Publication
Research Article
International Journal of MS Care
Cultivating the Multiple Sclerosis Workforce of the Future
Author(s):
Multiple sclerosis (MS) is a complex neurologic disorder that affects people with ever-changing needs. The MS health-care field has entered an era of exponential knowledge growth in which better understanding of the immunologic dysregulation of the disease has translated into an expanding array of treatment options. It is estimated that, if it has not already, within the next decade the demands of a growing MS patient population will outstrip the number of professionals dedicated to the management of this chronic, lifelong disease. Therefore, there is a pressing need to attract and retain clinicians in this dynamic field. In response to this need, the Foundation of the Consortium of Multiple Sclerosis Centers organized a 2-day colloquium, a Mentorship Forum, on January 23–24, 2015, bringing together talented internal medicine and neurology trainees from across North America with an interest in MS and neuroimmunology. This article highlights the rationale for the MS Mentorship Forum, its structure and content, and its outcomes. We believe that the stage has been set to interest young, promising clinicians in learning more about MS and to encourage them to consider a career in this field. In so doing, we hope to contribute to the development of the next generation of MS experts to make a palpable difference in the lives of those affected by MS.
Multiple sclerosis (MS) is a complex neurologic disorder that affects people with ever-changing needs. The MS health-care field has entered an era of exponential knowledge growth in which better understanding of the immunologic dysregulation of the disease has translated into an expanding array of treatment options. Keeping abreast of the latest clinical and research developments to provide the highest standard of care poses a genuine challenge that can be met only by a dedicated and knowledgeable workforce. It is estimated that within the next decade, the demands of a growing MS patient population will outstrip the number of professionals dedicated to the management of this chronic, lifelong disease; perhaps this is already the case.1 Therefore, there is a pressing need to attract and retain clinicians in this dynamic field.
In light of this need, the Foundation of the Consortium of Multiple Sclerosis Centers (FCMSC) organized a 2-day colloquium, a Mentorship Forum, on January 23–24, 2015, bringing together talented internal medicine and neurology trainees from across North America with an interest in MS and neuroimmunology. Led by a team of expert faculty and peer mentors (colleagues who recently completed their own MS-related fellowship), the program provided a platform during which key concepts of MS pathophysiology, diagnosis and prognosis, treatment, monitoring, and sustained care were discussed. The program was complemented by structured as well as informal discussions about career options and their unique challenges, work-life balance, and future prospects for careers in MS.
This article highlights the rationale for the MS Mentorship Forum, its structure and content, and its outcomes. We believe that the stage has been set to interest young, promising clinicians in learning more about MS and to encourage them to consider a career in this field. In so doing, we hope to contribute to the development of the next generation of MS experts to make a palpable difference in the lives of those affected by MS.
MS Mentorship Forum
Rationale
MS is a chronic disease and the most common cause of nontraumatic neurologic disability in young adults in the Western world. The disease typically affects individuals at the prime of their formative and working lives, thus having an enormous socioeconomic and psychological impact. People with MS require comprehensive care to manage the diversity of clinical symptoms and disability that can ensue, especially because this directly affects their quality of life. The complexity of the disease has ignited a seismic shift in its health-care delivery in which multidisciplinary teams delivering subspecialty expertise is becoming the expected clinical paradigm.
