly satisfied.7 Telerehabilitation is a burgeoning and valuable alternative method of delivering physical therapy services to people with MS28; it offers personalized interventions conducted by neurologic physical therapists, adapting the treatments based on the patient’s needs, expediting access to specialized physical therapy care, and saving time and opportunity costs.15,29,30 It is, however, important to acknowledge previous work that identifies the shortcomings of the rapid adoption of technology in other health populations (eg, veterans,31 postoperative care,32 urology33). This work seeks to expand on an existing framework34 to identify limitations, specifically as it relates to the delivery of physical therapy care, to inform future directions of more inclusive telerehabilitation models. Telerehabilitation extends delivery of care to more people with MS at all stages of the disease.6,28 This includes both younger patients with lower disability who are in the workforce, as well as more disabled or more remote patients for whom access is a major issue. The present study extends these observations by highlighting the qualitative factors that could be used as predictive factors in future efficacy trials and to optimize the delivery of MS telerehabilitation care.
CONCLUSIONS
Telerehabilitation can reduce barriers to care access for people with demyelinating disease. Although no demographic or transit-related factors were found to be predictors of completing physical therapy treatment, patients with minimal disability were less likely to complete treatment through a combination of telerehabilitation and in-person visits.
Physical therapists treating people with MS identified reduced travel burden and scheduling flexibility as benefits of telerehabilitation, and low technological literacy, cognitive impairment, and high fall risk as barriers. A hybrid model for physical therapy could include telerehabilitation, which is conducive to providing patient education, whereas in-person visits would enable collection of objective data (eg, reactive balance) and may be preferred for patients with cognitive and visual impairments.
PRACTICE POINT
» A hybrid care model, composed of in-person visits and telerehabilitation visits, could increase accessibility, attendance, and completion of physical therapy treatment for patients with demyelinating disease.
ACKNOWLEDGMENTS:
The authors would like to thank Monika Patel, E.J. Gann, and Alexander Dien for their contribution to this work.
References
Rohrig M. Physical therapy in multiple sclerosis: a resource for healthcare professionals. National MS Society. Accessed October 17, 2021.https://www.nationalmssociety.org/NationalMSSociety/media/MSNationalFiles/Brochures/Clinical_Bulletin_Physical-Therapy-in-MS-Rehabilitation.pdf
Finlayson M, Plow M, Cho C. Use of physical therapy services among middle-aged and older adults with multiple sclerosis. Phys Ther. 2010; 90(11): 1607–1618. doi: 10.2522/ptj.20100072
Pétrin J, Donnelly C, McColl MA, Finlayson M. Is it worth it? the experiences of persons with multiple sclerosis as they access health care to manage their condition. Health Expect. 2020; 23(5): 1269–1279. doi: 10.1111/hex.13109
Bove R, Garcha P, Bevan CJ, Crabtree-Hartman E, Green AJ, Gelfand JM. Clinic to in-home telemedicine reduces barriers to care for patients with MS or other neuroimmunologic conditions. Neurol Neuroimmunol Neuroinflamm. 2018; 5(6): e505. doi: 10.1212/NXI.0000000000000505
Khan F, Amatya B, Kesselring J, Galea M. Telerehabilitation for persons with multiple sclerosis. Cochrane Database Syst Rev. 2015; 2015(4): CD010508. doi: 10.1002/14651858.CD010508.pub2
Yeroushalmi S, Maloni H, Costello K, Wallin MT. Telemedicine and multiple sclerosis: a comprehensive literature review. J Telemed Telecare. 2020; 26(7–8): 400– 413. doi: 10.1177/1357633X19840097
Miller MJ, Pak SS, Keller DR, Barnes DE. Evaluation of pragmatic telehealth physical therapy implementation during the COVID-19 pandemic. Phys Ther. 2021; 101(1): pzaa193. doi: 10.1093/ptj/pzaa193
Hincapié MA, Gallego JC, Gempeler A, Piñeros JA, Nasner D, Escobar MF. Implementation and usefulness of telemedicine during the COVID-19 pandemic: a scoping review. J Prim Care Community Health. 2020; 11: 2150132720980612. doi: 10.1177/2150132720980612
Bove R, Bevan C, Crabtree E, . Toward a low-cost, in-home, telemedicine-enabled assessment of disability in multiple sclerosis. Mult Scler. 2019; 25(11): 1526–1534. doi: 10.1177/1352458518793527
Galea MD. Telemedicine in rehabilitation. Phys Med Rehabil Clin N Am. 2019; 30(2): 473–483. doi: 10.1016/j.pmr.2018.12.002
Swenarton N. During the COVID-19 pandemic, telehealth services were well liked and highly utilized by individuals with multiple sclerosis. Rutgers Today. March 1, 2022. Accessed July 5, 2022.https://www.rutgers.edu/news/people-multiple-sclerosis-benefit-telehealth-services
