Publication
Research Article
International Journal of MS Care
Symptom Co-occurrences Associated with Smoking in Individuals with Relapsing-Remitting Multiple Sclerosis
Author(s):
Background: The impact of tobacco on the multiple sclerosis (MS) disease process and symptoms is complex and not clearly understood. Tobacco may be used to self-treat some symptoms but also seems to intensify others. Studies to date have not characterized co-occurring symptoms (symptom patterns) and their association with tobacco use.
Methods: This study describes tobacco use in patients with relapsing-remitting MS and associated symptoms and symptom co-occurrences. In this cross-sectional study, 101 participants with an average age of 43 years completed a survey adapted from the Behavioral Risk Factor Surveillance System and the revised MS-Related Symptom Checklist. Data reduction was performed using factor analysis on the 43 items of the checklist, and linear regression was used to detect associations between symptom clusters (factors) and smoking.
Results: Using the factor analysis result, the linear regression analysis found that tobacco use is positively associated with co-occurring symptoms and symptoms of factor 1: Mental/Emotional (anxiety, loneliness, depression, and difficulty sleeping) and factor 4: Neuro/Autonomic (urinary).
Conclusions: Smoking is associated with patterns of symptoms. The study of MS and tobacco use over time will allow determination of the temporal pattern of tobacco use and MS symptoms.
Multiple sclerosis (MS), an autoimmune, neurodegenerative disease, afflicts more than 1 per 1000 people in the United States.1 2 MS damages the myelin sheath and axons, resulting in impaired transmission of action potentials.3 Relapsing-remitting MS (RRMS) is characterized by relapses or exacerbations followed by complete or incomplete remissions. Most patients with RRMS will eventually enter a progressive phase known as secondary progressive MS. Approximately 20% of patients with MS have primary progressive MS, a type of MS in which the symptoms continuously worsen from the time of onset without relapses. The disease is associated with chronic, debilitating signs and symptoms that often adversely affect the individual's most productive years and everyday life.3–5 Despite experiencing multiple symptoms, many patients with MS engage in unhealthy behaviors, such as smoking, at rates similar to those of the general population.6
Associations among smoking, the risk of developing MS, and disease progression have been reported.7–9 In a large Norwegian general population sample of more than 22,000 people, the risk of developing MS was significantly higher in those who had ever smoked versus those who had never smoked.7 Smoking also contributes to increased fracture risk and increased disease activity. Finally, smoking in those with MS is associated with delay in diagnosis, increased progression,9 and lower quality of life.
A longitudinal study showed that tobacco use in patients with MS results in worsening of vision, urinary problems,6 depression, and anxiety and that these effects are similar to effects in the general population. Specifically, heavy smokers were found to have a higher incidence of visual defects than nonsmokers.9 In addition, tobacco may modulate neuroendocrine responses to stressors and inflammatory processes leading to demyelination.10 Nicotine is a central nervous system and cardiovascular stimulant. However, patients with MS who use tobacco have a higher rate of disability as determined by the Expanded Disability Status Scale (EDSS)10 11 and lower quality of life12 13 than those who do not smoke. Similarly, in a nationally representative sample of veterans with MS, Turner and colleagues14 found that poorer self-reported mental health was associated with a greater likelihood of current tobacco use. This is consistent with the literature suggesting that depression may be both a risk factor for and a consequence of smoking.15 Tobacco use may function as a type of self-medication for psychiatric symptoms, such as depression and anxiety.14–16
These studies have limitations. Most studies did not address well-defined single symptoms (eg, psychological symptoms [depression]) or investigated only one symptom at a time rather than groups of symptoms regarding tobacco use. No studies have examined tobacco use co-occurrences (never, current, ever, and regular smoker) and symptom co-occurrences (several symptoms that occur together) in patients with RRMS.
Although patients with RRMS may use tobacco as a means of lessening MS symptoms, tobacco use may also increase the occurrence and severity of other symptoms. To fully appreciate the reciprocal relationship, a clearer understanding of the associations between tobacco use and the co-occurrences of MS symptoms is needed. This study aims to identify symptoms and symptom co-occurrences associated with tobacco use in patients with RRMS.
Methods
This cross-sectional descriptive study analyzes data collected as a follow-up to a larger study. After the institutional review board of Saint Louis University (St. Louis, MO) approved the study, participants were approached by the study investigator (PN) and a neurologist (FPT) and given information about the study. The study investigator obtained written informed consent on the day of the clinical visit. Face-to-face interviews were conducted to collect demographic and medical information, tobacco use status, and symptoms.
