Publication
Research Article
International Journal of MS Care
Associations Between Bladder Dysfunction and Falls in People with Relapsing-Remitting Multiple Sclerosis
Author(s):
Background:
Bladder dysfunction and falls are common in people with multiple sclerosis (MS), but associations between these problems are unclear. We sought to clarify the association between specific types of bladder dysfunction and prospectively recorded falls in people with MS.
Methods:
Fifty-one people aged 18 to 50 years with relapsing-remitting MS and mild-to-moderate disability (Expanded Disability Status Scale score ≤6.0) completed a self-report questionnaire regarding urinary incontinence, urgency, and frequency at baseline and then prospectively recorded their falls daily for 3 months using fall calendars. Participants were classified as recurrent fallers (two or more falls) or nonrecurrent fallers (fewer than 2 falls) for one regression model and then as fallers (one or more falls) or nonfallers (no falls) for another regression model. Associations between baseline bladder dysfunction and faller status were assessed using logistic regression adjusted for the potential confounders of age, sex, and disability.
Results:
Fifteen participants were recurrent fallers, 36 were nonrecurrent fallers, 32 were fallers, and 19 were nonfallers. After adjusting for age, sex, and disability, there was a significant association between urinary urgency with incontinence and recurrent falls in the 3 months after baseline (odds ratio, 57.57; 95% CI, 3.43–966.05; P = .005).
Conclusions:
Urinary urgency with incontinence is associated with recurrent falls in people with relapsing-remitting MS with mild-to-moderate disability. Further research is needed to better understand the mechanisms underlying this association and to evaluate the effect of bladder management programs on falls.
Falls are common in people with multiple sclerosis (MS), with many studies demonstrating more than 50% of people with MS falling in a 3- to 6-month period.1 2 Falls are associated with loss of confidence in walking, reduced quality of life, injuries, and possibly death.2–4 Ascertaining the risk factors for falls in people with MS, particularly the reversible fall risk factors, is essential for identifying those needing fall prevention interventions and for optimizing the content of these interventions. Bladder dysfunction is also common in MS.5 Demyelination of the complex neural circuitry responsible for urine storage and release, via urinary sphincter and bladder detrusor muscle contraction and relaxation, can cause a range of bladder symptoms, including urinary frequency, urgency, and incontinence.6–8 Bladder dysfunction is associated with falls in older adults.9–11 Bladder dysfunction may be associated with falls because it is a marker for other fall risk factors, such as declines in other physical or cognitive functions or overall frailty. It is also possible that bladder dysfunction directly contributes to falling, particularly with urgency and fear of incontinence making people move more quickly than is safe. Despite the high prevalence of bladder dysfunction and falls in people with MS, the known association between these problems in older adults, and a rationale for an association in people with MS, studies examining the association of bladder dysfunction with falls in people with MS are limited and have yielded conflicting results.2 12–16
Four studies found an association between retrospectively counted falls and urinary symptoms in people with MS. Finlayson et al.12 observed statistically significant associations between urinary incontinence and one or more falls occurring 6 months before baseline in a cohort of 1089 older adults with MS. Matsuda et al.14 found associations between urinary incontinence and one or more falls and between urinary incontinence and multiple falls occurring 6 months before baseline in a cohort of 474 patients with MS. In a study of 92 ambulatory adults with MS, Sung et al.15 reported that those with urinary bladder problems that they described as severe experienced more falls in the previous 3 months, independent of imbalance and walking speed. Sosnoff et al.16 reported that in 52 ambulatory adults with MS, the bladder/bowel subscale score of the Expanded Disability Status Scale (EDSS) was associated with falls in the previous 12 months. Although the results of these studies all suggest that bladder dysfunction, particularly incontinence, is associated with falls, they are limited by restricted assessment of bladder symptoms and by assessing falls retrospectively only. The present study attempted to overcome these limitations by assessing multiple aspects of bladder symptoms, including incontinence, urgency, and frequency, and by assessing falls prospectively, the current gold standard approach.
