Publication
Research Article
International Journal of MS Care
Interest in Providing Multiple Sclerosis Care and Subspecializing in Multiple Sclerosis Among Neurology Residents
Author(s):
Background: Although detailed knowledge regarding treatment options for multiple sclerosis (MS) patients is largely limited to neurologists, shortages in the neurologist workforce, including MS subspecialists, are predicted. Thus, MS patients may have difficulties in gaining access to appropriate care. No systematic evaluation has yet been performed of the number of neurology residents planning to pursue MS subspecialization. This study identifies factors affecting interest in providing MS patient care or MS subspecialization among current neurology residents.
Methods: We randomly selected half of all Accreditation Council of Graduate Medical Education–certified neurology residency programs in the continental United States to receive the neurology resident survey. Completed surveys were received from 218 residents.
Results: Residents were significantly more likely to have increased interest in MS care when they participated in MS research, were interested in teaching, and indicated that the “ability to improve patient outcomes and quality of life” was a positive factor influencing their desire to provide MS patient care. Residents who were interested in providing MS care, interested in teaching, and indicated that “research opportunities” was a positive factor for providing MS patient care were significantly more likely to express interest in MS subspecialization.
Conclusions: Increasing opportunities to interact with MS patients, learn about MS care, and participate in MS research may increase interest in MS care and subspecialization among neurology residents. Opportunities to educate residents regarding MS patient care may affect residents’ attitudes.
Multiple sclerosis (MS) is a chronic neurologic disease resulting in demyelination and axonal loss within the central nervous system. Over the past several years, treatment options for individuals with MS have expanded, including additional disease-modifying agents that can reduce relapses and decrease disease progression.1 Detailed knowledge regarding appropriate treatment options for MS patients is largely limited to neurologists and, within this physician specialist population, to MS subspecialists. More than 90% of MS patients have indicated that they receive treatment, assistance in obtaining medications, support, and education about their disease from neurologists.2 Further, receipt of treatment from neurologists is associated with higher quality of care3 and greater likelihood of receipt of disease-modifying agents.4
No systematic evaluation has been performed of the number of neurologists specializing in MS care. Reports of shortages among the overall neurologist workforce have existed for almost 3 decades.5 A report by the Workforce Task Force of the American Academy of Neurology6 projects a 19% shortfall in supply of neurologists by the year 2025. Anecdotal evidence suggests an inadequate supply of MS subspecialists, based on difficulty in filling MS subspecialist positions, waiting lists for new patients, and patient groups describing difficulties finding available MS subspecialists. Information on the projected future workforce of MS physicians is critical to ensure optimal care among individuals with MS. The objective of this study was to elucidate factors associated with interest in providing care to individuals with MS or subspecializing in MS care among current neurology residents.
Methods
Instrument Development
To develop the MS Physician Workforce Study Neurology Resident Survey, we initially reviewed previously developed physician career surveys to identify items relevant to assessing neurology residents’ current interest in providing care to MS patients and pursuing MS subspecialization. After compiling these items, we selected and adapted existing questions and crafted new items to create a draft neurology resident survey. The draft survey included questions on respondents’ future career plans (ie, following residency training) including subspecialization programs of interest, factors influencing subspecialization decisions (in general, not specific to MS), interest in providing MS care and MS subspecialization, exposure to MS patients and MS patient care resources during residency training, and factors indicating limits on or positive influences toward providing MS patient care once the resident was in clinical practice. Plans for future time to be spent in research, teaching, and providing MS patient care (following residency training) were rated using a 5-point Likert scale ranging from “none” to “all my time.” Factors influencing subspecialization decisions were also rated using a 5-point Likert scale ranging from “not at all important” to “extremely important.”
For assessing factors influencing future provision of MS patient care, residents were asked to respond to the questions “Which of the following factors could play a role in limiting the number of MS patients you would want to see once you have a clinical practice?” (eight choices) and “Which of the following factors could have a positive influence on your desire to provide care to MS patients once you have a clinical practice?” (seven choices). Residents were instructed to “mark all that apply,” and could indicate any, all, or none of these factors.
Exposure to MS patient care resources during residency included MS clinics and MS care teams. Although the term was not defined on the survey, we expected that residents would consider MS clinics to be outpatient encounters in a venue offering a range of medical care services and involving health-care professionals who specialize in MS care. MS care teams represent a coordinated group of health-care professionals with expertise in MS, but are not necessarily located in a specific clinic or venue dedicated to MS care.
We also tested the comprehensiveness and usability of the survey. The final version of the survey was approved by the RTI International Institutional Review Board prior to distribution. The survey is published as a supplementary file in the online version of this article at http://ijmsc.org.
Survey Administration
We developed a two-stage survey design in which Stage 1 randomly sampled geographically stratified neurology residency programs and Stage 2 obtained responses from neurology residents within these programs. The sampling frame consisted of all Accreditation Council of Graduate Medical Education (ACGME)–certified neurology residency programs in the continental United States and Puerto Rico. We stratified each residency program into one of four census regions (Northeast, South, West, and Midwest) and randomly selected half of the residency programs in each census region, for a total of 64 programs. We sent directors of the selected residency programs a cover letter describing the study and requesting that the directors distribute paper copies of the survey and return mailing materials (included with the cover letter) to all program residents. The cover letter, which indicated endorsement of this study by the National Multiple Sclerosis Society, also offered residents the opportunity to take the survey online. Residents who completed the survey received a $25 Visa gift card.
We tracked responses to determine whether residents from particular programs had submitted any completed surveys; if no residents from a given program submitted responses, we sent a reminder letter to the resident director at 2 weeks and then again at 6 weeks after the initial mailing. We received at least one survey response from 44 of the sampled programs (Stage 1 response rate of 70%). Among the responding programs, 218 residents submitted survey responses (Stage 2 response rate of 31%).
