Publication
Research Article
International Journal of MS Care
Barriers and Facilitators Related to Participation in Aquafitness Programs for People with Multiple Sclerosis
Exercise and leisure activities provide physical and psychosocial benefits to people with multiple sclerosis (MS) and can enhance their quality of life. In Winnipeg, Manitoba, Canada, people with MS have reported barriers to their participation in local MS-specific aquafitness (AF) programs. Therefore, a formal exploration of the accessibility of local AF programs for people with MS was undertaken. The purpose of this phenomenological study was to identify factors that facilitate or impede participation in AF programs by individuals with MS living in Winnipeg. Qualitative data were collected from a total of eight participants through one focus group (n = 7) and one in-depth interview (n = 1). The sample consisted of individuals with MS who were currently participating in AF programming as well as those who were not. Data were audio-recorded and transcribed verbatim, and thematic analysis was completed. Seven themes emerged regarding factors affecting participation in local AF programs. Barriers to participation included inadequate transportation, lack of one-on-one support, environmental inaccessibility, and fears associated with participation in the programs. Facilitators of participation included a knowledgeable instructor and experiencing physical and psychosocial benefits from the program. Information from this study was used locally to advocate for people with MS in order to increase participation in local AF programming.
Aquafitness (AF) programs provide a variety of physical and psychosocial benefits to people with multiple sclerosis (MS).1–3 Aquafitness programs consist of exercises performed in water, and are sometimes classified as aquatic therapy.4 In Winnipeg, Manitoba, Canada, AF programs tailored to people with MS are offered through the City of Winnipeg. Although this specialized program has been offered regularly for over 10 years, class sizes have remained small, and anecdotal reports from people with MS have indicated difficulty attending the programs. In order to validate the reports of people with MS in this community and further understand the difficulties associated with participation in these programs, a formal exploration of the accessibility of local AF programs was undertaken.
Benefits of AF Programs for People with MS
Many advantages of water-based exercise have been identified for individuals with MS. Literature suggests that it can lead to reduced muscle stress, decreased pain, less guarded movement associated with the fear of falling, and improved performance in physical activity due to the properties of water.5 6 The water supports the body through its density and buoyancy, allowing the individual with MS to move more easily.4 7 Aquatic exercise also limits exercise-induced increases in body temperature, a factor associated with worsening MS-related fatigue symptoms.6 7
Many physical benefits are associated with AF programs for people with MS, including increased strength, endurance, flexibility, energy levels, cardiorespiratory function, balance, coordination, muscle tone, and postural control.3 4 8 Aquafitness classes have also been associated with improved performance in functional activities such as walking, climbing stairs, carrying essential items, getting up from a chair, dressing, and bathing.7 9 10 Psychosocial benefits of AF programs include increased social interaction and support, the development of friendships, a sense of acceptance from others with MS, decreased anxiety, and improved affect.5 11 12 These benefits may increase the participant's enjoyment, self-confidence, and feelings of achievement.2 4
Barriers and Facilitators Related to Participation
Rimmer and colleagues13 have proposed that a multifactorial array of barriers and facilitators act in conjunction to influence an individual's participation in physical activity. Barriers and facilitators can be factors inherent within the individual (including symptoms of MS and psychological factors), factors in the physical and social environments, or factors related to the occupation itself.14–16 Literature indicates that people with MS encounter an array of barriers to participation in leisure and physical activity in general,12 17 18 while there is less information specific to people with MS and AF programs. A meta-analysis found that MS patients' levels of physical activity are lower than those of the general population19; however, people with MS report that finding ways to incorporate physical activity into their lives is important.20 For people with MS, barriers to physical activity include the built environment, access to adaptive and exercise equipment, access to information about programs, fatigue, emotional and psychological factors, economic factors, knowledge and training of people working with those with disabilities, people's attitudes and perceptions about individuals with disabilities, facility and city-level policies and procedures, and transportation.13 14 21
Because the benefits of physical activity for people with MS are well documented but participation rates among this population remain low, more investigation into how to promote participation in leisure activities by people with MS is needed.13 14 This article describes the findings of a qualitative pilot study on the barriers and facilitators influencing participation in AF programs among people with MS in Winnipeg, Manitoba. This site-specific research was conducted in order to fully understand regional barriers to participation in AF programs and to identify ways to promote participation locally.
Study Design and Methods
This study was based on the principles of phenomenology, a qualitative research approach that is appropriate when the researcher wants to comprehend the common lived experiences of several people engaged in a phenomenon.22 The phenomenon explored, using focus group methodology,23 was the experience of people with MS in participating in AF programs in Winnipeg, Manitoba. The research questions were as follows: 1) What barriers do people with MS face to participating in AF programs in Winnipeg? 2) What facilitators help people with MS to participate in AF programs in Winnipeg?