Of the two previously published studies evaluating the relationship between prospectively counted falls and urinary symptoms only one found a significant association. Gunn and colleagues13 found, in a cohort of 148 ambulatory (EDSS score of 3.5–6.5) people with MS aged 33 to 84 years, that those with regular or frequent urinary incontinence were at significantly greater odds of being a faller in the 3 months after baseline than were those with no or occasional urinary incontinence. However, Nilsagård and colleagues2 found no significant association between baseline urinary incontinence and falling in the 3 months after baseline in a cohort of 76 ambulatory (EDSS score of 3.5–6.0) people with MS aged 25 to 75 years. This discrepancy in findings could be because Gunn et al. defined a faller as someone who fell two or more times, whereas Nilsagård et al. defined a faller as someone who fell only once or more. Because people who have recurrent falls may have different characteristics than those who fall at least once,1 it is possible that there may be different associations between bladder dysfunction and falls in these two groups.
In addition to conflicting results, no study published to date has evaluated whether specific urinary symptoms are associated with future falls in people with MS. The purpose of the present study was to clarify the possible association between baseline urinary symptoms and future falls, including one or more falls and recurrent (two or more) falls and to identify whether specific urinary symptoms, including incontinence, urgency, and frequency, are associated with future falls in people with MS.
Methods
Participants
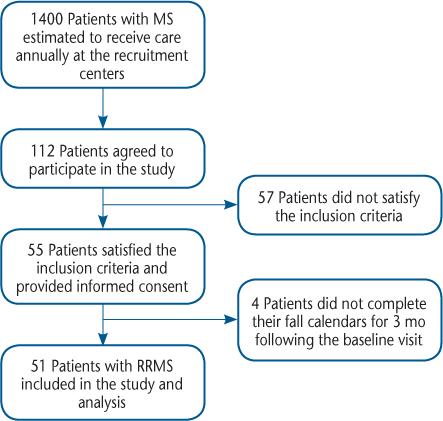
Participants were recruited to this longitudinal observational cohort study of fall risk factors in MS from outpatient MS clinics in the VA Portland Health Care System (VAPORHCS) and Oregon Health and Science University (OHSU) multiple sclerosis clinics and from the surrounding community using flyers, advertisements at educational programs, and referrals from clinicians, as previously reported.17 Of an estimated 1400 people with MS receiving care annually in these clinics, 112 agreed to participate in the study, and 55 provided informed consent and satisfied the criteria for this analysis. Of the eligible individuals, four were excluded from this analysis because they had incomplete fall calendars, resulting in 51 people with relapsing-remitting MS (RRMS) being included in this analysis (Figure 1). This study was approved by the VAPORHCS and OHSU institutional review boards. All participants provided written informed consent to participate.
Consort diagram for participant recruitment, participation, and analysis
The inclusion criteria for this analysis were a physician-confirmed diagnosis of MS18; RRMS subtype; mild-to-moderate disability due to MS (EDSS19 score ≤6.0); no relapse within 30 days of baseline; able to understand and consent in English; and complete data available. Age was limited to 18 to 50 years to minimize causes of falls other than MS. In addition, individuals were excluded if they had balance or gait affected by a condition other than MS, were not able to walk 100 m, could not comprehend English, or were blind.
Variables
Urinary Symptoms
At baseline, as part of their health history, participants were asked to respond “yes” or “no” to the following written question: “Do you currently have any of the following symptoms? Urinary incontinence? Urinary frequency? Urinary urgency?” Responses were collected for each symptom.
Falls
Participants were then asked to prospectively record their number of falls each day using fall calendars. The definition of a fall was clearly written at the top of each calendar page, as follows: “any unexpected event that results in ending up on the ground, floor, or any lower surface.”17 This definition is recommended for use in investigations, and the use of fall calendars to count falls is the current gold standard for fall detection in research because it helps minimize recall bias.20 21 Participants were asked to mail their fall calendars back to the investigative team in self-addressed envelopes at the end of each month. To reduce bias due to loss to follow-up, participants who did not turn in their calendars on time were telephoned within 1 week after the deadline to remind them to submit their calendars.