Analysis
For analyses, the study population was categorized based on self-reported demographic characteristics, including age group (categorized in quartiles), sex, race (white, Asian or Pacific Islander, and black or other race, the latter two groups being combined because of small numbers of black respondents), and ethnicity (Hispanic/Latino or not). Number of MS patients seen per year was categorized in approximate tertiles of 0 to 10, 11 to 30, and 31 or more.
The primary study outcome measures were interest in providing MS care and interest in MS subspecialization. Neurology residents’ interest in providing MS care was classified into three categories based on the time they would ideally like to devote to MS patient care following completion of training: “none” or “a little” (categorized as “not interested”), “some” (categorized as “moderately interested”), or “a lot” or “all my time” (categorized as “very interested”). Similar criteria were applied to corresponding questions on time devoted to research and time devoted to teaching to identify residents not, moderately, or very interested in research or teaching, respectively. Residents’ ratings of the importance of factors influencing decisions to pursue subspecialty training (not restricted to MS) were classified into only two categories owing to more limited distribution of responses: “somewhat or less important” versus “very or extremely important.”
Residents were classified as interested in MS subspecialization if they responded affirmatively to the survey question “Have you considered or are you considering a fellowship in MS as subspecialty training?” This “interest in MS subspecialization” variable did not take into account other areas of interest for subspecialization. We therefore also explored a dependent variable of “focused interest in MS subspecialization,” defined as an indication of interest in MS subspecialization as their only subspecialization choice or as one of two clinical areas specified for subspecialization. There were insufficient numbers of residents (n = 13) to examine factors associated with interest in only MS subspecialization.