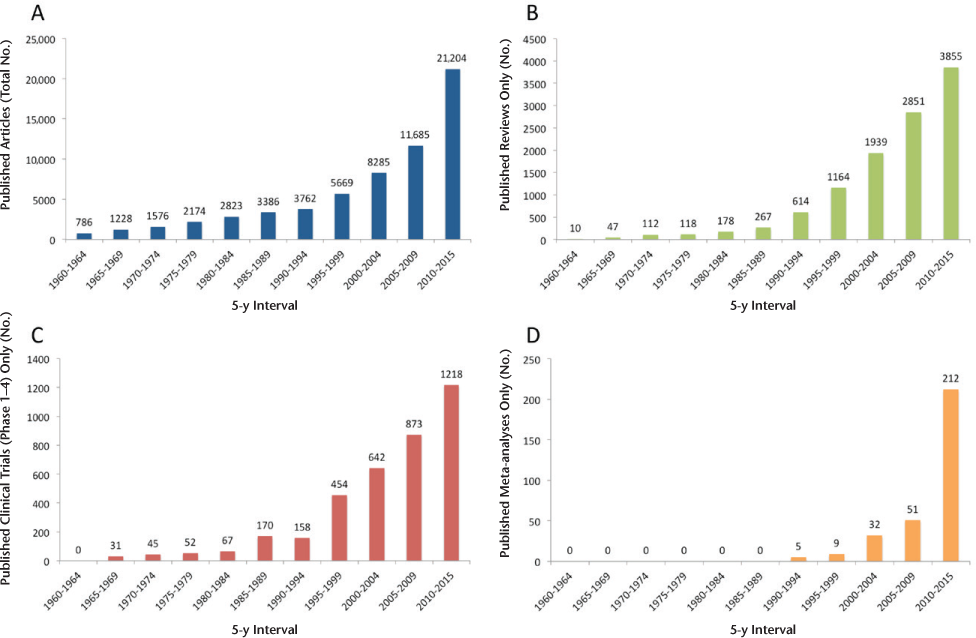
The basic pathophysiologic underpinnings of MS are being unraveled at an escalating pace. Advances in neuroimmunology, neuropathology, neuroimaging, genomics, and neuropharmacology have made it increasingly difficult for even MS specialists to remain up-to-date. The accelerated pace of interest and knowledge acquisition in MS is reflected in the exponential rise in MS-related publications during the past several decades (Figure 1). This poses a daunting challenge for busy general neurologists and emphasizes the need for fellowship training in MS clinical care and neuroimmunology. The rapidly increasing availability of many effective disease-modifying and symptomatic treatments for MS is a potential draw to new trainees who are looking for a dynamic, impactful career in medicine.
Publications in the multiple sclerosis (MS) field (1960–present)
Exposure to neuroimmunology in neurology residency is a key step to attracting the brightest neurology trainees to a career in MS and related disorders. Although most neurology residency programs expose residents to neuroimmunologic disorders, the mechanisms through which neurology trainees obtain experience in MS and related disorders are highly variable throughout the country. Some institutions offer dedicated, structured rotations and didactic sessions in neuroimmunology, and others provide exposure through more general neurology service–related settings. Neurology trainees can be left with the difficult task of assembling reading lists, arranging clinical rotations, and seeking mentorship support to fulfill training needs and interests. To our knowledge, there is no centralized resource aimed at neurology trainees that provides relevant, up-to-date information about key concepts in neuroimmunology, a directory of fellowship training opportunities, mentorship support networks, and future career options in the field of MS and related diseases. Furthermore, enduring forums in which neurology trainees interested in a career in MS and neuroimmunology can interact with and gain advice/support from junior and senior faculty from across the country in an ongoing and structured way are underrepresented. The FCMSC Mentorship Forum sought to address these critical unmet needs.
Structure and Content
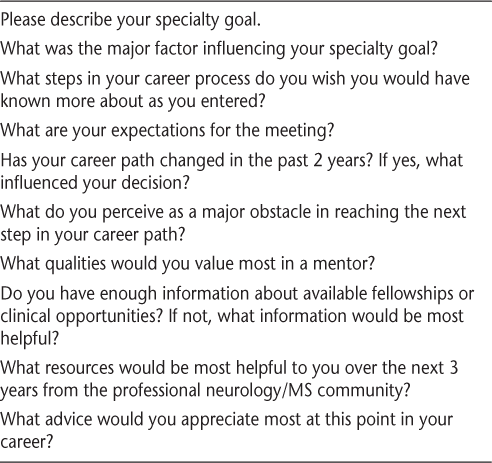
The Consortium of Multiple Sclerosis Centers (CMSC) has more than 220 CMSC-affiliated institutions across Canada and the United States. Neurology trainees from these CMSC-affiliated institutions were invited to apply to participate in a 2-day Mentorship Forum about MS and related disorders in Newark, New Jersey, on January 23–24, 2015. Trainee participants (neurology residents and neuroimmunology fellows) were recruited through calls for application to an overall list of 33 neurology academic and training programs across North America. Information about the program was also disseminated to recent recipients of FCMSC medical student research scholarships and FCMSC resident scholarships and their mentors as well as to all professional members of the CMSC. Applicants were nominated by their program directors and selected by a review committee composed of CMSC and FCMSC leadership as well as the program chair. Twenty-three neurology residents from all years of training were selected. To gauge the needs and interests of the selected participants, neurology residents were asked to complete a premeeting survey to help guide the structure and content of the program (Table 1).