Based on the number of falls reported during 3 months of counting, participants were categorized as recurrent fallers if they fell two or more times or as nonrecurrent fallers if they fell once or not at all. Participants were also categorized as fallers if they experienced one fall or more and as nonfallers if they had no falls during 3 months of counting. This was done so that we could compare these findings with previously published results because previous studies have defined a faller as a person who has fallen two or more times or as a person who has fallen once or more.2 12 13
Potential Confounders
Age and sex were reported by participants at baseline. Disability due to MS was assessed using the EDSS performed by a physician or nurse practitioner.19 Age and sex were targeted as potential confounders because they have been found to be associated with bladder incontinence and falls in adults with and without MS.22–24 The EDSS score was targeted as a potential confounder because greater MS-associated disability may also affect bladder dysfunction7 and falls.23 25
Statistical Analyses
To assess for differences in characteristics between recurrent fallers and nonrecurrent fallers (and between fallers and nonfallers), mean age was compared between groups using two-sample t tests, and associations between the extent of disability as measured by the EDSS and faller status and between sex and faller status were assessed using Fisher exact and χ2 tests. Age was treated as a continuous variable and sex as a categorical variable. The EDSS score was treated as a continuous variable in adjusted analyses.
To assess the relationship between recurrent falls (or one and more falls) and urinary incontinence or urinary urgency, adjusting for age, sex, and disability (EDSS score), we divided the cohort into two groups: participants having urinary urgency without incontinence (represented by indicator variable 1) and those having urinary urgency with incontinence (represented by indicator variable 2). This was done because all the participants with urinary incontinence were found to have urinary urgency, although some participants had urinary urgency without incontinence.
Adjusted relationships between bladder dysfunction and faller status were assessed using multiple logistic regression, providing odds ratios (ORs) with 95% confidence intervals (CIs). For multiple logistic regression, we performed standard diagnostics to assess model integrity and evaluated the ability of the model to distinguish participants who experienced recurrent falls or one or more falls from those who did not by computing the area under the receiver operating characteristic curve. Where standard multiple logistic regression could not be implemented because of quasi-complete separation of data, we used Firth restricted logistic regression and estimated the goodness-of-fit of the regression models using McFadden's R 2.26 Finally, achieved power was determined for significant results, and sample size estimates were calculated for suggestive but nonsignificant results. Statistical computations were performed using Stata (version 13.1, StataCorp, College Station, TX), and the level of significance was set at P < .05. All computed P values were two-tailed.
Results
Participant Characteristics
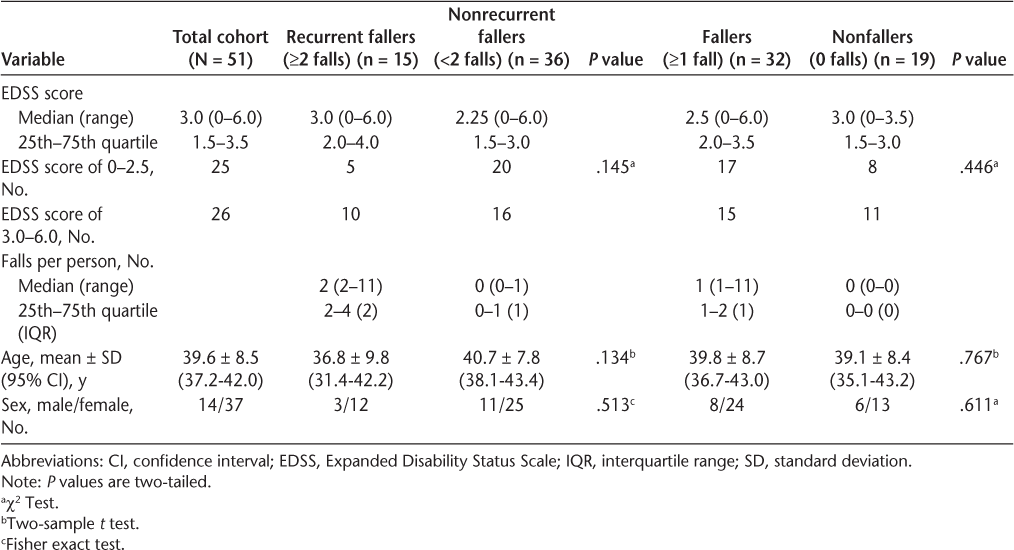
Of the 51 participants, 15 (29%) were recurrent fallers (3 men, 12 women; fall count range, 2–11) and 36 (71%) were nonrecurrent fallers (11 men, 25 women). On reclassification of the cohort, 32 (63%) were fallers (8 men, 24 women; fall count range, 1–11), and 19 (37%) were nonfallers (6 men, 13 women). No statistically significant differences were observed between recurrent and nonrecurrent fallers in EDSS scores (P = .145), mean age (P = .134), or sex (P = .513) or between fallers and nonfallers in EDSS scores (P = .446), age (P = .767), or sex (P = .611) (Table 1).