Participants
A convenience sample of individuals with RRMS (N = 101) were asked to participate. Recruitment, screening, and inclusion criteria have been described elsewhere.17 Participants were recruited from two midwestern MS clinics during routine clinic visits and by e-mail invitations sent to patients with RRMS using a list provided by the local chapter of the National Multiple Sclerosis Society. Eligibility criteria included a diagnosis of RRMS, age older than 18 years, and willingness/ability to participate and give informed consent.
Measures
Descriptive information, including demographic characteristics (eg, age, sex, race, and time since diagnosis), was collected using a researcher-developed questionnaire. Medical information, including type of disease-modifying MS medication used, was obtained from medical record review and self-report for descriptive purposes and was not used for the final analysis.
Neurologic disability status was assessed using the self-report EDSS (SR-EDSS),18 in which bladder, visual, cerebral or mental, and “other” functions are rated based on a standard neurologic examination with ordinal scales ranging from 0 to 5 or 6. The SR-EDSS is a standard rating scale for neurologic function in MS and validates well with the physician version.18 19
MS symptoms were assessed using a revised version of the MS-Related Symptom Checklist (R-MS-RS).20 Revisions consisted of adding items generated from focus group data17 and a single open-ended question designed to elicit reports of recent co-occurring symptoms. Participants rated the frequency of each symptom on a 6-point scale from never (0) to always (5). The total MS-RS score ranges between 0 and 180, with a higher score indicating symptoms that are more frequent. The R-MS-RS included 17 additional symptoms, for a total of 43 symptoms. Test-retest reliability with the added items included was completed over a 2-week period and was calculated with a correlation coefficient of 0.89.17
MS Symptom Co-occurrences
We used exploratory factor analysis to reduce the 43 MS symptoms to a lower number of variables and to identify empirically related groups of symptoms. Factors are based on empirically derived groupings (ie, co-occurrence) of items (symptoms in this case) that are believed to represent a more general underlying construct. The number of factors chosen (n = 10) for the factor analysis was based on the eigenvalues and the interpretability of the components.21 22 Each symptom's factor score coefficient that was produced by the factor analysis for each factor represented the strength of the relationship between the symptom and the latent factor and, thus, was treated as the relative weight of that symptom on the factor (eg, sensation). The factor scores (eg, sensation score) are a weighted sum of the loaded symptoms for each participant. Factors were then labeled based on the symptoms with the highest coefficients or factor loadings (>0.500) (eg, sensation).
Tobacco Use Status
To measure tobacco use we used a subset of the Behavioral Risk Factor Surveillance System tobacco use questions.23 The participants were asked four questions: “Have you smoked at least 100 cigarettes in your life?” “How long has it been since you last smoked cigarettes regularly?” “Do you now smoke cigarettes every day, some days, or not at all?” “On a typical day now, if you are smoking, or in the past when you smoked, how many cigarettes did/do you smoke?” From these four questions we derived four tobacco use variables: 1) ever smoked 100 cigarettes (yes/no); 2) recency of regular smoking (never a regular smoker; <10 years ago, regular smoker but >6 months ago; or regular smoker in the past 6 months); 3) currency, with current smokers smoking at least 100 cigarettes ever and reporting smoking every day or on some days now (never smoker, smoker but not current, or current smoker); and 4) quantity smoked (never or not in past 6 months, 1–5 cigarettes per day in the past 6 months, 6–19 cigarettes per day in the past 6 months, or a pack a day or more in this same period). The last two variables provide graduated categories, which allowed testing for dose-response relationships with MS symptoms.
Statistical Analysis
Chi-square tests for categorical variables and unpaired t tests for continuous variables were used to analyze the difference between ever smokers and never smokers. Demographic variables included age, sex, racial/ethnic category, time since diagnosis, and SR-EDSS score. Percentages were used for current, ever, and regular smokers.