We used χ2 tests (or, as necessary because of small cell sizes, Fisher’s exact tests) to examine relationships between discrete variables and multivariate logistic regression models to identify predictors of increased interest in providing MS care (ordered logistic regression, with three-level dependent variable) and of interest in MS subspecialization. These models included independent variables related to MS patient exposure during residency, future interest in research or teaching, attitudes toward MS patient care, and demographic characteristics that were statistically significant (P < .05) or approached statistical significance (P < .10) in bivariate analyses of either dependent variable (interest in MS care or interest in MS subspecialization), as presented in Tables 1 to 3. The regression model examining interest in MS subspecialization also included interest in providing MS care and factors associated with the decision to pursue subspecialty training as independent variables. All variables included in regression analyses were examined for multicollinearity (Variance Inflation Factor > 5) prior to inclusion in the final model.
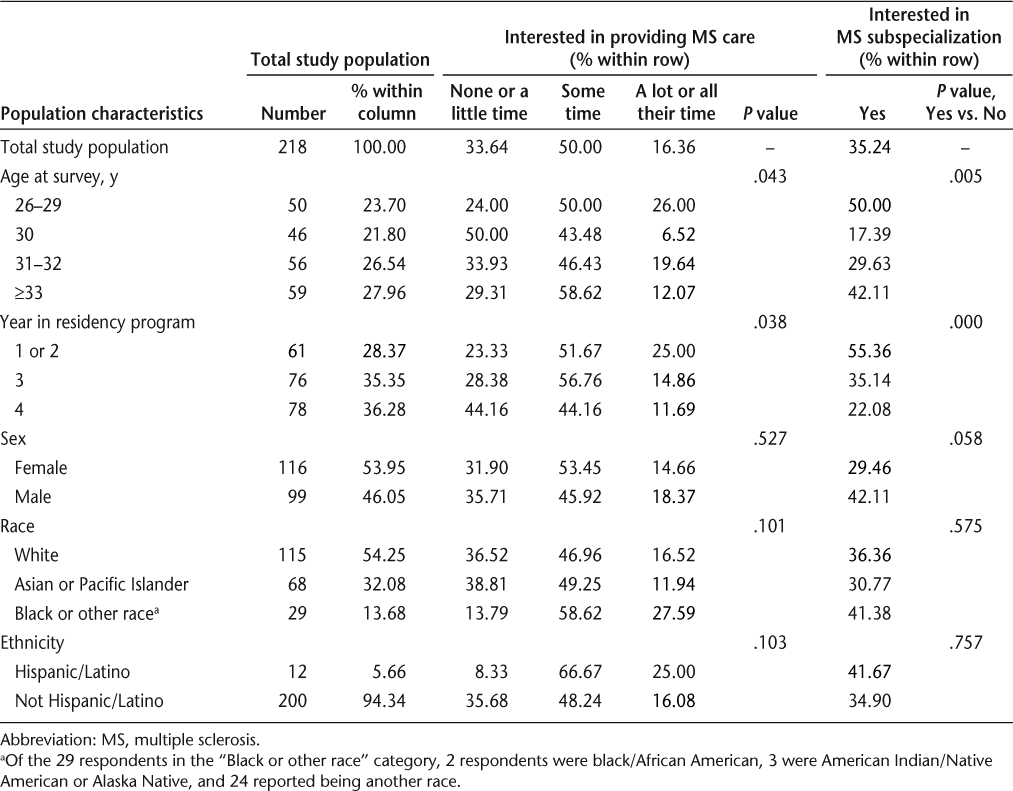
Characteristics of study population by interest in providing MS care and interest in MS subspecialization
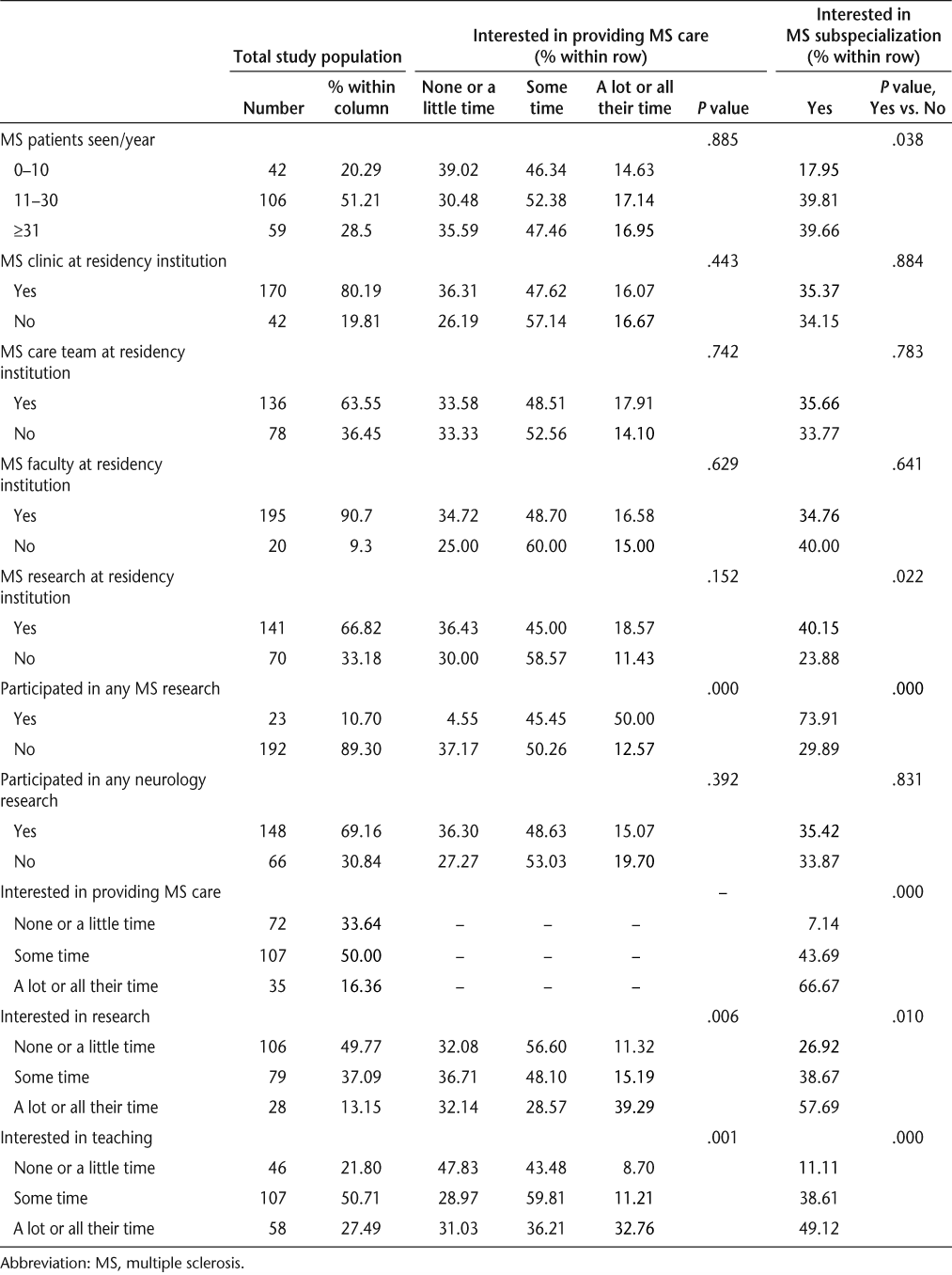
Relationship of MS patient exposure during residency and research/teaching plans with interest in MS care and interest in providing MS subspecialization
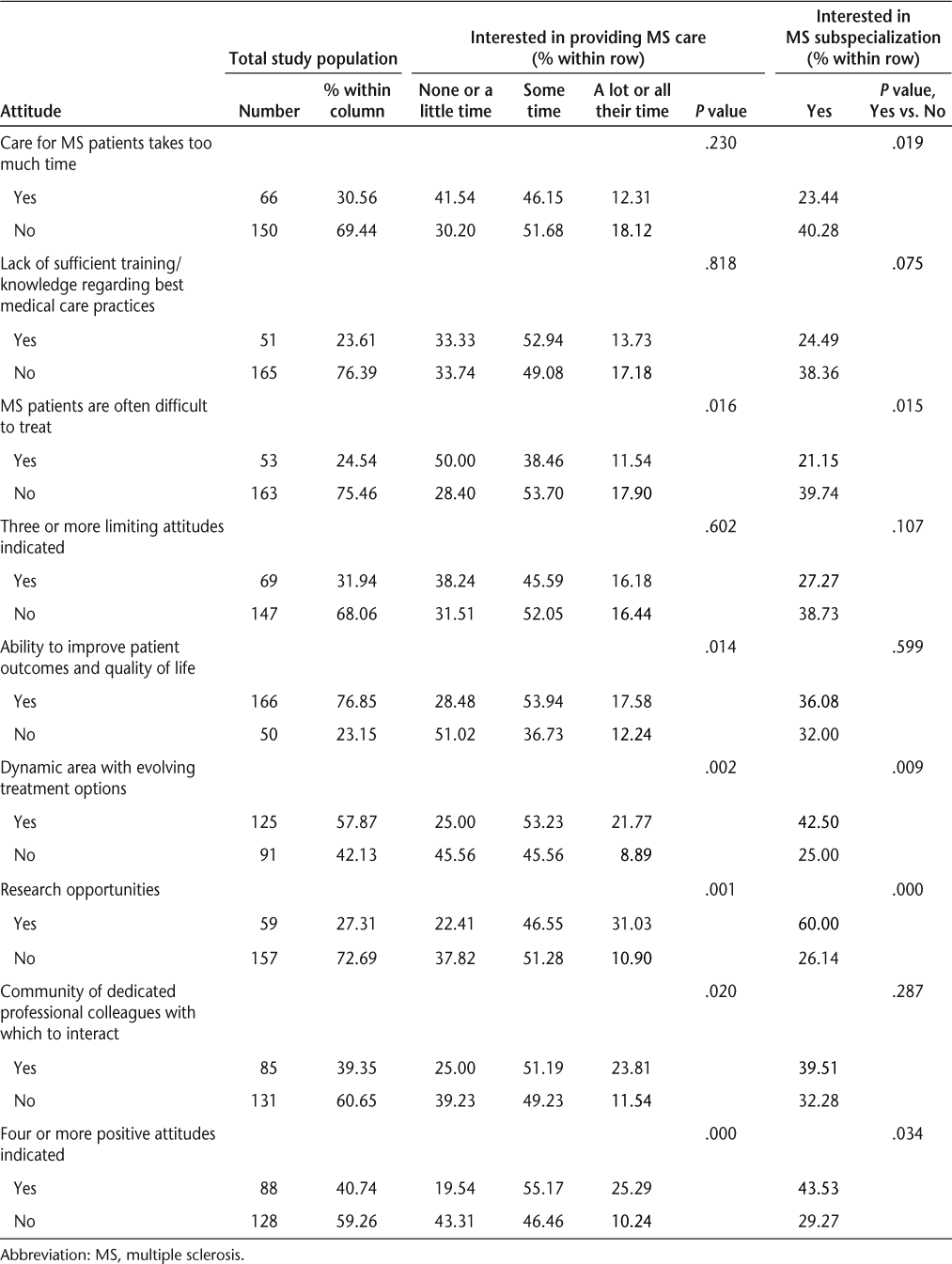
Relationship of attitudes toward MS patient care with interest in providing MS care and interest in MS subspecialization
Missing data generally comprised less than 2% of responses, and individuals with missing data for descriptive, bivariate, or regression analyses were excluded from those analyses. We defined P < .05 as the criterion for statistical significance and classified analysis results with P > .05 but < .10 as marginally significant.