Characteristics of the 51 study participants according to fall status
Urinary dysfunction was more prevalent in fallers (any or recurrent) than in nonrecurrent fallers or nonfallers. Of the 15 recurrent fallers, two (13%) had urinary urgency without incontinence, seven (47%) had urinary urgency with incontinence, and seven (47%) had urinary frequency. Of the 36 nonrecurrent fallers, five (14%), one (3%), and six (17%) had urinary urgency without incontinence, urinary urgency with incontinence, and urinary frequency, respectively. Of the 32 fallers, five (16%), eight (25%), and 11 (34%) had urinary urgency without incontinence, urinary urgency with incontinence, and urinary frequency, respectively; and of the 19 nonfallers, two (11%), none, and two (11%) had urinary urgency without incontinence, urinary urgency with incontinence, and urinary frequency, respectively.
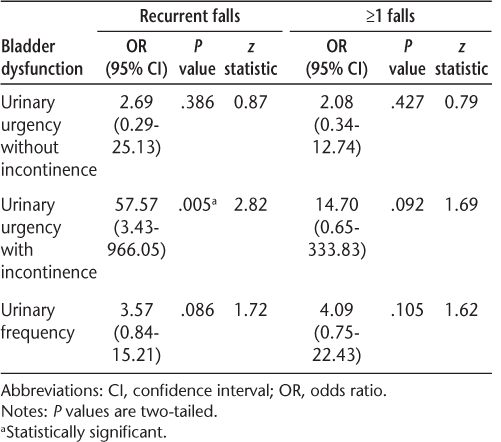
Adjusted analyses revealed a significant association between having urinary urgency with incontinence and recurrent falls (OR, 57.57; 95% CI, 3.43–966.05; P = .005). Standard diagnostics demonstrated that the logistic regression model fit the observed data well (McFadden's R 2 = 0.3).27 The ability of the model to discriminate recurrent fallers from nonrecurrent fallers was assessed by computing the area under the receiver operating characteristic curve, which was 0.815.
After adjusting for the potential confounders of age, sex, and disability, we did not find significant associations between urinary urgency without incontinence (OR, 2.69; 95% CI, 0.29–25.13; P = .386) or urinary frequency (OR, 3.57; 95% CI, 0.84–15.21; P = .086) and recurrent falls (two or more falls compared with fewer than two falls). We also did not find significant associations between urinary urgency with incontinence (OR, 14.70; 95% CI, 0.65–333.83; P = .092), urinary urgency without incontinence (OR, 2.08; 95% CI, 0.34–12.74; P = .427), or urinary frequency (OR, 4.09; 95% CI, 0.75–22.43; P = .105) and sustaining one or more falls (compared with no falls) (Table 2). In all the regression models, the assumption of linearity was satisfied. For all the adjusted analyses, age, sex, and disability were not significantly associated with recurrent falls or one or more falls. Power analysis revealed that the association between urinary urgency with incontinence and recurrent falls was powerfully significant, having achieved an observed post hoc power of 96%. The nonsignificant trends observed for the relationships between urinary frequency and recurrent falls and between urinary urgency with incontinence and one or more falls were expectedly underpowered, achieving post hoc power of 36% and 42%, respectively. With respect to potential future studies, sample size estimates are large but not necessarily intractable, needing a total of approximately 125 individuals to observe statistically significant associations between falls and either urinary frequency or urinary urgency dysfunction.