Hatcher-Martin JM, Busis NA, Cohen BH, . American Academy of Neurology telehealth position statement. Neurology. 2021; 97(7): 334–339. doi: 10.1212/WNL.0000000000012185
Landi D, Ponzano M, Nicoletti CG, . Patient’s point of view on the use of telemedicine in multiple sclerosis: a web-based survey. Neurol Sci. 2022; 43(2): 1197–1205. doi: 10.1007/s10072-021-05398-6
Xiang XM, Bernard J. Telehealth in multiple sclerosis clinical care and research. Curr Neurol Neurosci Rep. 2021; 21(4): 14. doi: 10.1007/s11910-021-01103-4
Di Tella S, Pagliari C, Blasi V, Mendozzi L, Rovaris M, Baglio F. Integrated telerehabilitation approach in multiple sclerosis: a systematic review and meta-analysis. J Telemed Telecare. 2020; 26(7–8): 385–399. doi: 10.1177/1357633X19850381
Scott Kruse C, Karem P, Shifflett K, Vegi L, Ravi K, Brooks M. Evaluating barriers to adopting telemedicine worldwide: a systematic review. J Telemed Telecare. 2018; 24(1): 4–12. doi: 10.1177/1357633X16674087
Annaswamy TM, Verduzco-Gutierrez M, Frieden L. Telemedicine barriers and challenges for persons with disabilities: COVID-19 and beyond. Disabil Health J. 2020; 13(4): 100973. doi: 10.1016/j.dhjo.2020.100973
Niknejad N, Ismail W, Bahari M, Nazari B. Understanding telerehabilitation technology to evaluate stakeholders’ adoption of telerehabilitation services: a systematic literature review and directions for further research. Arch Phys Med Rehabil. 2021; 102(7): 1390–1403. doi: 10.1016/j.apmr.2020.12.014
Grimes DA, Schulz KF. Cohort studies: marching towards outcomes. Lancet. 2002; 359(9303): 341–345. doi: 10.1016/S0140-6736(02)07500-1
Telehealth coverage in California. California Physical Therapy Association. Accessed April 13, 2022.https://www.ccapta.org/page/CaliforniaTelehealth
News Now Staff. CMS guidance allows PTs, PTAs in private practice to provide services via telehealth. American Physical Therapy Association. April 30, 2020. Accessed July 5, 2022.https://www.apta.org/news/2020/04/30/cms-guidance-allows-pts-ptas-in-private-practice-to-provide-services-via-telehealth
Koma W, Cubanski J, Neuman T. FAQs on Medicare coverage of telehealth. Kaiser Family Foundation. May 23, 2022. Accessed July 5, 2022.https://www.kff.org/medicare/issue-brief/faqs-on-medicare-coverage-of-telehealth
Kurtzke JF. Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS). Neurology. 1983; 33(11): 1444–1452. doi: 10.1212/wnl.33.11.1444
Walk Score. 2022. Accessed April 7, 2022.https://www.walkscore.com/professional/research.php
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007; 19(6): 349–357. doi: 10.1093/intqhc/mzm042
Westfall PH, Tobias RD, Wolfinger, RD. Multiple Comparisons and Multiple Tests: Using the SAS System. SAS Institute Inc; 2011.
Ennis M, Thain J, Boggild M, Baker GA, Young CA. A randomized controlled trial of a health promotion education programme for people with multiple sclerosis. Clin Rehabil. 2006; 20(9): 783–792. doi: 10.1177/0269215506070805
Shaw MT, Best P, Frontario A, Charvet LE. Telerehabilitation benefits patients with multiple sclerosis in an urban setting. J Telemed Telecare. 2021; 27(1): 39–45. doi: 10.1177/1357633X19861830
Almathami HKY, Win KT, Vlahu-Gjorgievska E. Barriers and facilitators that influence telemedicine-based, real-time, online consultation at patients’ homes: systematic literature review. J Med Internet Res. 2020; 22(2): e16407. doi: 10.2196/16407
Rimmer JH, Thirumalai M, Young HJ, . Rationale and design of the Tele-Exercise and Multiple Sclerosis (TEAMS) study: a comparative effectiveness trial between a clinic- and home-based telerehabilitation intervention for adults with multiple sclerosis (MS) living in the deep south. Contemp Clin Trials. 2018; 71: 186–193. doi: 10.1016/j.cct.2018.05.016
Hale-Gallardo JL, Kreider CM, Jia H, . Telerehabilitation for rural veterans: a qualitative assessment of barriers and facilitators to implementation. J Multidiscip Healthc. 2020; 13: 559–570. doi: 10.2147/JMDH.S247267
Williams AM, Bhatti UF, Alam HB, Nikolian VC. The role of telemedicine in postoperative care. Mhealth. 2018; 4: 11. doi: 10.21037/mhealth.2018.04.03
Dubin JM, Wyant WA, Balaji NC, . Telemedicine usage among urologists during the COVID-19 pandemic: cross-sectional study. J Med Internet Res. 2020; 22(11): e21875. doi: 10.2196/21875
Lopez AM, Lam K, Thota R. Barriers and facilitators to telemedicine: can you hear me now? Am Soc Clin Oncol Educ Book . 2021; 41: 25–36. doi: 10.1200/EDBK_320827
PRIOR PRESENTATION: This work was accepted for presentation as an abstract at the 2022 Combined Sections Meeting, San Antonio, Texas.
FINANCIAL DISCLOSURES: Dr Bove is funded by the NMSS Harry Weaver Award. She has received consulting and advisory board fees from Alexion, Biogen, EMD-Serono, Genzyme-Sanofi, Novartis, and Roche-Genentech and research support from Akili Therapeutics, Biogen, and Roche Genentech. Dr Gopal, Ms Bonanno, and Dr Block declare no conflicts of interest.
FUNDING/SUPPORT: None.