The ten symptom factors (factor scores) were used in the further analysis as continuous variables. To examine the symptom pattern scores in relation to tobacco use, we used independent-samples t tests and then linear regression adjusting for race and age, the only covariates significantly associated with the factor scores and tobacco variables in the bivariate analyses. Data were analyzed using a statistical software program (IBM SPSS Statistics for Windows, version 19.0; IBM Corp, Armonk, NY). Study data were collected and managed using REDCap electronic data capture tools hosted at Washington University (St. Louis).24
Results
Sample Demographics
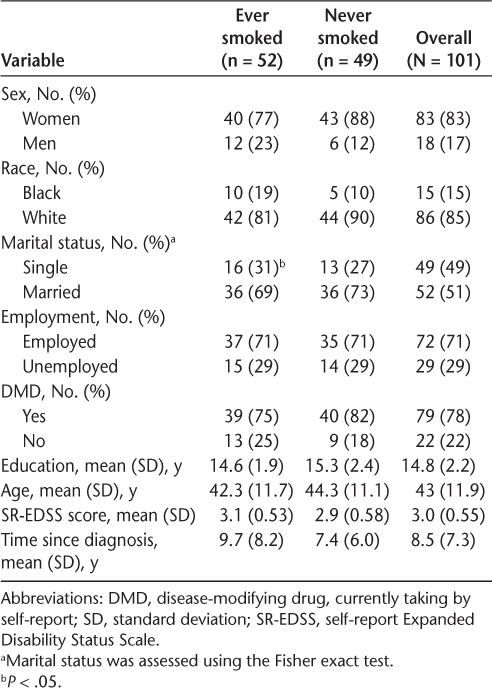
A total of 101 patients with RRMS took part in the study. Table 1 displays the sample demographics of the ever smokers and never smokers. The average age was 43 years. Most of the overall sample was female (83%), white race (85%), and married (51%). The overall mean duration of MS disease was 8.5 years and mean SR-EDSS score was 3 (Table 1). The overall prevalence of smoking (past or present) in the present sample was 52%, which is higher than the 45.5% obtained in patients with MS responding to the 2002 and 2008 iterations of the Integrated Health Interview Survey, a nationally representative general population sample of more than 74,000 people.6 Ever smokers in the present sample were more likely to be single compared with never smokers (P = .03). All other demographic characteristics and disability status (eg, SR-EDSS score, age, sex, race, and educational level) were not associated with lifetime smoking status.
Sample demographics by smoking status in people with relapsing-remitting multiple sclerosis
Factor Analysis Findings
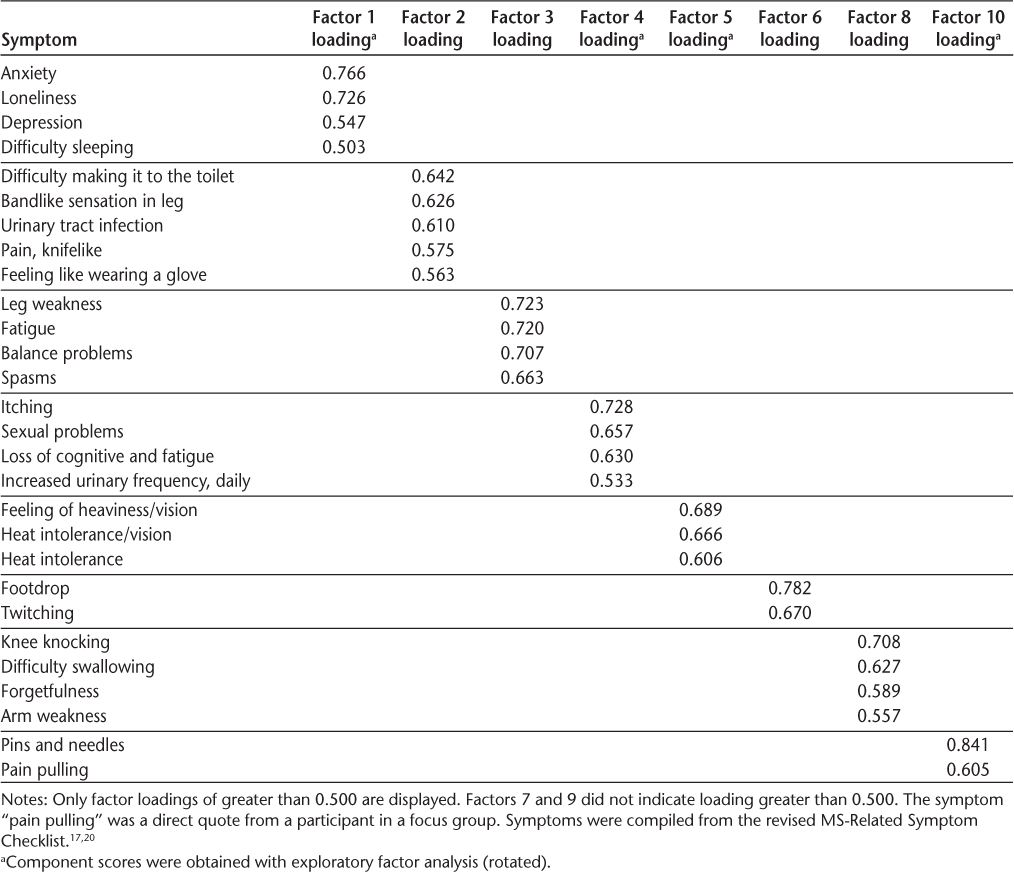
The factor analysis of the symptoms from the R-MS-RS produced a rotated factor matrix comprising ten factors (Table 2). We then listed these factors and the symptom labels that we attached to each factor, along with the loadings. The first factor significantly associated with smoking status was labeled Mental/Emotional (factor 1). It had the highest factor loadings (>0.500) on symptoms of depression, loneliness, anxiety, and difficulty sleeping. Factor 4, Neuro/Autonomic, was significantly associated with race, with high factor loadings on symptoms of urinary and sexual problems. Factor 5 was labeled Heat Intolerance/Vision and had high factor loadings on symptoms of heat intolerance and vision problems. Factor 10, labeled Sensation, had high factor loadings on symptoms of pins and needles and pain pulling (direct participant quote).