Foundation of the Consortium of Multiple Sclerosis Centers Mentorship Forum premeeting survey
The participant responses highlighted several important themes. First, participant specialty goals were mainly neuroimmunology and MS, as expected. Several residents cited interest in various related fields, including autoimmune disease, neurogenetics, neuropediatrics, and neuro-ophthalmology, reflecting the breadth of MS as a subspecialty. The challenges associated with MS diagnosis and treatment, previous exposure to patients with MS (which may be within residency or a personal connection), and involvement in MS-related research were factors that influenced participant interest in the field. Major obstacles in reaching a decision to subspecialize in MS and neuroimmunology included a lack of information about fellowships and career options in the field, inadequate funding (or unclear mechanisms of securing funds) for clinical and research fellowships, and insufficient exposure to neurologists with expertise in MS and neuroimmunology in their residency programs. In line with this, participants clearly voiced that the scope of the FCMSC mentorship program should include the provision of education about core principles of MS (and more broadly neuroimmunology), clinical classifications, and the scope and evolution of current MS care. Networking opportunities with peers who recently completed residencies or fellowships and exposure to potential mentors in the MS field were also deemed to be important objectives. In particular, residents requested a forum in which information about fellowship programs and career opportunities and challenges in the current health-care environment could be discussed candidly with dedicated, enthusiastic, and compassionate MS clinicians. The need for content development for Web-based programs for professionals-in-training (PiTs) and the creation of an MS interest group were identified. These survey results greatly influenced the structure, content, and outcomes of the program.
The 2-day FCMSC colloquium used a variety of educational strategies. Presentation formats included seminars about a range of neuroimmunology topics; small-group, neuroimmunology-focused, case-based discussions; interactive large-group experiential sharing; and informal, fireside chats about medical/neurology topics and career issues facing neurology trainees. The broad objectives of the Mentorship Forum included 1) identifying the appropriate diagnosis and management strategies for MS as well as anticipating future challenges, 2) discussing the vital role that clinicians and researchers play in the care of patients with MS, 3) developing content and resources for other PiTs with an interest in neuroimmunology and MS as a career path, and 4) providing a platform of networking and mentorship opportunities for future leaders in the field.
Outcomes
Knowledge Transfer
The foundation of the mentorship program was built on a comprehensive series of didactic seminars on important topics in the MS field ranging from basic principles of MS (including epidemiology, pathology, and immunology) to diagnostic criteria, differential diagnosis, and treatment strategies. Presentations included an in-depth discussion of immunopathology and imaging and their effect on the understanding of the MS disease process and the importance of MRI in diagnosis and treatment monitoring. Participants were introduced to the complexity of MS symptoms and psychosocial issues (and their management) facing people with MS, including fatigue, cognitive dysfunction, depression, and pain. Also highlighted were the significant unmet needs in MS care and the importance of health and wellness promotion. Common threads united each of the seminars: the pressing need to recruit bright, dedicated MS clinicians and researchers and the importance of having collaborative, multidisciplinary health-care teams to deliver optimal care for people with MS.
Career Paths in Neurology and in MS as a Specialty
Career paths in neurology (and in particular MS/neuroimmunology) and the influence of the current health-care environment on future opportunities were important discussion points led by faculty. It is well recognized that the mode of health-care delivery is changing. In the future, small, single-specialty private practices or single practitioners will likely be replaced by integrated, multidisciplinary subspecialty MS care centers, especially in major metropolitan areas. This will be an important shift in the MS field to accommodate the increasingly complex and rapidly evolving management of people with the disease. The focus of newer health-care delivery will be on efficient delivery of quality care, and this means delivering health-care value. Patient-centered outcomes2 will be an important tenet wherein people with MS will be active participants in the clinical decision-making process and assessors of excellence in health-care delivery. These imminent changes will be positive for MS clinicians (and their patients) in allowing for optimized health-care delivery and outcomes.