Theoretical Framework
The Person-Environment-Occupation (PEO) model24 was adopted to consider participation in AF programs by people with MS. The PEO model considers the success of participation in any occupation or activity as the outcome of the interactions among three spheres: 1) person, 2) environment, and 3) occupation. Improving the congruency of these three spheres is posited to result in improved participation. In this study, the “person” is defined as the person accessing or attempting to access AF programs, the “environment” includes the pool environment and the city environment as the person accesses or attempts to access the program, and the “occupation” is the AF programs themselves.
Participant Recruitment
Ethical approval for the study was obtained from the Human Research Ethics Board of the University of Manitoba, and institutional approval was obtained from institutions that assisted with recruitment of participants. All participants provided informed written consent.
Participants were recruited over a 2-month period in the spring of 2010 in Winnipeg. Recruitment sites were the local chapter of the MS Society, the Health Sciences Centre Multiple Sclerosis Clinic, and two City of Winnipeg aquatic centers. Recruitment strategies included informational brochures, leaflets, and provision of information to visiting chapter members by the local MS chapter.
Each interested individual was contacted via telephone to screen for eligibility, with the exception of one participant who was screened via e-mail. Inclusion criteria were 1) age of 18 years or older; 2) self-reported diagnosis of MS; 3) the ability to contribute verbally in a focus group; 4) prior awareness of AF programming in the City of Winnipeg regardless of current participation status; and 5) fluency in English.
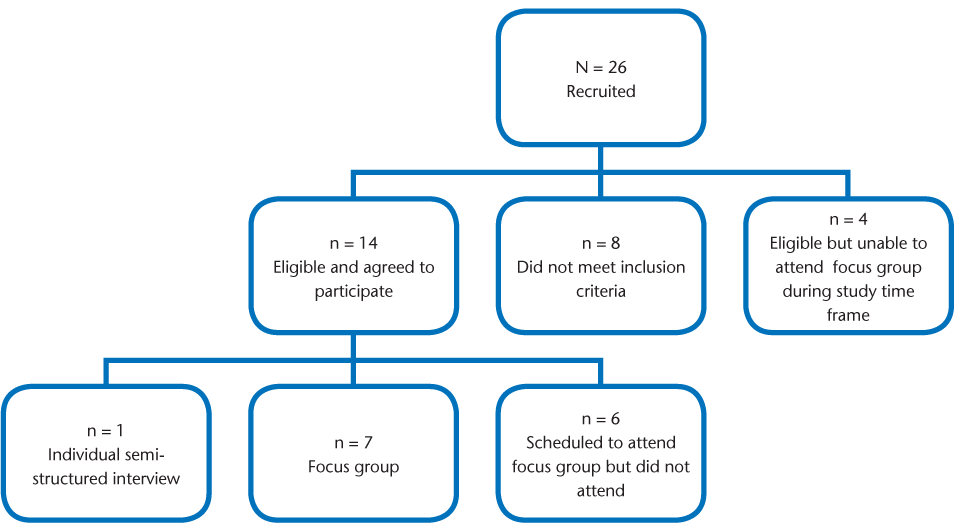
A total of 26 individuals were recruited (Figure 1), 25 via the above-mentioned recruitment strategies and 1 via snowball sampling. Eight participants did not meet the inclusion criteria, and 14 agreed to participate in the focus group discussions. Four people were eligible but were unable to attend the focus groups within the study timeframe. Of the 14 people who agreed to attend the focus groups, only 8 attended. Two of the six nonattenders contacted the researchers and cited a) lack of child care and b) lack of transportation as reasons for nonattendance at the focus group, while it is unknown why the other four expected participants did not attend. Although two focus groups were planned, only one participant attended the first scheduled focus group. Therefore, data collection was based on one semi-structured individual interview and one focus group.
Sample recruitment process
Data Collection
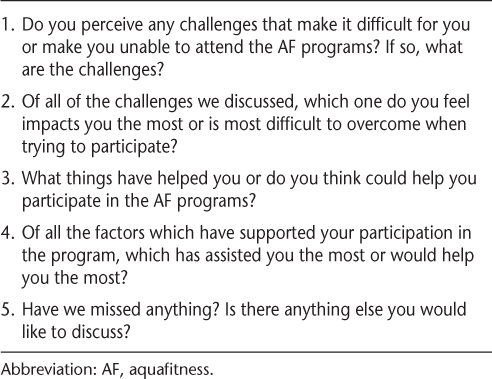
Each participant completed a demographic questionnaire prior to the focus group discussion that asked the participant's age, sex, year diagnosed with MS, and type of MS, as well as current or past involvement in AF programs. A semi-structured question guide was developed for the focus group (65 minutes' duration) and was adapted for the individual interview (40 minutes' duration) (Table 1). The individual interview and focus group were held at the MS Society of Canada, Manitoba Division, which was environmentally accessible and familiar to the participants.