Relationship between bladder dysfunction and fall status adjusted for age, sex, and disability
Effect Modification
Age, sex, and disability were not effect modifiers in the relationship between urinary urgency with and without urinary incontinence and fall status.
Discussion
In this study, we found a statistically significant association between baseline urinary urgency with incontinence and subsequent recurrent falls (two or more falls in 3 months) after adjusting for age, sex, and disability (EDSS score) in people with mild-to-moderate RRMS. We did not find significant associations between urinary urgency without incontinence or urinary frequency and subsequent falls or between urinary urgency with incontinence and any (one or more) falls in the 3 months after baseline.
These findings help clarify the previous controversy in the literature regarding the association between bladder symptoms and subsequent falls in people with MS. It is likely that Gunn and colleagues13 found an association between urinary incontinence and subsequent falls when Nilsagård and colleagues2 did not find such an association because Gunn's group looked at recurrent falls (ie, two or more falls) and Nilsagård's group looked at any falls (ie, one or more falls). We found an association between the bladder symptoms of urgency with incontinence and recurrent falls but not between urinary urgency with incontinence and one or more falls.
Various mechanisms may underlie an association between urinary urgency with incontinence and recurrent falls, including specific behaviors, such as rushing to the restroom to avoid incontinence and dehydration because of avoiding drinking water28; adverse effects of anticholinergic or antimuscarinic medications used for the management of neurogenic bladder dysfunction6 29 30; or the common pathology of spinal cord lesions contributing to both problems. The persistence of this association after adjusting for EDSS score argues against a strong influence of the common pathology of spinal cord lesions. We did not have sufficient information about behaviors or medication use to further explore these potential relationships.
The number of fallers in this study was similar to that reported in other studies of falls in people with MS. Approximately 63% of this sample fell once or more, comparable with the 63% reported by Nilsagård et al.,2 and approximately 30% fell twice or more, fewer than reported by Gunn et al.13 (~53%) and Matsuda et al.14 (~45%). The prevalence of urinary dysfunction in the present cohort was fairly comparable with that of previous studies in people with MS. In the present study, 29% had urinary urgency, 25% had urinary frequency, and 16% had urinary incontinence. Previous studies in people with MS report approximately 24% to 86% having urinary urgency, 17% to 82% having urinary frequency, and 34% to 72% having urinary incontinence.7 We also observed that although several participants had urinary urgency without incontinence, none had incontinence without urgency. This suggests that having urinary urgency with incontinence may occur subsequent to having urinary urgency without incontinence, but urodynamic evaluation is needed to fully assess the nature and severity of bladder dysfunction and its effect on the upper and lower urinary tracts.
The average level of disability in the present study, as assessed by the EDSS, was lower than that in previous studies examining the association between bladder symptoms and prospectively assessed falls. In this study, the median EDSS score was 3.0, whereas in the studies by Nilsagård et al.2 and Gunn et al.,13 the median EDSS score was 4.0 to 4.5. The high prevalence of falls and bladder dysfunction in all of these samples suggest that both falls and bladder dysfunction are common, early, and persistent symptoms in MS.
This study has several strengths. Falls were prospectively counted using a fall calendar to limit recall bias, and participants were reminded to record their falls and submit their calendars to reduce loss to follow-up. We also delineated different types of bladder symptoms rather than assessing only the effect of any bladder symptoms. In addition, we identified different associations between bladder symptoms and any falls or multiple falls. It has been suggested that multiple falls are more clinically relevant because multiple falls may be more likely to increase risk of injury and reduce activity, participation, and quality of life.