Subspecialty expertise in MS was discussed as being an area of increasing demand, justifying recruitment of young and talented clinicians into the field. Recent evidence suggests that health-care reform and the increased availability of insurance will increase the demand for health-care access and delivery.1 This is particularly salient in neurology, where there is a sizable shortfall in the number of neurologists1 needed to treat a rapidly increasing number of patients with chronic neurologic diseases. The necessity of comprehensive clinical care for people with MS demands a multidisciplinary team approach. MS specialists can expect to interact with an expanding team of health-care providers, including (but not limited to) physiatrists, physical therapists, occupational therapists, speech and language pathologists, primary-care physicians, nurse practitioners and MS nurse specialists, physician assistants, neuropsychologists, psychiatrists, psychologists, social workers, pediatric neurologists, ophthalmologists, orthopedic surgeons, and urologists. With the recent explosion in the number of disease-modifying therapies available to treat people with MS, there is an increasing need to recognize and manage associated toxicities that may require medical support from other specialties, such as cardiology, nephrology, hematology, endocrinology, and rheumatology. Adding a further layer of intricacy in response to the MS-related knowledge “boom,” MS clinicians will likely become subspecialized; this goes beyond focusing on MS to becoming expert in neuroimmunology, neuroinfectious disease, neuroimaging, neuropathology, and neurorehabilitation. It is clear that the landscape of MS health-care delivery is changing, which requires the development of adaptable and highly specialized MS clinicians and researchers. There is an air of excitement in the MS and neuroimmunology fields about the possibilities that lie ahead. These concepts invigorated the participants and faculty of the FCMSC Mentorship Forum.
Once clarifying the pressing need for MS specialists, the faculty presented a multitude of career options available to resident-participants. The diversity of MS clinical care and research has created the need to fill various niches in the field, ranging from full-time clinicians to full-time bench researchers and a combination of both. Most clinicians involved in MS care will be involved in some form of clinical research (ie, clinical trials or postmarketing surveillance). The combination of clinical duties with research provides a rewarding platform to engage patients while increasing knowledge to eventually provide therapeutic benefit for people with MS. Patient advocacy and government reform are an integral component of MS care, and access to treatment and clinical investigation often necessitate the participation of MS clinicians in health policy. The multifaceted nature of the MS specialty demands interaction with multiple disciplines, medical specialties, and policy makers to achieve the safest and most cost-effective outcomes for people with MS.
Participants were reminded that MS clinicians are often master diagnosticians and, by extension, should be well equipped to teach. Because MS can affect any part of the central nervous system, MS clinicians need to be highly skilled in obtaining a patient's neurologic history and performing a neurologic examination. Because efferent and afferent visual disorders are prominent and visual testing has become widespread for diagnosis and monitoring, the new MS neurologist must also have at least basic proficiency in the neuro-ophthalmologic examination and in interpreting visual testing. In addition, the MS clinician needs to demonstrate a commanding knowledge of differential diagnosis and MS mimics. The required repository of knowledge of anatomy, pathophysiology, immunology, and neuroimaging equips MS clinicians with the foundation needed to be effective teachers. As a result, MS clinicians often play an important part in medical school and resident education. This provides yet another career opportunity for budding neurologists interested in entering the field of MS.
Neurology Trainee Issues and Options
Neurology residents are at a critical crossroads regarding their future career choices. Although the multitude of career options are generally perceived as positive, many participants found that they are insufficiently armed with the knowledge needed to make an informed decision about their long-term careers. It was recognized that the MS field is broadening in scope, with the specialty more appropriately fitting under the expanding umbrella of neuroimmunology. Participants indicated that a Web-based resource with the “top 25” articles relevant to the subspecialty would help them fill an important knowledge gap and allow them to understand better whether the field suits their interests.