Focus group questions
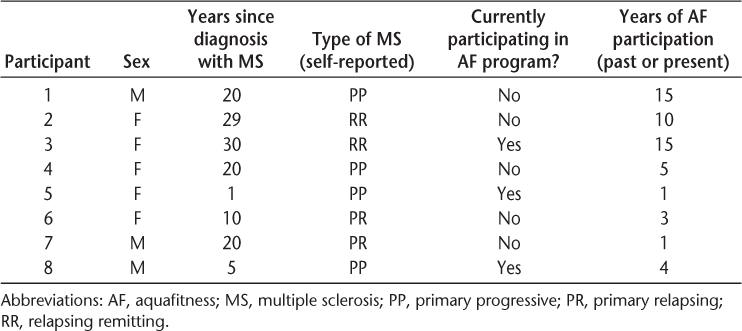
Sample
Five females and three males between the ages of 47 and 66 years participated (Table 2). Participants had been diagnosed with MS from 1 to 30 years previously. Diagnoses cited included primary progressive (n = 4), progressive relapsing (n = 2), and relapsing remitting (n = 2). Three of the participants were currently involved in AF programming, while the other five had participated in the past. Duration of participation in the AF programming ranged from 1 to 15 years.
Study participant characteristics
Data Analysis
Data were audio-recorded, transcribed verbatim, and then analyzed by the researchers. Data were transcribed using Microsoft Word (version 2007; Microsoft Corp, Redmond, WA) for thematic analysis. The second and third authors read and re-read the data to develop an initial coding scheme using the PEO model to inform the analysis.24 One of these authors completed the initial coding scheme for the interview, while the other completed the initial coding scheme for the focus group. The second and third authors then reviewed the coding from both the interview and the focus group to identify common experiences or recurring ideas among participants. Similar factors were identified in both the individual interview and the focus group, and common experiences among participants guided the formation of themes from the original coding schemes. Transcripts were then exchanged between the second and third author to increase familiarity with both the individual interview and focus group data. Finally, all authors discussed the results, which led to multiple revisions of the initial themes.
To ensure rigor in data collection and analysis, the second and third authors discussed preconceived notions before the interview and focus group, analyzed all data, and compared results. In addition, the first author provided feedback on thematic development, and different analytical frameworks were applied to the data to confirm that the PEO model accurately reflected the data.25
Results
Seven main themes emerged from the data that reflect the factors influencing participation in AF programs.
Theme 1: The Benefits of AF Encourage Continued Participation
All participants reported that AF programs had a positive effect on their physical and social well-being. Some individuals perceived the physical benefits to be the primary motivator to participation, with the social benefits being an “added plus,” while others held the opposite view.
Physical Effects
Physical benefits reported by the participants included maintaining and improving health, maintaining muscle tone, improving flexibility, enhancing quality of movement, and increasing activity level. Knowing that they will feel good after the class helped motivate participants to attend: “It makes you feel good, you miss it if you don't go. . . . Your body lets you know, like especially if you haven't been at it for a while. You don't have the same activity level. So it's keeping your activity level up and your strength. . . . If you stay away for a long time you lose it totally. . . . You've heard that saying, ‘If you don't use it, you're gonna lose it’—well, it's a fact. You start to lose it, but if you keep it up you're in good spirits and you're in good health and you're stronger.”
Exacerbation of fatigue was the only reported negative physical effect of AF classes. Participants discussed the importance of monitoring their fatigue levels while in the pool so that they could continue to enjoy the program. A certain degree of fatigue was noted to be positive, with participants viewing it as an indicator of having exercised and “used their muscles,” while high levels of fatigue had a negative impact on participation. One participant explained, “You can push yourself too hard and then you don't want to go back. It's not fun anymore.”
Psychosocial Effects
Socialization was a motivating factor to attend AF classes. As one participant stated, “The association with other people, with my peers . . . I found encouraging.” Another participant said, “Exercise is good, but to me the people keep it positive and get you out there and doing it.” Participants also emphasized the positive social interactions that occur after class as participants enjoy going for lunch or coffee together.
Feelings of acceptance, despite disability, were also reported to be a motivating factor in AF class attendance, as class participants felt understood and accepted by others. One participant described this experience of universality by saying, “Everyone has something in common with everybody else in the group. So that even if you didn't really like the person, you can relate very well on certain levels.” Another participant remarked, “If you come in with a walker or a scooter, once you get in the water it doesn't matter, you're all the same.” Participants felt that the pool environment allowed them to relate to one another as “normal people.”
Aquafitness was seen to be an activity in which all participants can experience feelings of accomplishment. One participant shared, “It's a wonderful thing to be able to know that there's something out there that you can do,” with another reiterating, “You can't do all the sports, and if you're a sports nut or growing up that way, and all of a sudden you can't do it, then it's kinda nice [to be able to do something].”