Factor analysis: ten-factor solution for multiple sclerosis (MS) symptoms (N = 101)
Symptoms by Smoking Status and Demographic Characteristics
Four factors of the 10 extracted (presented in Table 2) were associated with smoking status (never smoked, smoked but not currently, and current smoker) and race (Table 3). The associations with current smoking indicated that higher factor scores (indicating more symptoms) were associated with being a current smoker. The association with race indicated that African American patients had higher levels of symptoms than white patients. Participants who ever smoked at least 100 cigarettes (past or present smokers) had a significantly higher score on the Mental/Emotional symptoms (factor 1), whereas those who had smoked on a regular basis but not currently reported more Heat Intolerance/Vision problems (factor 5). For those who ever smoked 100 cigarettes, there was an association with the Mental/Emotional factor score (eg, symptoms of depression, anxiety) compared with never smokers after adjusting for race and age. For example, solving the linear regression equation mathematically for a hypothetical case indicates that an individual who is African American, of average age (42 years old), and a smoker would have a 34% higher Mental/Emotional symptom score (factor 1) than a similar person who has never been a smoker. Those endorsing “ever a regular smoker but not currently a smoker” likewise had an association with the Neuro/Autonomic symptom score (factor 4) (eg, increased urinary frequency) compared with never regular smokers when controlling for race and age. Specifically, African American patients who ever smoked would have 36% higher Neuro/Autonomic symptom scores than those who never smoked.
Regression of smoking status on symptom factor scores adjusting for race and age in 101 persons with relapsing-remitting multiple sclerosis
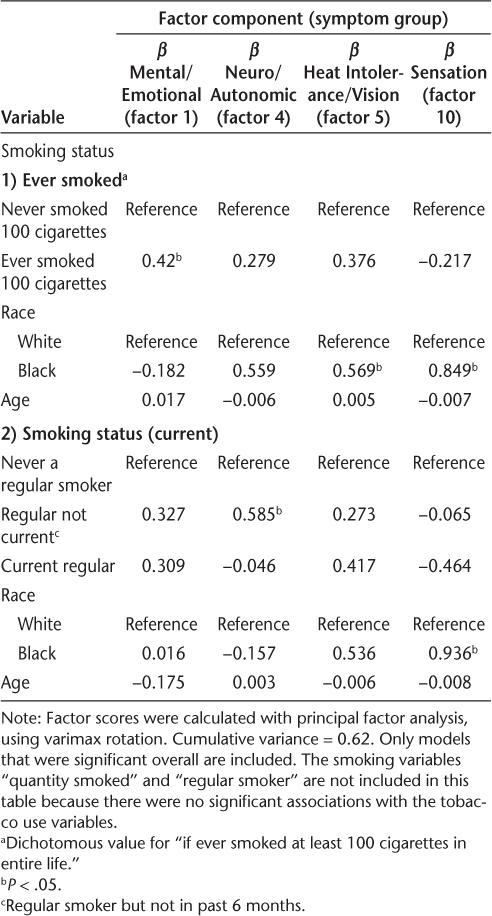
Being African American was associated with higher scores on the Heat Intolerance and Sensation symptoms (factors 5 and 10). No associations were found between race and the other symptom factor scores and either the quantity of cigarettes smoked or the four-category regular smoking variable.