This study also has several limitations. The sample size was small and included only individuals 50 years and younger with RRMS, limiting generalizability. It is also not known whether these findings will hold true for falls occurring beyond 3 months after baseline. This evaluation of bladder symptoms, although more detailed than any previous studies, was limited. We asked participants about urinary frequency, urgency, and incontinence but not about nocturia (need to wake in the night to urinate), a symptom of overactive neurogenic bladder that is a known risk factor for falls in older adults.10 11 We also did not ask about urinary tract infections, which are associated with a worsening of MS symptoms31 and with falls in older adults.32 In addition, the present study did not quantify the severity of urinary symptoms, which would allow for a dose response assessment of the effect of bladder dysfunction on fall risk. Further larger-scale prospective studies of longer duration with more heterogeneous samples and more complete evaluation of urinary dysfunction are needed to verify the associations we detected.
Although preliminary, the results of this study, combined with those of previous studies demonstrating an association between bladder dysfunction and falls in people with MS, are potentially clinically important. Multidisciplinary fall prevention programs are recommended for people with MS. The results of this study suggest that such programs should particularly be considered for reducing fall risk in recurrent fallers and that such programs should include strategies for managing urinary urgency with incontinence.
Conclusion
The results of this study support that urinary urgency with incontinence is an independent risk factor for recurrent falls occurring within 3 months after baseline in adults with RRMS. This is an important finding because urinary urgency with incontinence is often amenable to physical, behavioral, and pharmaceutical interventions.29 This study also draws attention to the wide range of potential consequences of bladder incontinence, a symptom possibly underreported in certain patient populations.14 33 Further studies specifically designed and powered to investigate the association between bladder dysfunction and falls are needed to fully understand this relationship and to evaluate whether including treatment of urinary urgency with incontinence in fall prevention interventions helps prevent falls and their sequelae and improve quality of life.
PracticePoints
People with MS who have urinary urgency and incontinence are likely at greater risk for falls than those without these symptoms.
MS patients should be asked about bladder symptoms and fall history.
Treating bladder symptoms in people with MS may provide benefits beyond direct effects on the bladder.
Acknowledgments
We thank the study participants for their time and support in this study and urologist Dr. Nina Davis and neurologist Dr. Dennis Bourdette for their invaluable expertise and feedback.
References
Gunn HJ, Newell P, Haas B, Marsden JF, Freeman JA. Identification of risk factors for falls in multiple sclerosis: a systematic review and meta-analysis. Phys Ther. 2013; 93:504–513.
Nilsagård Y, Lundholm C, Denison E, Gunnarsson L-G. Predicting accidental falls in people with multiple sclerosis: a longitudinal study. Clin Rehabil. 2009; 23:259–269.
Peterson EW, Cho CC, Finlayson ML. Fear of falling and associated activity curtailment among middle aged and older adults with multiple sclerosis. Mult Scler. 2007; 13:1168–1175.
Brønnum-Hansen H, Hansen T, Koch-Henriksen N, Stenager E. Fatal accidents among Danes with multiple sclerosis. Mult Scler. 2006; 12:329–332.
Mahajan ST, Patel PB, Marrie RA. Under treatment of overactive bladder symptoms in patients with multiple sclerosis: an ancillary analysis of the NARCOMS Patient Registry. J Urol. 2010; 183:1432–1437.
Kalsi V, Fowler CJ. Therapy insight: bladder dysfunction associated with multiple sclerosis. Nat Clin Pract Urol. 2005; 2:492–501.
Betts CD, D'Mellow MT, Fowler CJ. Urinary symptoms and the neurological features of bladder dysfunction in multiple sclerosis. J Neurol Neurosurg Psychiatry. 1993; 56:245–250.
Ginsberg D. The epidemiology and pathophysiology of neurogenic bladder. Am J Manag Care. 2013; 19:s191–s196.
Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988; 319:1701–1707.
Hunter KF, Voaklander D, Hsu ZY, Moore KN. Lower urinary tract symptoms and falls risk among older women receiving home support: a prospective cohort study. BMC Geriatr. 2013;13:46.
Parsons JK, Mougey J, Lambert L, et al. Lower urinary tract symptoms increase the risk of falls in older men. BJU Int. 2009; 104:63–68.