Results
Population Characteristics
The study population consisted of 218 neurology residents. After excluding 4 neurology residents who did not respond to the question on interest in providing MS care, 142 (66%) expressed interest in providing MS care (ie, indicated that they would like to devote at least some of their time to providing MS care) and 72 (34%) were not interested. After excluding 8 neurology residents who were not aware of MS fellowships or did not respond to the question, 74 (35%) expressed interest in MS subspecialization and 136 (65%) were not interested.
Characteristics Associated with Interest in Providing MS Care
Neurology residents very interested in MS care (ie, indicating spending “a lot” or “all my time” in MS care in the resident survey) were more likely to be in the youngest age group and the first or second year of their residency program (Table 1). Male residents were marginally more interested in MS subspecialization than were females. Neurology residents from larger residency programs did not differ significantly in interest in providing MS care or interest in MS subspecialization from residents from smaller programs (data not shown). All residency programs in our sample were located in metropolitan core areas, so we were unable to examine differences based on urban versus rural locale.
As shown in Table 2, participation in any MS research, level of interest in research, and level of interest in teaching were also significantly associated with level of interest in providing MS care. Residents very interested in MS care were more likely to have participated in MS research and to be very interested in research and teaching than were residents not interested in MS care.
Residents indicating “MS patients are often difficult to treat” as a factor that could limit the number of MS patients they would see once in clinical practice were less likely to express interest in providing MS care (Table 3). In contrast, the percentage of neurology residents very interested in MS care was significantly higher among those who indicated several positive factors associated with MS patient care: “ability to