How MS fellowship training programs are adapting to the broadening clinical landscape was questioned. In part, this relates to the lack of information about the available MS/neuroimmunology training programs at institutions across the United States and Canada. Furthermore, when MS/neuroimmunology training programs are identified, there is an obvious lack of standardized information about their curricula and requirements and expectations (ie, amount of time available for clinical service provision, research, and education). The participants highlighted a critical need to improve information about neurology programs offering fellowships in the MS/neuroimmunology field.
From a practical point of view, participants were given advice about how to select a subspecialty training program that best fits their needs and learning style. Faculty encouraged participants to inquire about the duration and structure of programs and to take the opportunity to visit and possibly undertake a clinical or research rotation at the institutions of interest. This can provide important insight into the mechanics and ethos of the subspecialty program to help trainees determine whether the program is a good fit. It was recommended that neurology trainees develop a constructive dialogue with subspecialty program directors about clinical, research, and education options that may be available to them and whether the program offers any flexibility to accommodate specific professional goals. This dialogue necessitates a bidirectional approach wherein MS/neuroimmunology program directors and neurology trainees both engage in the training decision-making process. It is possible for trainees to inquire about spending time at other institutions if their fellowship does not provide enough exposure to certain areas of neuroimmunology.
Need for Guidance and Mentorship
A recurring theme raised by the forum participants was the need to access both informal guidance and more formal mentorship support about MS fellowship and career decisions. Neurology trainees find it difficult to access adequate subspecialty support networks given the demands and time pressures associated with their training. Many institutions do not offer MS/neuroimmunology subspecialty clinical rotations, making it difficult for residents to connect with relevant experts to help guide career decisions. Learning from peers and MS subspecialists who have gone into the field through different paths at different institutions provides neurology trainees with a concrete idea about what to expect in a career in MS/neuroimmunology and how best to achieve their goals. Because identifying a single mentor can be a challenge, neurology residents were encouraged to seek the advice of many individuals. The need to have a national database of MS/neuroimmunology experts who would be willing to provide informal support and guidance was identified.
In addition to informal support networks, establishing a relationship with a formal mentor is beneficial. A mentor is an experienced and trusted adviser who invests in the well-being of a colleague and can provide candid advice about career options and work-life balance issues. Faculty recommended that neurology trainees make a conscious effort to seek out opportunities to meet and work with MS clinicians, researchers, and educators whenever possible. Engaging in a research project with a clinician was identified as an excellent means to interact regularly and meaningfully and to establish an enduring relationship. It was stressed that a mentor need not be in one's own specialty of interest and, in fact, need not be restricted to one individual. Interestingly, faculty thought that trainees in many ways act as mentors to senior colleagues as well, bringing to light the importance of bidirectional experience and knowledge exchange in this important professional relationship.
Work-life balance is an important topic throughout clinical training. Faculty shared their personal experiences with the struggles associated with juggling career development and personal family life. The need for role models in leadership positions in MS (and in neurology, more generally) who can nurture a productive career while preserving a fulfilling family life was highlighted. This was thought to be a particularly challenging issue for women. Various ways to address these topical issues were discussed. It was recognized that compartmentalizing and protecting time outside of work is critical to one's personal happiness and health. Personal well-being has a powerful effect on professional motivation and success. The concept of supervisors or other decision makers focusing on the well-being of their trainees (and employees) to accommodate their evolving needs, regardless of sex, was stressed.
Recommendations and Next Steps
Colloquium participants had numerous, meaningful suggestions to address the needs identified throughout the Mentorship Forum. Among them were:
Gathering references, articles, and reading materials in one accessible location. Residents find it difficult to wade through an ever-increasing number of articles and references. Faculty noted that there are a dozen or more papers that every resident should read about MS and related disorders.
Providing a guide or algorithm of how to initiate medication therapy, including screening and follow-up, for newly diagnosed patients with MS. It is also important to include information about medication adverse effects and contraindications. The likelihood of treating someone with MS is high, regardless of subspecialty. Continuing education courses and case discussions are helpful.