Theme 2: The Environment Must Be Accessible and Tailored to the Needs of Those with MS
Participants emphasized the importance of an accessible environment for participation in AF programs. Participants hailed from two different AF sites, both of which met standard accessibility requirements. However, participants still described accessibility challenges at both pools such as small, cramped changing-room facilities. “Like, one of us has to sit on the toilet and the other one has to sit in the shower, and then you have two other seats.” The size and layout of the changing rooms were particularly challenging for participants who used walkers, scooters, or wheelchairs, with one participant who used a scooter describing the process of navigating the changing room entrance as follows: “And you run into something like an L-shape where you gotta go through a door and then you make a left-hand turn right away, and then you gotta make a right-hand turn. . . . You'd find a scooter does not exactly zig-zag. So you end up, you're trying to maneuver or you get stuck on the walls.” The participants felt that changing rooms with “loads of room” would be advantageous.
The proximity of the changing room to the pool's edge was also considered an important environmental feature, especially as the physical symptoms of MS became more severe: “For me, the men's change room is further away. It's not a big deal now, but I can see it becoming a big deal, you know, if you weren't able to walk that far.”
Participants cited pool equipment such as pool “noodles,” floating boards, webbed mitts, and Styrofoam weights as an environmental facilitator. The equipment was viewed as important both for flotation for weaker swimmers and for “get[ting] your heart rate up.” Two main methods of pool entry were discussed by participants: stepladders and stairs. “Steps with rails that you can hang onto” were preferred, since, as one participant explained, “Well, if you're compromised with your legs and your arms, climbing a ladder is not the best thing to try.” Participants also noted the importance of mechanical lifts for assisting individuals who were not able to otherwise access the pool. Although stairs were considered the most accessible method of getting into and out of the pool, stairs elsewhere in the environment (such as leading into the building and within the facility) were seen as obstacles.
Water temperature was a frequently discussed feature of the environment, with participants noting that “everyone is different” regarding individual preferences about water temperature. One participant stated that the cold water caused her legs to “cramp up . . . seize up.” However, warmer water was also recognized as a challenge for other participants who were heat-sensitive.
Theme 3: The Ability to Get To and From the Pool Influences Participation
The participants reported using a variety of means to get to and from the program, including driving themselves, getting a ride from a fellow participant or family member, taking a taxi, and using Handi-Transit (a subsidized accessible-transportation program for people with disabilities). Participants agreed that driving oneself to and from the program was easiest, but noted that many individuals have lost their driver's license as a result of MS-related physical and/or cognitive impairments. Participants viewed limited accessible parking as a barrier to accessing the pool facilities, and it was agreed that more accessible parking spots were warranted.
Lack of flexible and accessible transportation was a barrier for some participants. Although many individuals participating in the AF programs relied on Handi-Transit for transportation to and from the program, several barriers to using the service were identified. It was noted that people with cognitive and mobility problems may find it difficult to be ready exactly at their pick-up time, especially when experiencing fatigue after the AF class. A second barrier was that pick-up and drop-off times often required participants to be at the pool well in advance of the class or to stay late after the class to wait for their ride. Finally, participants reported that the use of Handi-Transit limited their ability to engage in spontaneous social meetings following the class, as pick-up times are pre-booked and generally inflexible. One Handi-Transit user explained that the extra steps and planning needed to use the service discouraged class attendance: “It's gotten so hard to get anywhere and now I don't drive, which means I have to take Handi-Transit. . . . I'm glad they have it, but any excuse not to go.”
Theme 4: Pool Staff Attitudes and Knowledge Are Important for Facilitating AF Participation
Helpful and friendly pool staff, attentive lifeguards, and an effective AF instructor were all considered important for facilitating AF participation. Participants emphasized the importance of a motivating AF instructor. Participants spoke very highly of their instructors: “We've got a real good instructor there, she's been with us for a long time”; “She's great, we love her.” Participants identified several characteristics they considered central to an instructor's effectiveness, including “experienced,” “knowledgeable and personable,” “likeable,” “relate well to everybody,” attentive, “blend in with the group,” “good communication,” good teaching skills, and taking courses to update and improve the program. While describing the importance of a good communication style, one participant said “she talks to us like we're, like we're normal . . . and we don't have a disability.”
Participants recognized that the diverse needs and abilities of the individuals in the AF programs require the instructors to adjust the classes accordingly. While acknowledging that this task could be challenging, they considered this skill to be central to an instructor's success. One participant said, “All of us are different, we all move different ways, you know, and she just, she knows how to deal with all of us.” Another participant noted, “They [the instructors] have to monitor each person . . . and they can't push the group beyond their means. . . . There's certain limitations [of group participants] and they have to adjust themselves to that.” Participants recognized the difficulty of finding and keeping a good instructor: when they “get a good one, you try and keep her.”