improve patient outcomes and quality of life,” “dynamic area with evolving treatment options,” “research opportunities,” and “community of dedicated professional colleagues with which to interact.” Residents very interested in MS care were also significantly more likely to indicate four or more positive factors influencing their desire to provide MS patient care once in clinical practice.
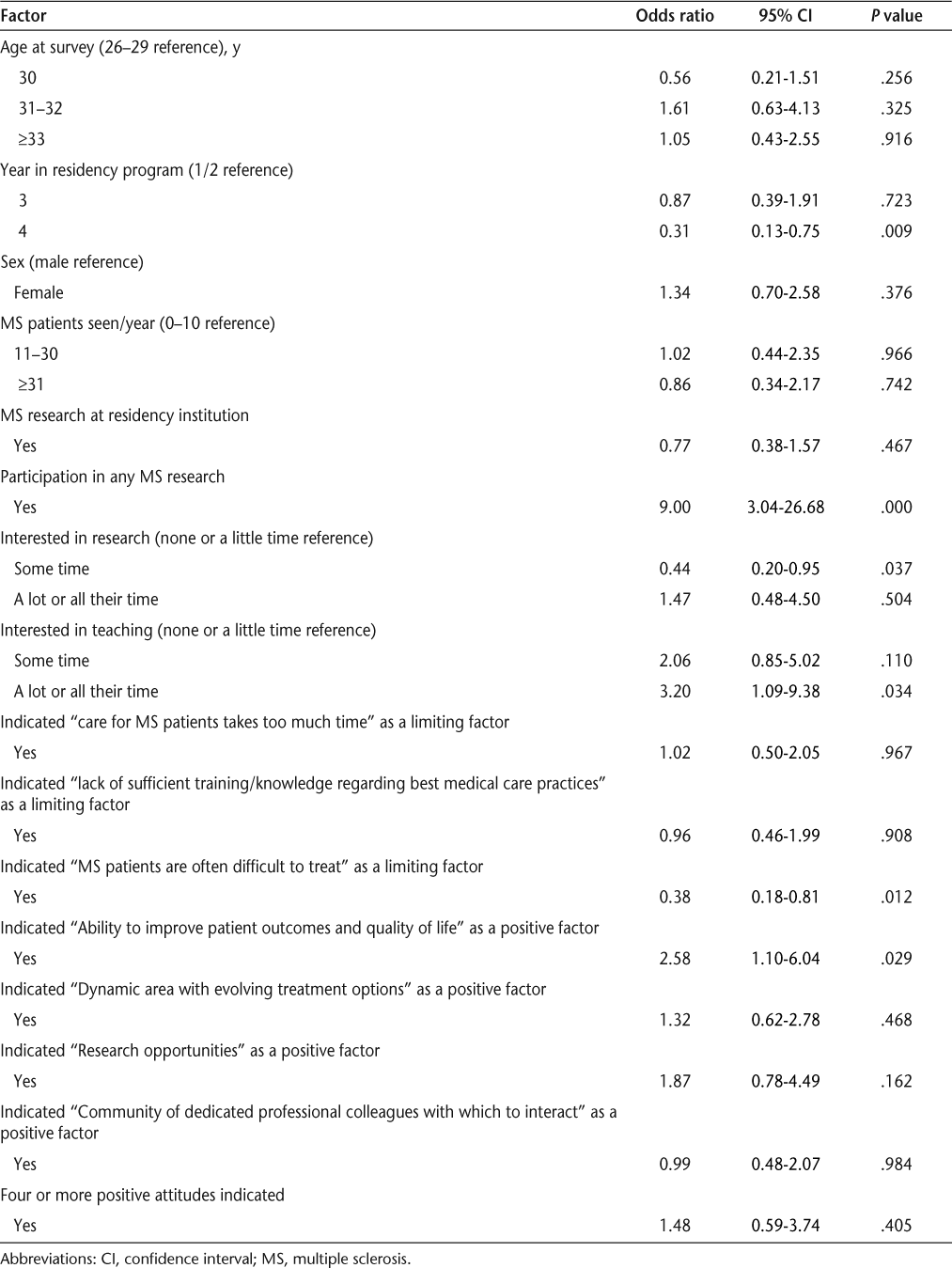
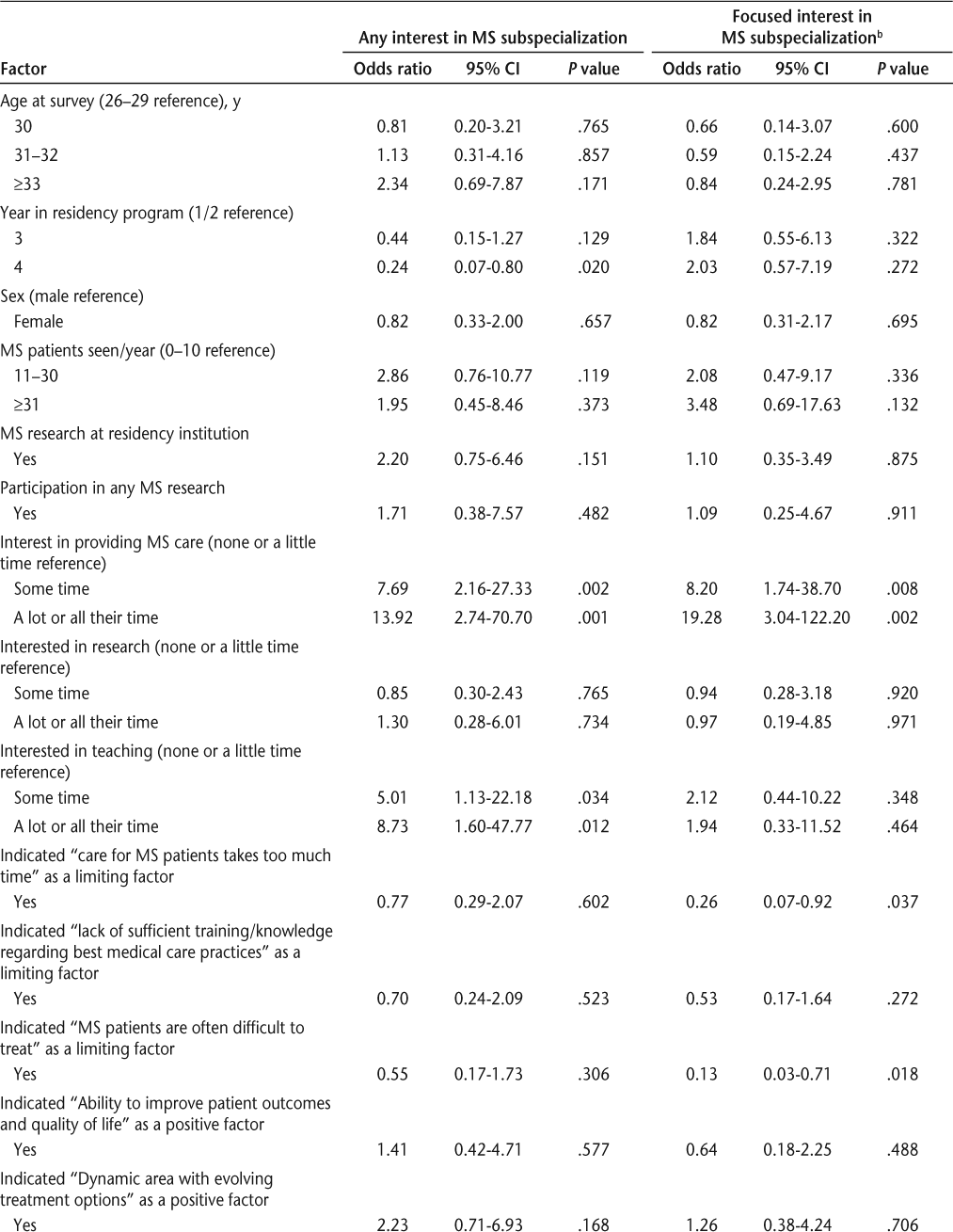
We used an ordered logistic regression model to examine the association of resident demographic characteristics, exposure to MS patients during residency, research and teaching plans, and attitudes toward MS patient care with level of interest in providing MS care (Table 4). All survey items that had significant or marginally significant associations with self-reported interest in providing MS care or interest in MS subspecialization in bivariate analyses (Tables 1–3) were included as independent variables in this regression model. In this analysis, residents were significantly more likely to have increased interest in MS care when they participated in any MS research, were very interested in teaching (compared with those not interested in teaching), and indicated that the “ability to improve patient outcomes and quality of life” was a positive factor influencing their desire to provide MS patient care once in clinical practice. Residents were significantly less likely to be interested in MS care when they were in the fourth year of their residency program (compared with those in the first or second year of their residency program) and indicated that “MS patients are often difficult to treat” as a factor that could limit the number of MS patients seen once in clinical practice. Residents who indicated moderate interest in research were also significantly less likely to be interested in MS care (compared with those not interested in research). In contrast, residents very interested in research or indicating “research opportunities” as a positive factor were more interested in providing MS care, but these effects did not reach statistical significance.