Providing information about symptomatic management. Again, continuing education courses and case discussions are helpful.
Increasing the availability of information to arm residents with choices about fellowships. Participants noted a need for a directory of available fellowships that includes information about the structure and funding of each fellowship. A list of mentors and those willing to be contacted should accompany this listing.
Creating a dedicated MS/neuroimmunology subspecialty interest group for neurology residents to encourage experience and knowledge sharing to be created through the CMSC.
In response to these excellent suggestions, the FCMSC and the CMSC invited all participants to attend the CMSC 2015 Annual Meeting (Indianapolis, IN) and arranged a meeting with faculty and FCMSC and CMSC staff to devise a clear action plan to make these recommendations a reality. The FCMSC and the CMSC are proud to announce several initiatives that have stemmed directly from this Mentorship Forum, including:
Construction of a Web-based resource for PiTs with an interest in MS that contains summaries of disease state, diagnosis, and symptom management presentations developed by the MS Mentorship Forum.
A North American directory of training programs and institutions offering MS-related fellowships.
Creation of a CMSC special interest group (SIG) for MS residents and fellows (MS-PiTs SIG) to represent this growing group to the CMSC Board of Governors.
A password-protected LISTSERV facilitating communication among members of the proposed MS-PiTs SIG and periodic needs assessment surveys.
A bibliography of current, important MS literature compiled by the faculty.
Links to Web-based educational resources within the MS community.
Outcome measures for these initiatives will be used to monitor and continuously improve the structure of the mentoring program. We will survey program participants for their satisfaction after each meeting and solicit their ideas for new initiatives that will facilitate their careers. The number of participants who go on to MS-focused clinical or research careers will be tracked, as well as those who take on leadership roles in organizations such as the CMSC, the American Academy of Neurology, and Americas Committee on Treatment and Research in MS. The present group has already organized a new PiTs SIG supported by the CMSC. They have a website (http://www.MS-PiT.org), and the SIG co-leaders are members of the CMSC Board of Directors. Together, these actions provide the PiTs group with an enduring forum and a voice in CMSC initiatives and educational offerings at the annual meeting. The overarching goal is to provide a framework to help aspiring clinical trainees in MS-related disciplines find a community of colleagues to share the excitement of our field, enhance their education in the comprehensive care model, and increase the number of well-trained clinicians and scientists who go on to provide care and hope for people with MS.
Conclusion
The FCMSC and the CMSC are committed to the establishment of programs and resources to attract talented, up-and-coming clinicians to the exciting field of MS/neuroimmunology. The creation of a mentorship forum wherein neurology residents from across the United States and Canada can meet and interact meaningfully with faculty was a critical stepping-stone in achieving this aim. The achieved outcomes from the forum are noteworthy and fill critical information and knowledge gaps. The success of the program highlights the power of active engagement of trainees in the career decision-making process. In the future, it is anticipated that the FCMSC Mentorship Forum will extend beyond neurology trainees to include medical students, MS fellows, and an expanding network of MS faculty from across North America. At the conclusion of this pilot project, the FCMSC and the CMSC hope to engage trainees from a variety of health-care disciplines to stimulate their interest and enhance their knowledge of MS/neuroimmunology. The ultimate goals of these endeavors are to improve competence and performance in the care of patients with MS and to expand the workforce of the future.
PracticePoints
MS and neuroimmunology are rapidly expanding disciplines with exponential knowledge growth and diverse career opportunities. With the ever-increasing demands of a growing MS patient population, there is a pressing need to attract and retain clinicians in the MS and neuroimmunology fields.
The Foundation of the Consortium of Multiple Sclerosis Centers (FCMSC) Mentorship Forum is a novel initiative that aims to stimulate and nurture interest in MS and neuroimmunology by linking talented internal medicine and neurology trainees with faculty and peer mentors who are experts in these fields.
The broad objectives of the FCMSC Mentorship Forum are to 1) identify the appropriate diagnosis and management strategies for MS as well as anticipate future challenges, 2) discuss the vital role that clinicians and researchers play in the care of patients with MS, 3) develop content and resources for other professionals-in-training with an interest in neuroimmunology and MS as a career path, and 4) provide a platform of networking and mentorship opportunities for future leaders in the field.