Discussion
To our knowledge, this is the first study to examine symptom co-occurrences (clusters) and smoking in people with RRMS. Previous studies8 10 are not recent or did not examine more than one symptom at a time (ie, symptom co-occurrence).11–13 The present results imply that Mental/Emotional and Heat Intolerance/Vision symptom factors are associated with tobacco use. However, we did not see dose-response relationships between the level of symptoms and either of the measures that could have shown a dose-response relationship (the tobacco use currency or quantity variables). A smoking tool with greater detail may complement the Behavioral Risk Factor Surveillance System questions used in the present study and benefit future studies. Replication of this study with a cohort study design using various types of MS would more fully clearly explain the co-occurring patterns of symptoms and smoking behaviors in this population.9
Because these data suggest that the mental health symptoms of anxiety, loneliness, depression, and difficulty sleeping co-occur, attention to this cluster may be necessary as part of care and routine screening of depression. Because we did not use screening tools for either depression or anxiety, future investigations with more comprehensive mental health screening using a gold standard assessment are warranted.25
Practically speaking, the increases in the Mental/Emotional symptoms and Neuro/Autonomic symptom between those with and without the relevant smoking behavior (34% and 36%, respectively) have no absolute clinical meaning and may or may not be clinically significant due to the MS-RS frequency scoring and the subjective nature of the symptoms. Thus, it is imperative that people with MS are adequately assessed for smoking status and symptoms at each clinical encounter.
The present findings underscore the need for comprehensive assessment of symptoms and smoking history at each clinic visit. The use of a short MS-related symptom scale may assist in understanding the possible association with certain co-occurring symptoms and smoking. Future larger studies should consider separating never smokers from those who have quit smoking. Although the causal direction between symptoms and smoking is unclear, a clinical interview that includes multidisciplinary care would help inform treatment. It was not possible from the present data to separate effects on symptoms from previous tobacco use and the use of tobacco in response to certain symptoms (self-treatment). However, as with depression, it may be that both phenomena occur, that those with greater symptoms are more likely to smoke, and that those who smoke have more symptoms. Next steps include large prospective studies to determine this and to tease apart issues of causality. However, associations between reported past smoking behavior, without a similar association with current behavior, suggest that past tobacco use is associated with current symptoms.
Although generalization of the present results is limited to patients with RRMS, this limitation is also a strength because we did not complicate interpretation by including multiple types of MS. Volunteer bias from the convenience sample of patients with RRMS may have influenced the makeup of the sample. Owing to the self-report format, tobacco use and symptoms may have been underreported. Using only a single study site, and its regional restriction to the Midwest, as well as the inclusion of only a few African American patients could also be considered limitations. Therefore, generalizability to other regions, by race, or to nonresponders cannot be assumed. Owing to the small sample size, replication of these findings is needed with larger, more geographically diverse samples. Finally, the limited sample size precluded including comorbidities in the models, and the cross-sectional design did not allow for examination of the temporal relationship between tobacco use and symptom co-occurrence.
Conclusion
This study offers an important first step in understanding the relationship between symptom groups and smoking status in patients with RRMS. Investigating the associations of symptoms and tobacco use can allow for improved management of MS through targeted symptom management and smoking cessation counseling and treatment. Decreasing tobacco use in MS should reduce health-care costs and improve quality of life. A tailored therapeutic approach may be indicated, such as discussion of the benefits of not beginning smoking or of smoking cessation in MS. For example, cessation programs might offer novel ways to quit (ie, mobile phone applications) and offer follow-up contacts. Multidisciplinary approaches that include health educators, social workers, and psychologists may be needed. Further research in this area is warranted to clarify the mechanism by which smoking affects symptom co-occurrences in RRMS and tobacco use for self-treatment in larger samples and over time.
Acknowledgments
We thank the Gateway Area Chapter of the National Multiple Sclerosis Society for assistance with recruitment.
PracticePoints
Co-occurring symptom domains for those who smoke and those who smoked in the past but quit should be assessed regularly in people with relapsing-remitting MS.
The association of smoking status with the symptom factors Mental/Emotional and Neuro/Autonomic highlights the need for increased diligence in screening for smoking status and enrolling smokers in cessation programs.