Theme 5: Lack of One-on-One Support May Restrict Participation in AF Programs
The participants wished that more people with MS could participate in AF programs, particularly those with more severe disability. Participants reported that the programs exclude people who require one-on-one support because there is only one instructor. One participant explained that a friend was unable to attend the AF programs because “she doesn't have anybody to go with her. . . . There's a big segment of people that are shut out of the program.” Participants felt that greater supervision in the water was needed for people with more mobility limitations. They suggested numerous ways in which one-on-one support could enable participation, including helping people into and out of the water, walking beside them, and helping them get dressed after the class. However, participants also acknowledged barriers to finding a personal attendant to bring to the AF classes: “Even to hire somebody, you wanna work for 1 hour? No, you're gonna get a job. . . . It's very hard to find somebody to fit into that niche.” Even if a personal attendant could be found, participants thought that finances would be a barrier, since many people with MS are “on disability [benefits]—fixed incomes” and do not have “a lot of money . . . to throw around.” This disparity in ability to participate in the AF programs based on level of disability—coupled with the expense of having to obtain a private aide—was considered unfair: “Money should not be the reason that you can't participate.”
Theme 6: Enhanced Visibility of AF Programs Is Needed
Enhanced Visibility of the AF Program Itself
Most participants learned about the AF classes through the local leisure guide or a citywide telephone service inquiry line. Finding information on the AF program was facilitated by membership in the local MS Society for some participants, while others sought information independently. One participant said, “When I came [to the MS Society] when I found out that I had MS—I'm not sure if everybody does that when they first find out—they come here and get an information package and . . . in there is information about yoga, swimming, and everything else that they offer and then I went . . . and found out about the pool because those details are through the City of Winnipeg, not specifically in the MS guide.”Although this individual demonstrated initiative in seeking out information about the AF programs, participants noted that others might not have the same level of resourcefulness. Many participants received initial information about AF through the MS Society, but participants saw the need for additional marketing strategies to reach people who may not be members of the society.
Word-of-mouth communication was cited as an effective strategy for raising awareness of AF programs: “The only way you can tell people is to tell people about it and hope they talk to someone else.” Participants expressed that “we need to spread the word that [AF is] very beneficial for people with MS.” The group also felt that “somehow we need to get the message out to the men who have MS” and that there is a need to “get the message out to men, period,” since men are underrepresented in the AF classes.
Participants brainstormed alternative marketing strategies to increase awareness of local AF programs in the MS community. Increased direction to local resources upon receiving the diagnosis of MS was thought to be advantageous, but too much information upon initial diagnosis was viewed to be overwhelming. Participants also suggested displaying a pamphlet produced by the AF program at clinics and the MS Society. Some felt that increased public attention and media advertising of MS programming may help reach the larger community of individuals with MS. Other participants suggested partnership with a “radio personality” or “somebody important” to raise awareness of MS programming.
Increased Visibility of Information Regarding Financial Subsidies
An additional barrier related to accessing the AF program is the cost of the enrollment fee, which at the time of the study was $58.60 (CAD) for a 10-week session. “I know that there's some people in our group . . . that really can't afford it, and there should be something out there offered to them.” Although participants thought that there might be subsidies available for the AF programming, they were not aware of specific details, or how to access them. Participants remarked that information regarding government funding is often not well publicized to citizens, with one participant stating, “you aren't made aware of it, you have to go find it.” The group concluded that “there should be easier access to [information about financial assistance].”
Theme 7: Participating in AF Programming Requires Negotiating Fears
Overcoming Feelings of Fear, Shock, and Denial Upon Diagnosis with MS
Participants discussed the challenges they faced when they were first diagnosed with MS, stating that it was “hard to accept” and reporting feelings of denial, shock, and fear. Acceptance of the diagnosis took time—in some cases years—and some participants' denial prevented them from joining MS-specific programs such as AF. One individual expressed her fear this way: “I was just floored, I didn't know anything about this, nothing at all, and I was scared.” Another participant stated, “Well I was shocked, right? What are you talking about I have MS, right?” and yet another elaborated: “I kept denying it, I don't have it, I don't have it.” Participants said they had to overcome their fear, shock, and denial of the diagnosis itself before considering joining MS-specific programs.
Apprehension About What to Expect
Even once participants had processed the diagnosis of MS, they still needed to overcome additional fears about what to expect from the AF program before enrolling in it. One participant recalled, “I was actually afraid to go at first. I didn't know what to expect.” In addition to anxiety about the program itself, participants expressed initial concerns about not knowing anyone else in the program and whether they would make friends with other participants.