Ordered logistic regression analysis of factors associated with interest in providing MS care
Characteristics Associated with Interest in MS Subspecialization
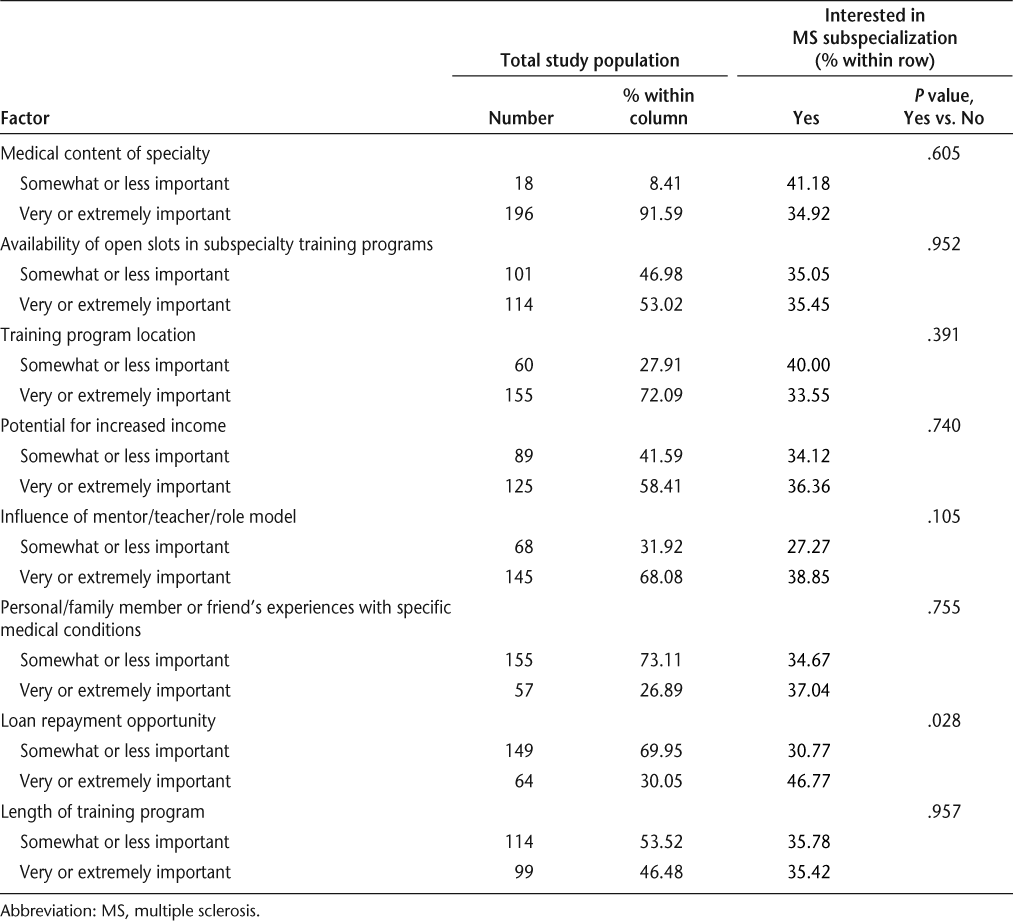
Neurology residents who were interested in MS subspecialization were more likely to be in the youngest or oldest age category and in the first or second year of their residency program (Table 1). They were more likely to have seen greater numbers of MS patients, have ongoing MS research studies at their residency institutions, have participated in any MS research, and express interest in spending more time providing MS care, conducting research, and teaching (Table 2). Residents interested in MS subspecialization were less likely to indicate that the following factors could limit the number of MS patients seen once in clinical practice: “care for MS patients takes too much time,” “lack of sufficient training/knowledge regarding best medical care practices,” and “MS patients are often difficult to treat.” These residents were more likely to indicate “dynamic area with evolving treatment options” and “research opportunities” as factors that could have a positive influence on their desire to provide MS patient care once in clinical practice and to indicate four or more positive factors (Table 3). Among factors potentially influencing the decision whether to pursue subspecialty training in general, residents indicating that loan repayment opportunities were an important factor in subspecialty decisions were more likely to express interest in MS subspecialization.
In logistic regression analysis including all significant or marginally significant variables from Tables 1 to 3 and Table 5, several factors were significantly associated with residents’ interest in MS subspecialization (Table 6). Residents in their fourth program year were significantly less likely to be interested in MS subspecialization compared with those in their first or second year. Residents who were moderately or very interested in providing MS care, moderately or very interested in teaching, and indicated that “research opportunities” was a positive factor influencing their desire to provide MS patient care once in clinical practice were significantly more likely to express interest in MS subspecialization.