Acknowledgments
We thank Lori Saslow (Great Neck, NY), editorial consultant, on behalf of the FCMSC and the CMSC, for her expert assistance in manuscript development, preparation, and editing.
References
Dall TM, Storm MV, Chakrabarti R, et al. Supply and demand analysis of the current and future US neurology workforce. Neurology. 2013; 81:470–478.
Patient-Centered Outcomes Research Institute website. http://www.pcori.org. Accessed May 4, 2015.
Foundation of the Consortium of Multiple Sclerosis Centers (FCMSC) MS Mentorship Forum Participants: Sudhir Aggarwal, MD, PhD, Drexel University/Hahnemann Hospital, Philadelphia, PA, USA; Thandar Aung, MD, St. Joseph's Hospital and Medical Center, Phoenix, AZ, USA; Scott Belliston, DO, University of Kansas Hospital, Kansas City, KS, USA; Idanis Berrios-Morales, MD, University of Massachusetts, Worcester, MA, USA; Miguel Mielo Bicchi, MD, Rutgers New Jersey Medical School, Newark, NJ, USA; Alison Daigle, DO, Rhode Island Hospital/Albert Brown Medical School, Providence, RI, USA; Jaclyn Rosencutter Duval, MD, University of Oklahoma College of Medicine, Oklahoma, OK, USA; Evdokia Eleftheriou, MD, University of Massachusetts Medical School, Worcester, MA, USA; Carla Marina Francisco, MD, Children's Hospital, Los Angeles, CA, USA; Jose Luis Gonzalez, MD, University of Miami/Jackson, Miami, FL, USA; Tirisham Gyang, MD, University of Rochester Medical Center, Rochester, NY, USA; Michelle Hadden-Young, MD, CCFP, Memorial University of Newfoundland, St. John's, NL, Canada; Yasir Jassam, MD, MRCP, National Institute of Neurological Disorders and Stroke, Bethesda, MD, USA; Demetrio Konstas, MD, University of South Florida, Tampa, FL, USA; Marisa McGinley, DO, Loyola University Medical Center, Maywood, IL, USA; NikHaliza NikHassan, University of Minnesota, Minneapolis, MN, USA; Maryam Nabavi Nouri, MD, Hospital for Sick Kids, Toronto, ON, Canada; Viviana Ivonne Orozco-Leon, MD, University of Puerto Rico, San Juan, PR, USA; Veronica Penyak, MD, Northwestern McGaw Medical Center, Chicago, IL, USA; Fahed Saada, MD, University of Florida, Jacksonville, FL, USA; Meagan Seay, DO, Cleveland Clinic, Cleveland, OH, USA; Luka Vlahovic, MD, Loyola University Medical Center, Maywood, IL, USA; Vitaliy Zhivotenko, DO, Penn State Hershey Medical Center, Hershey, PA, USA.
Financial Disclosures: Dr. DeLuca is supported by the National Institute for Health Research Biomedical Research Centre and has received travel expenses from Biogen, Genzyme, Merck Serono, and Novartis. Ms. Halper has served as an unpaid consultant for Biogen in a research activity. Dr. Newsomehas participated in scientific advisory boards for Biogen, Novartis, and Genzyme and received research support from Biogen and Novartis. Dr. Ford has received honoraria as a consultant for advisory activities from Teva, Biogen, Genzyme, and EMD Serono and grant support from these companies as well as Genentech, MedImmune, Merck Serono, Novartis, Roche, and Sanofi Aventis. Drs. Buckle, Cortese, Graves, and Sicotte have no relevant financial disclosures.
Funding/Support: Funding for the Mentorship Forum and subsequent resources under development is provided through a medical education grant from Biogen through the FCMSC. Initiatives and ongoing activities (Web-based resources, directory of training programs/fellowships, CMSC SIG, and LISTSERV communication) under this grant are part of the FCMSC's ongoing MS Workforce of the Future development program.