Finlayson ML, Peterson EW, Cho CC. Risk factors for falling among people aged 45 to 90 years with multiple sclerosis. Arch Phys Med Rehabil. 2006; 87:1274–1279.
Gunn H, Creanor S, Haas B, Marsden J, Freeman J. Risk factors for falls in multiple sclerosis: an observational study. Mult Scler. 2013; 19:1913–1922.
Matsuda PN, Shumway-Cook A, Bamer AM, Johnson SL, Amtmann D, Kraft GH. Falls in multiple sclerosis. Phys Med Rehabil. 2011; 3:624–632.
Sung J, Shen S, Motl RW, Sosnoff JJ. Bladder function and falls in individuals with multiple sclerosis. Disabil Rehabil. 2016; 38:2193–2197.
Sosnoff JJ, Socie MJ, Boes MK, et al. Mobility, balance and falls in persons with multiple sclerosis. PLoS One. 2011;6:e28021.
Cameron MH, Thielman E, Mazumder R, Bourdette D. Predicting falls in people with multiple sclerosis: fall history is as accurate as more complex measures. Mult Scler Int. 2013;2013:496325.
Polman CH, Reingold SC, Edan G, et al. Diagnostic criteria for multiple sclerosis: 2005 revisions to the “McDonald Criteria.” Ann Neurol. 2005;58:840–846.
Kurtzke JF. Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS). Neurology. 1983; 33:1444–1452.
Hauer K, Lamb SE, Jorstad EC, Todd C, Becker C. Systematic review of definitions and methods of measuring falls in randomised controlled fall prevention trials. Age Ageing. 2006; 35:5–10.
Lamb SE, Jørstad-Stein EC, Hauer K, Becker C. Development of a common outcome data set for fall injury prevention trials: the Prevention of Falls Network Europe consensus. J Am Geriatr Soc. 2005; 53:1618–1622.
Rubenstein LZ, Josephson KR. Falls and their prevention in elderly people: what does the evidence show? Med Clin North Am. 2006; 90:807–824.
Nilsagård Y, Gunn H, Freeman J, et al. Falls in people with MS: an individual data meta-analysis from studies from Australia, Sweden, United Kingdom and the United States. Mult Scler. 2015; 21:92–100.
MacLennan AH, Taylor AW, Wilson DH, Wilson D. The prevalence of pelvic floor disorders and their relationship to gender, age, parity and mode of delivery. Br J Obstet Gynaecol. 2000; 107:1460–1470.
Sosnoff JJ, Sandroff BM, Pula JH, Morrison SM, Motl RW. Falls and physical activity in persons with multiple sclerosis. Mult Scler Int. 2012;2012:315620.
Heinze G, Schemper M. A solution to the problem of separation in logistic regression. Stat Med. 2002; 21:2409–2419.
McFadden D. Quantitative methods for analyzing travel behaviour of individuals: some recent developments. In: Hensher DA, Stopher PR, eds. Behavioural Travel Modelling. London, UK: Croom Helm; 1978:279–318.
Goldstein DS, Sharabi Y. Neurogenic orthostatic hypotension: a pathophysiological approach. Circulation. 2009; 119:139–146.
Stoffel JT. Contemporary management of the neurogenic bladder for multiple sclerosis patients. Urol Clin North Am. 2010; 37:547–557.
Ooi WL, Hossain M, Lipsitz LA. The association between orthostatic hypotension and recurrent falls in nursing home residents. Am J Med. 2000; 108:106–111.
Mahadeva A, Tanasescu R, Gran B. Urinary tract infections in multiple sclerosis: under-diagnosed and under-treated? a clinical audit at a large university hospital. Am J Clin Exp Immunol. 2014; 3:57–67.
Rowe TA, Juthani-Mehta M. Urinary tract infection in older adults. Aging Health. 2013; 9:519–528.
DeMaagd GA, Davenport TC. Management of urinary incontinence. Phys Ther. 2012; 37:345–361.