Relationship of factors potentially influencing the decision to pursue subspecialty training with interest in MS subspecialization
Logistic regression analysis of factors associated with interest in MS subspecializationa
Logistic regression analysis of factors associated with interest in MS subspecializationa
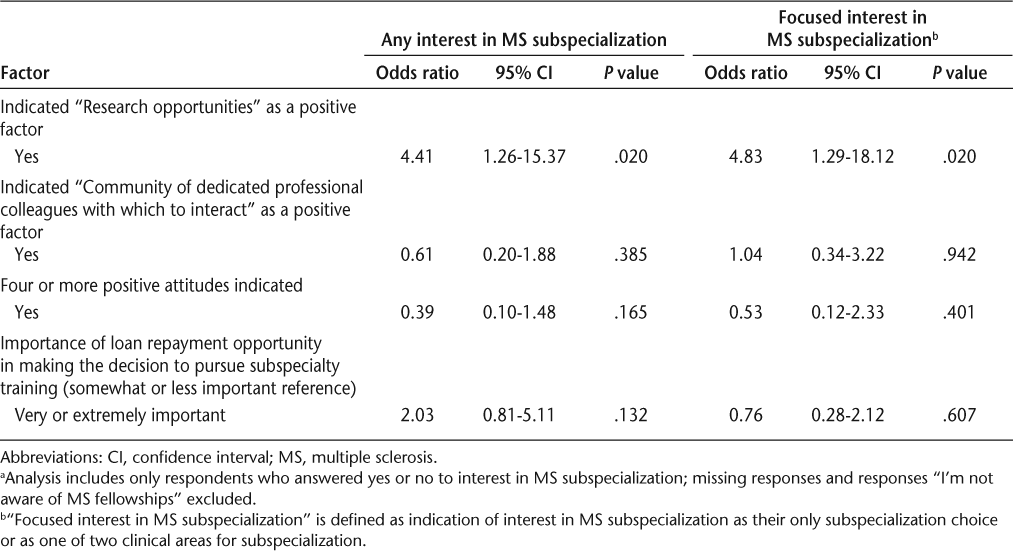
We also examined whether these same variables (from Tables 1–3 and Table 5) were significantly associated with “focused interest” in MS subspecialization (Table 6). As discussed in the Methods section, we classified residents as having focused interest in MS subspecialization if they were considering MS subspecialization plus at most one additional subspecialization area. This measure therefore indicates more selective interest in MS subspecialization than does the outcome of any interest in this area of subspecialization. In logistic regression analysis, residents who were moderately or very interested in providing MS care and indicated that “research opportunities” was a positive factor influencing their desire to provide MS patient care once in clinical practice were significantly more likely to express a focused interest in MS subspecialization; these results were very similar to those from regression analyses of any interest in MS subspecialization. Residents indicating “care for MS patients takes too much time” and “MS patients are often difficult to treat” as factors that could limit the number of MS patients they would see once in clinical practice were significantly less likely to express a focused interest in MS subspecialization. Interestingly, while overall interest in MS subspecialization decreased among residents in their third or fourth program year, focused interest in MS subspecialization increased in these later-year residents, although this increase was not statistically significant.
Discussion
This study yielded information on interest in providing care for individuals with MS and in subspecializing in MS among a sample of neurology residents. An important finding of this study was overall high levels of interest in MS patient care, with 66% of residents expressing an interest in MS care and 35% expressing interest in MS subspecialization. However, the levels of interest in MS care and subspecialization were significantly lower among fourth-year residents (Table 1). There are a number of possible explanations for this finding. When starting a neurology residency program, residents may be aware of only a limited number of subspecialty opportunities. Because individuals with MS are frequently encountered at academic medical centers, new residents may be aware of opportunities to provide care for MS patients and subspecialize in their care. As residents progress through their training programs, they may learn of other subspecialization opportunities (eg, clinical neurophysiology) that they did not know of previously and may decide to focus on other groups of patients and pursue subspecialties other than MS.
Although interest in MS subspecialization decreases with year of residency, interest in a number of other subspecialties also decreases with time in residency program (data not shown). This may reflect neurology residents’ becoming more focused and considering fewer subspecialties over time. We observed that the average number of subspecialty programs considered by neurology residents decreases over time, from 1.92 among first- or second-year residents to 1.59 among third-year residents to 1.13 among fourth-year residents (data not shown). The significant decrease in resident interest in MS subspecialization over time likely reflects (at least in part) more specific focus by residents on their career path of interest. In addition, while any interest in MS subspecialization decreased with year in residency program (likely reflecting the decreased number of subspecialty programs of interest going from the start of residency to year 4), focused interest in MS subspecialization was greater among residents in their third or fourth program year, although this difference was not statistically significant. Therefore, residents who have more specific interest in MS subspecialization at the start of residency appear to either maintain this interest or show a trend for increased focus on this subspecialty while excluding other potential areas of subsequent training.
Our analyses found a significant association between number of MS patients seen per year and interest in MS subspecialization (Table 2), although this was not statistically significant in multivariate regression analysis (Table 6). This association may reflect greater exposure to individuals with MS during residency training leading to increased interest in careers focusing on this patient group. Alternatively, it is possible that residents who are more interested in MS subspecialization will select MS electives during their residency and thus see more MS patients because of prior interest in this area. It is not possible to determine the direction of this association with our available data, and both of these factors may be important.
We can, however, examine differences in residents’ attitudes toward MS patient care to explore whether the association between number of MS patients seen and interest in MS subspecialization reflects a priori interest in MS care versus interest in MS that develops following greater patient exposure. During required rotations, neurology residents may predominantly see MS patients whose disease is not well managed, potentially leading to a skewed view of MS patient care. In contrast, MS electives often include interactions with individuals in ambulatory care settings, exposing residents to MS patients whose disease may be better controlled and who have fewer symptoms and less disability. If residents who saw more MS patients did so through MS electives, these residents would likely have greater interactions with MS patients having well-controlled disease. As a consequence, we would expect that residents seeing more MS patients would be less likely to indicate limiting attitudes about MS patient care such as “MS patients are difficult to care for” or “MS patients have multiple comorbidities.” We found no significant association between numbers of MS patients seen and agreement with these two limiting attitudes on MS patient care (data not shown). We therefore assume that, at least in part, residents who have the opportunity to see more individuals with MS do so as part of their required rotations, and are more likely to develop interest in this clinical area as a career focus after this increased MS patient exposure.
In bivariate analyses (Table 5), residents who expressed interest in MS subspecialization were more likely to indicate that loan repayment opportunities were a moderately or very important factor in making subspecialty training decisions in general. Loan repayment opportunities were not significantly associated with interest in MS subspecialization in the multivariate regression model (Table 6). MS subspecialization may have lower income prospects compared to other neurology subspecialties, according to members of this study’s advisory panel. As such, individuals interested in MS subspecialization may have increased concerns regarding their ability to repay educational loans if they were to pursue additional training in this area. However, this factor appears to have only a limited impact on subspecialization choice.