Anxiety About Prognosis of MS
Participants also recounted feeling anxious about seeing other AF program participants who might have higher levels of disability. As one participant said, “All I could think of was ‘I am going to get like that?’” The experience of interacting with people with varying degrees of disability took time to accept and adjust to. One participant explained that seeing other participants with mobility limitations caused her to wonder about the future course of her disease: “I think it's only human that it would go through your mind when you see other people with [MS] . . . that don't have their mobility and are far worse than you . . . do I want to see people in wheelchairs and walkers but you're not like that yet and so you think . . . is that what I'm going to be like? It's just a whole accepting process.” As participants in the focus group expressed these thoughts, other group members seemed relieved to learn that they were not the only ones to feel this way. Participants reported that despite their fears of the future, they were encouraged by seeing how others with more advanced MS were able to manage at AF classes.
Feeling Safe While in the Water
Once in the pool, participants often experienced a fear of drowning. The perception of whether or not a lifeguard was being attentive was important to feeling safe in the water. One participant noted, “I have no concerns about that because I have seen them jump in to get somebody out.” The lifeguards provided “peace of mind,” a feeling of safety that was needed even though it was recognized that “9 out of 10 times, nothing will happen.”
Discussion
Consistent with the theoretical basis of this study, the seven themes that emerged from the data reflect characteristics of the person, features of the environment, and factors of the occupation, as well as interactions of these three spheres that influence AF program participation. While many of the study findings were consistent with previous studies, others represent new insights. The findings from this study are discussed using the PEO framework.24
Person
The PEO model asserts that an individual's affective, physical, and cognitive attributes influence participation. In this study, the affective component, identified as a person's fears and anxieties, constituted a barrier to participation. Fear of the unknown and concerns about one's safety within a fitness facility have been documented previously.13 14 16 However, the participants in this study reported broader and more diverse anxieties influencing AF participation by people with MS than previously reported. Specifically, difficulties with acceptance of the diagnosis and the progressive nature of MS impeded participation in MS-specific programming. Since participants in this study were reassured when they learned that the other participants shared the same fears, increased attention to validating common fears upon initial diagnosis may help people with MS take steps to participate in disease-specific programming.
Environment
The environment encompasses both the physical and social contexts in which the AF programs take place.24 This study reinforces previous reports that the physical environment such as small changing rooms and narrow aisles can act to enable or restrict participation.16 26 A new finding in this study was the identification of stairs with a railing as a preferred pool entry method rather than a traditional stepladder.
Previous literature has suggested that cooler water is advantageous for people with MS, as it helps to limit elevation of body temperature—a factor thought to exacerbate the neurologic symptoms of MS.4 6 11 In contrast, this study found that water temperature preference varies from person to person, indicating that AF classes should be offered in more than one location in pools with varying temperatures.
Another finding consistent with previous literature is the influence of transportation on participation.11 21 Survey research has indicated that accessible transportation is a main facilitator of participation in physical activity programs for people with MS, while a lack of transportation is a main barrier to participation.13 26 Froehlich and colleagues27 found inadequate transportation to be the main barrier to physical activity participation and transportation costs to be the fourth-ranked barrier. In addition, their study highlighted the inflexibility of subsidized transit systems and the difficulty in obtaining rides at the time they are needed, paralleling the findings of this study.
A surprising finding in this study was the importance participants placed on the role of the instructor in promoting a positive experience during AF sessions. Although the value of a knowledgeable instructor who understands how to adapt activities for people with disabilities has been previously recognized,13 17 the present study highlights the great influence of this factor on people's continued participation in the program. Moreover, while other studies have identified instructors' lack of assistance, lack of knowledge about MS, and lack of training in disease-specific AF programs as barriers to participation of people with MS,13 16 21 the participants in this study identified strong interpersonal skills as a central feature of AF instructor effectiveness.
Another theme that was consistent with the literature was the need for increased one-on-one support for AF program participants.13 16 Because individual support may be a key factor limiting participation in these activities, creative solutions need to be devised to provide one-on-one support both during and after the AF class.
This study also highlights the need for increased awareness of AF programs, as well as increased publicity about financial subsidies available. Several individuals who initially contacted the researchers for further information on the study had never heard of the AF program before seeing the recruitment posters. This is consistent with previous research suggesting that individuals with disabilities often feel that they should be provided with more information regarding suitable leisure and fitness pursuits, and that when they seek out such information themselves, it should be easier to obtain.13 14 While some individuals are self-directed in seeking information about disease-specific programs, others require more deliberate marketing strategies, and people with MS who are not members of the MS Society may miss information about AF programs. Previous research suggests that provision of information may increase participation in physical and recreational activities by those with MS.16 17
Occupation
The PEO model considers occupations to be everything a person needs or wants to do, including leisure, productivity, and self-care activities.24 Participants in this study regarded AF programs as a valuable occupation, as it contributed to both their self-perceived physical and psychosocial health. However, the benefits needed to outweigh the barriers associated with participating in the AF programs. The physical and social benefits reported are those previously identified in the literature2 5 8 10 11; in particular, it is notable that the perceived universality among group members echoes the finding of Elsworth and colleagues,16 and suggests that individuals with MS prefer to exercise with others with a disability.