References
Courtney AM, Treadaway K, Remington G, Froman E. Multiple sclerosis. Med Clin North Am. 2009;93:451–476.
MS prevalence. National Multiple Sclerosis Society website. http://www.nationalmssociety.org/About-the-Society/MS-Prevalence. Retrieved May 17, 2016.
Berger JR. Functional improvement and symptom management in multiple sclerosis: clinical efficacy of current therapies. Am J Manag Care. 2011;17(suppl 5):S146–S153.
Zwibel HL, Smrtka J. Improving quality of life in multiple sclerosis: an unmet need. Am J Manag Care. 2011;17(suppl 5):S139–S145.
Compston A, Coles A. Multiple sclerosis. Lancet. 2008;372:1502–1517.
Minnesota Population Center and State Health Access Data Assistance Center. Integrated Health Interview Series: Version 5.0. Minneapolis, MN: University of Minnesota; 2012.
Koch M, van Harten A, Uyttenboogaart M, De Keyser J. Cigarette smoking and progression in multiple sclerosis. Neurology. 2007;69:1515–1520.
Coyne KS, Kaplan SA, Chapple CR, et al. Risk factors and comorbid conditions associated with lower urinary tract symptoms: EpiLUTS. BJU Int. 2009;103(suppl 3):24–32.
Manouchehrinia A, Tench CR, Maxted J, Bibani RH, Britton J, Constantinescu CS. Tobacco smoking and disability progression in multiple sclerosis: United Kingdom cohort study. Brain. 2013;136:2298–2304.
Marrie RA, Horwitz RI, Cutter G, Tyry T, Vollmer T. Smokers with multiple sclerosis are more likely to report comorbid autoimmune diseases. Neuroepidemiology. 2011;36:85–90.
D'Hooghe MB, Haentjens P, Nagels G, De Keyser J. Alcohol, coffee, fish, smoking and disease progression in multiple sclerosis. Eur J Neurol. 2012;19:616–624.
Marrie RA, Hanwell H. General health issues in multiple sclerosis: comorbidities, secondary conditions, and health behaviors. Continuum (Minneap Minn). 2013;19:1046–1057.
Weiland TJ, Hadgkiss EJ, Jelinek GA, Pereira NG, Marck CH, van der Meer DM. The association of alcohol consumption and smoking with quality of life, disability and disease activity in an international sample of people with multiple sclerosis. J Neurol Sci. 2014;336:211–219.
Turner AP, Kivlahan DR, Kazis LE, Haselkorn JK. Smoking among veterans with multiple sclerosis: prevalence correlates, quit attempts, and unmet need for services. Arch Phys Med Rehabil. 2007;88:1394–1399.
Thornton LK, Baker AL, Lewin TJ, et al. Reasons for substance use among people with mental disorders. Addict Behav. 2012;37:427–434.
Pedersen W, von Soest T. Smoking, nicotine dependence and mental health among young adults: a 13-year population-based longitudinal study. Addiction. 2009;104:129–137.
Newland PK, Thomas FP, Riley M, Flick LH, Fearing A. The use of focus groups to characterize symptoms in patients with multiple sclerosis. J Am Assoc Neurosci Nurses. 2012;44:351–357.
Bowen J, Gibbons L, Gianas A, Kraft GH. Self-administered Expanded Disability Status Scale with functional system scores correlates well with a physician-administered test. Mult Scler. 2001;7:201–206.
Kurtzke JF. Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS). Neurology. 1983;33:1444–1452.
Gulick EE. Model confirmation of the MS-Related Symptom Checklist. Nurs Res. 1989;38:147–153.
Tabachnick BG, Fidell LS. Using Multivariate Statistics. 6th ed. New York, NY: Pearson Education Inc; 2012.
Newland PK, Flick LH, Thomas FP, Shannon WD. Identifying symptom co-occurrence in persons with multiple sclerosis. Clin Nurs Res. 2014;23:529–543.
Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System Survey Questionnaire. Atlanta, GA: US Department of Health and Human Services; 2011.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap): a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381.
Perkins KA, Jao NC, Karelitz JL. Consistency of daily cigarette smoking amount in dependent adults. Psychol Addict Behav. 2013;27:723–729.
Financial Disclosures: The authors have no conflicts of interest to disclose.
Funding/Support: This research was made possible by a Ruth Kirschstein National Service Award from the National Institutes of Nursing Research (1F32NR012389) and by a research grant from the International Organization of Multiple Sclerosis Nurses.