Our findings indicate that interest and participation in research was associated with greater interest in MS. As presented in Tables 4 and 6, participation in MS research, desire to spend a lot or all of their time performing research, and viewing “research opportunities” as a positive factor for MS patient care were associated with increased interest in both MS patient care and MS subspecialization, although not all of these associations reached statistical significance. However, the questions on research in the resident survey correspond to three different dimensions. Participation in MS research captured previous experience among residents; those who had participated in MS research were highly motivated to provide MS patient care. In contrast, desired time to be spent performing research as a part of future careers (ie, following residency training) may relate to type of career track. Residents who responded that they wanted to spend a lot or all of their time in research were likely interested in academic careers. Finally, viewing “research opportunities” as a positive factor for MS patient care may relate to both interest in performing research and interest in providing care for individuals with MS. These residents are among those most likely to indicate focused interest in MS subspecialization (Table 6). Thus, while interest in research is generally associated with interest in MS care, the differences in type of research interest may provide important information on differences in career plans and desired future role related to MS patient care.
Analyses of differences between any interest in MS subspecialization and “focused interest” in this area of subspecialization (Table 6) showed an additional important finding. Residents indicating that “care for MS patients takes too much time” and “MS patients are often difficult to treat” were significantly less likely to express a focused interest in MS subspecialization. However, neither of these limiting factors was significantly associated with overall interest in MS subspecialization. This suggests that these attitudes may have critical impacts, discouraging residents with some interest in MS from pursuing this area of subspecialization. These results suggest several approaches to addressing potential shortages among neurologists providing care for individuals with MS or subspecializing in MS patient care. Exposure to a broader range of MS patients, including those whose disease is well controlled, and education regarding expected outcomes among individuals whose disease is well managed, may affect interest in MS care and subspecialization. In particular, exposure to broader groups of MS patients could affect the limiting attitudes of MS patient care being too difficult and requiring too much time, which differentiate any interest from focused interest in MS subspecialization. Providing educational opportunities regarding the range of disease among individuals with MS may also be relevant for medical students, prior to selection of a residency field.
In addition, more information on research opportunities related to MS and additional programs to facilitate resident research in this area may increase interest in MS care and subspecialization. Among neurology residents responding to this survey who were not interested in MS patient care, approximately 30% indicated that mini-grant funding in MS research or the availability of a mentor directing MS research would have encouraged them to participate in research in MS (data not shown). Similarly, among residents not interested in MS subspecialization, 30% indicated that mini-grant funding would have encouraged their participation in MS research and 47% indicated that a research mentor would have encouraged participation in this research area (data not shown). Thus, additional information on MS research and new opportunities to participate in this research may be important steps to address shortages in the MS physician workforce.
A number of limitations are associated with this study. First, although neurology residency programs identified to receive the survey were randomly selected from all US neurology programs, distribution of the survey to the residents was dependent on the residency director. Also, residents self-selected whether to respond to the survey. Either of these factors could bias the study population, reducing the generalizability of the results. The study population of 218 residents, while representing a Stage 2 response rate of more than 30% (and thus not unusual for this type of survey), is fairly small; factors that were only marginally associated with the study outcome measures (interest in MS patient care and MS subspecialization) may actually have stronger associations. In addition, all data were collected by self-response to the survey; no attempt was made to validate these responses. Finally, as with any survey, we were limited in the number of items included and the range of responses to the items. Although we included open-ended response opportunities with several items and an open-ended comment section at the end of the survey, we likely did not capture all factors related to interest in providing MS care and MS subspecialization among neurology residents.
Despite these limitations, this study provides important new information for addressing potential shortages among neurologists focused on providing MS patient care. Several actionable items, such as increasing exposure to MS patients and to research opportunities related to MS patient care, may increase interest in MS. Our subsequent work to project the adequacy of the future MS physician workforce will explore the potential impacts of these actions and assist in developing policy recommendations to address physician shortages that may adversely affect MS patient care.
PracticePoints
Predicted shortages among neurologists may increase the difficulty of people with MS in obtaining care. Identifying factors that encourage neurology residents’ interest in providing MS patient care and pursuing MS subspecialization may help to address these potential physician shortages.
Providing educational opportunities that give neurology residents exposure to a broader range of MS patients, including those whose disease is well controlled, may increase interest in providing MS care and subspecializing in MS and decrease perceptions that MS patient care is too difficult and requires too much time.
Offering additional MS research opportunities (eg, mini-grants) and providing research mentors may promote neurology residents’ interest in MS care and MS subspecialization.
Acknowledgments
The authors would like to thank Dr. Nicholas LaRocca and the National Multiple Sclerosis Society for their funding of this study and guidance during the study. We would also like to thank members of the MS Physician Workforce Study Advisory Panel for their thoughtful comments on earlier versions of the manuscript. Advisory Panel members include Dr. Corey Ford, Dr. Barbara Giesser, Ms. June Halper, Dr. Shana Johnson, Dr. Aaron Miller, and Dr. Steven Ringel.
References
Bandari DS, Sternaman D, Chan T, Prostko CR, Sapir T. Evaluating risks, costs, and benefits of new and emerging therapies to optimize outcomes in multiple sclerosis. J Manag Care Pharm. 2012; 18: 1–17.
National Multiple Sclerosis Society and Teva Neuroscience. Multiple Sclerosis Trend Report: Perspectives from Managed Care, Providers, and Patients. Washington, DC: Kikaku America International; 2007.
Buchanan R, Kaufman M, Zhu L, James W. Patient perceptions of multiple sclerosis-related care: comparisons by practice specialty of principal care physician. NeuroRehabilitation. 2008; 23: 267–272.
Minden SL, Hoaglin DC, Hadden L, Frankel D, Robbins T, Perloff J. Access to and utilization of neurologists by people with multiple sclerosis. Neurology. 2008;70(13 Pt 2):1141–1149.
Dyken ML. The continuing undersupply of neurologists in the 1980s: impressions based on data from three studies. Neurology. 1982; 32: 651–656.
Dall TM, Storm MV, Chakrabarti R, et al. Supply and demand analysis of the current and future US neurology workforce. Neurology. 2013; 81: 470–478.
Funding/Support: This study was funded by the National Multiple Sclerosis Society (Award No. HC0121).
Financial Disclosures: The authors have no conflicts of interest to disclose.