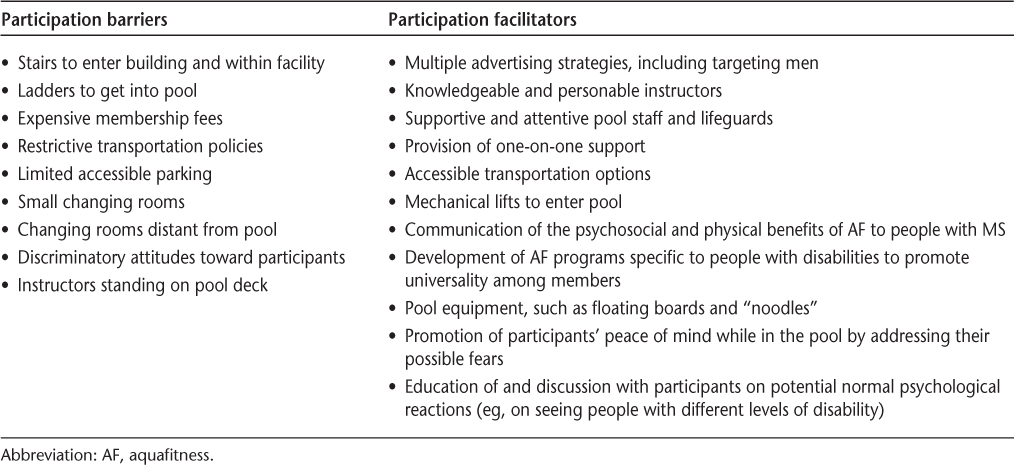
Information on the barriers and facilitators related to AF programming can be useful to AF instructors, MS clinicians, and recreational facility program planners. Table 3 provides a summary of these barriers and facilitators and can serve as a checklist for service providers and program planners who are initiating new aquatics programs or reviewing current programming.
Considerations for service providers and planners of AF programs
One limitation of this study was the small sample size and rate of attrition. Because this was a time-limited student project, it was not possible to continue with sampling, and therefore data collection did not reach saturation. In addition, people with a level of cognition or communication that would not allow them to participate fully in a focus group, people who had never participated in AF classes, and caregivers were not included in this study. These excluded groups, which may have represented the MS population with a higher level of disability, may have experienced different barriers to participation in the AF programs. Finally, member-checking could have further strengthened the trustworthiness of the results.
Future research should investigate the experiences of individuals with a broader range of disability levels and their caregivers. PhotoVoice research28 may help provide further insight into how people with MS navigate barriers and facilitators related to participation in physical and recreational programming. Survey methodology may also improve understanding of this topic over a larger geographic region. The concept of gender and its impact on the decision to participate in AF programs emerged during this study and is an interesting possible avenue for future research.
This project was a small-scale study of local experience that was effective in informing local advocacy groups about local issues. The results of this study resulted in improved communication with the local accessible public transportation system on the prioritization of AF programs for transportation, enhancements in aquatics marketing by the local chapter of the MS Society, and re-energized advocacy efforts for improving accessibility of leisure programs in the City of Winnipeg.
Conclusion
People with MS report many benefits as well as barriers related to AF programs. In order for an individual to participate in AF programming, the personal benefits must outweigh the personal barriers. Participants in AF programs have many simple suggestions and solutions for improving access to AF programs for people with MS.
PracticePoints
Aquafitness (AF) programs have diverse physical, social, and psychological benefits for people with MS.
People with MS encounter various barriers to participation in AF programs, including lack of transportation, need for one-on-one support, inaccessible pool environments, and fitness professionals' lack of knowledge about MS.
As fear can prevent MS patients from initiating participation in AF programs, support from clinicians is needed to help patients begin and continue these programs.
Acknowledgments
The MS Society of Canada, Manitoba Division, provided assistance with participant recruitment. In particular, we would like to acknowledge Ellen Karr, Client Services Coordinator, for her advice regarding study design and assistance with recruitment.
References
Broach E, Groff D, Dattilo J, Yaffe R, Gast D. Effects of aquatic therapy on adults with multiple sclerosis. Ann Ther Recreation. 1998; 7: 1–18.
Broach E, Dattilo J, McKenney A. Effects of aquatic therapy on perceived fun or enjoyment experiences of participants with multiple sclerosis. Ther Recreation J. 2007; 41: 179–200.
Gehlsen GM, Grigsby SA, Winant DM. Effects of an aquatic therapy program on the muscular strength and endurance of patients with multiple sclerosis. Phys Ther. 1984; 64: 653–657.
Veenstra J, Brasile F, Stewart M. Perceived benefits of aquatic therapy for multiple sclerosis participants. Am J Recreation Ther. 2003; 2: 33–48.
Broach E, Dattilo J. Effects of aquatic therapy on adults with multiple sclerosis. Ther Recreation J. 2001; 35: 141–154.
Vargas L. Aquatic Therapy: Interventions and Applications. Ravensdale, WA: Idyll Arbor Inc; 2004.
Pariser G, Madras D, Weiss E. Outcomes of an aquatic exercise program including aerobic capacity, lactate threshold, and fatigue in two individuals with multiple sclerosis. J Neurol Phys Ther. 2006; 30: 82–90.
Broach E, Dattilo J. The effect of aquatic therapy on strength of adults with multiple sclerosis. Ther Recreation J. 2003; 37: 224–239.
Motl RW, McAuley E. Longitudinal analysis of physical activity and symptoms as predictors of change in functional limitations and disability in multiple sclerosis. Rehabil Psychol. 2009; 54: 204–210.
Woods D. Aquatic exercise programs for patients with multiple sclerosis. Clin Kinesiol. 1992; 46: 14–20.
Roehrs TG, Karst GM. Effects of an aquatic therapy exercise program on quality of life measures for individuals with progressive multiple sclerosis. J Neurol Phys Ther. 2004; 28: 63–71.
Finlayson M, Impey MW, Nicolle C, Edwards J. Self-care, productivity and leisure limitations of people with multiple sclerosis in Manitoba. Can J Occup Ther. 1998; 65: 299–308.
Rimmer JH, Riley B, Wang E, Rauworth A, Jurkowski J. Physical activity participation among persons with disabilities: barriers and facilitators. Am J Prev Med. 2004; 26: 419–425.
Becker H, Stuifbergen AK. What makes it so hard? barriers to health promotion experienced by people with multiple sclerosis and polio. Fam Community Health. 2004; 27: 75–85.
Borkoles E, Nicholls AR, Bell K, Butterly R, Polman R. The lived experiences of people diagnosed with multiple sclerosis in relation to exercise. Psychol Health. 2008; 23: 427–441.
Elsworth C, Dawes H, Sackley C, et al. A study of perceived facilitators to physical activity in neurological conditions . . . including commentary by Cup E, Pieterse A, Block P. Int J Ther Rehabil. 2009; 16: 17–24.
Stuifbergen A, Rogers S. Health promotion: an essential component of rehabilitation for persons with chronic disabling conditions. Recov Rehabil. 1997; 19: 1–20.
Yorkston KM, Johnson KL, Klasner ER. Taking part in life: enhancing participation in multiple sclerosis. Phys Med Rehabil Clin. 2005; 16: 583–594.
Motl RW, McAuley E, Snook EM. Physical activity and multiple sclerosis: a meta-analysis. Mult Scler. 2005; 11: 459–463.
O'Hara L, De Souza L, Ide L. A Delphi study of self-care in a community population of people with multiple sclerosis. Clin Rehabil. 2000; 1: 62–71.
Vanner E, Block P, Christodoulou C, Horowitz B, Krupp L. Pilot study exploring quality of life and barriers to leisure-time physical activity in persons with moderate to severe multiple sclerosis. Disabil Health J. 2008; 1: 58–65.
Creswell JW, Hanson WE, Clark Plano VL, Morales A. Qualitative research designs: selection and implementation. The Counseling Psychologist. 2007; 35: 236–264.
Kruger RA, Casey MA. Focus Groups: A Practical Guide for Applied Research. Thousand Oaks, CA: Sage Publications, Inc; 2009.
Strong S, Rigby P, Stewart D, Law M, Letts L, Cooper B. Application of the Person-Environment-Occupation model: a practical tool. Can J Occup Ther. 1999; 66: 122–133.
Bradbury-Jones C. Enhancing rigour in qualitative health research: exploring subjectivity through Peshkin's I's. J Adv Nurs. 2007; 59: 290–298.
Meyers A, Anderson J, Miller D, Shipp K, Hoenig H. Barriers, facilitators, and access for wheelchair users: substantive and methodologic lessons from a pilot study of environmental effects. Soc Sci Med. 2002; 55: 1435–1446.
Froehlich A, Nary D, White GW. Identifying barriers to participation in physical activity for women with disabilities. SCI Psychosocial Process. 2002; 15: 21–28.
Newman S, SCI PhotoVoice participants. Evidence-based advocacy: using PhotoVoice to identify barriers and facilitators to community participation after spinal cord injury. Rehabil Nurs. 2010; 35: 47–59.
Financial Disclosures: The authors have no conflicts of interest to disclose.







