Publication
Research Article
International Journal of MS Care
Impact of Pilates Exercise in Multiple Sclerosis
Author(s):
CME/CNE Information
Activity Available Online:
To access the article, post-test, and evaluation online, go to http://www.cmscscholar.org
Target Audience:
The target audience for this activity is physicians, physician assistants, nursing professionals, and other health-care providers involved in the management of patients with multiple sclerosis (MS).
1) Recognize the lack of evidence for Pilates exercise in MS and the limitations of the current body of evidence.
2) Understand how Pilates exercise improves walking ability in individuals with MS.
Learning Objectives:
Accreditation Statement:

In support of improving patient care, this activity has been planned and implemented by the Consortium of Multiple Sclerosis Centers (CMSC) and Delaware Media Group. CMSC is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Physician Credit
The CMSC designates this journal-based activity for a maximum of 0.5 AMA PRA Category 1 Credit(s) ™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nurse Credit
The CMSC designates this enduring material for 0.5 contact hours (none in the area of pharmacology).
Disclosures:
Editor in Chief of the International Journal of MS Care (IJMSC), has served as Physician Planner for this activity. He has received royalties from Springer Publishing, intellectual property rights/patent holder from Biogen, and consulting fees from Ipsen Pharma, and has performed contracted research for Biogen, Adamas Pharmaceuticals, and Acorda Therapeutics.Francois Bethoux, MD,
has served as reviewer for this activity. She has disclosed no relevant financial relationships.Laurie Scudder, DNP, NP,
has disclosed no relevant financial relationships.Whitney R.D. Duff, PhD,
has disclosed no relevant financial relationships.Justin W. Andrushko, MSc,
has disclosed no relevant financial relationships.Doug W. Renshaw, MEd,
has disclosed no relevant financial relationships.Philip D. Chilibeck, PhD,
has disclosed no relevant financial relationships.Jonathan P. Farthing, PhD,
is the co-owner of Lead Pilates and Integrated Health Therapies, where the study interventions occurred.Jana Danielson, MBA,
has disclosed no relevant financial relationships.Charity D. Evans, PhD,
The peer reviewers for the IJMSC have disclosed no relevant financial relationships.
The staff at the IJMSC, CMSC, and Delaware Media Group who are in a position to influence content have disclosed no relevant financial relationships.
Note: Disclosures listed for authors are those applicable at the time of their work on this project and within the previous 12 months.
Method of Participation:
Release Date: April 1, 2018
Valid for Credit Through: April 1, 2019
In order to receive CME/CNE credit, participants must:
1) Review the continuing education information, including learning objectives and author disclosures.
2) Study the educational content.
3) Complete the post-test and evaluation, which are available at http://www.cmscscholar.org.
Statements of Credit are awarded upon successful completion of the post-test with a passing score of >70% and the evaluation.
There is no fee to participate in this activity.
Disclosure of Unlabeled Use:
This educational activity may contain discussion of published and/or investigational uses of agents that are not approved by the FDA. CMSC and Delaware Media Group do not recommend the use of any agent outside of the labeled indications. The opinions expressed in the educational activity are those of the faculty and do not necessarily represent the views of CMSC or Delaware Media Group.
Disclaimer:
Participants have an implied responsibility to use the newly acquired information to enhance patient outcomes and their own professional development. The information presented in this activity is not meant to serve as a guideline for patient management. Any medications, diagnostic procedures, or treatments discussed in this publication should not be used by clinicians or other health-care professionals without first evaluating their patients' conditions, considering possible contraindications or risks, reviewing any applicable manufacturer's product information, and comparing any therapeutic approach with the recommendations of other authorities.
Abstract
Background:
Pilates is a series of exercises based on whole-body movement and may improve mobility in people with multiple sclerosis (MS). The purpose of this study was to determine the effect of Pilates on walking performance in people with MS.
Methods:
30 individuals with MS who were not restricted to a wheelchair or scooter (Patient-Determined Disease Steps scale score <7) were randomized to receive Pilates (twice weekly) and massage therapy (once weekly) or once-weekly massage therapy only (control group). The Pilates was delivered in a group setting (five to ten participants per session). The primary outcome was change in walking performance (6-Minute Walk Test) after 12 weeks. Secondary outcomes included functional ability (Timed Up and Go test), balance (Fullerton Advanced Balance Scale), flexibility (sit and reach test), body composition (dual-energy X-ray absorptiometry), core endurance (plank-hold test), and muscle strength and voluntary activation (quadriceps). Intention-to-treat analysis was performed using a two-factor repeated-measures analysis of variance.
Results:
Walking distance increased by a mean (SD) of 52.4 (40.2) m in the Pilates group versus 15.0 (34.1) m in the control group (group × time, P = .01). Mean (SD) time to complete the Timed Up and Go test decreased by 1.5 (2.8) seconds in the Pilates group versus an increase of 0.3 (0.9) seconds in the control group (group × time, P = .03). There were no other significant differences between groups over time.
Conclusions:
Pilates improved walking performance and functional ability in persons with MS and is a viable exercise option to help manage the disease.
Evidence consistently shows that exercise therapy has beneficial effects on physical performance and quality of life in persons with multiple sclerosis (MS).1–3 Pilates is a series of exercises based on whole-body movement that emphasizes awareness of body structure, body alignment, and muscle recruitment with a focus on stabilizing core muscles during dynamic movement. As such, Pilates may have a beneficial effect in persons with MS because activation of core muscles could combat difficulties with mobility and balance.4 5 A modest 10% to 14% improvement in walking performance has been reported with Pilates, along with improvements in functional ability, balance, strength, and well-being.4 6–11 However, previous studies have been limited by low frequency of Pilates exercises (once-weekly 30-minute sessions),4 7 restrictive inclusion criteria (lower disability thresholds), and nonrandomized study design.6 8 9 Furthermore, the potential benefits of Pilates include alleviation of side-to-side strength imbalances and an improved ability to recruit motor neurons, which is severely affected in persons with MS.12 13 These potential benefits are due to the emphasis of Pilates training on body alignment and muscle recruitment. The primary purpose of this study was to determine the impact of a Pilates exercise program on walking ability in people with MS when conducted at a frequency recommended by the Canadian Physical Activity Guidelines for Adults with MS.14 The secondary purpose of this study was to explore the potential impact of a Pilates exercise program on quality of life and additional physical performance indicators, including functional ability; balance; flexibility; body composition; core endurance; quadriceps strength, fatigability, and voluntary muscle activation; and daily/weekly physical activity. Although some of these additional indicators have been recorded in previous Pilates research, muscle strength and neural activation have not been studied and may help determine mechanisms by which mobility might be improved. We hypothesized that Pilates exercises would improve walking ability, physical performance, and quality of life.
Methods
Study Design
This was a single-blinded, parallel-group, randomized controlled trial conducted over a 12-week period. Participants were randomized 1:1 to the Pilates or control group after completing baseline testing. Randomization was performed using a computer-generated allocation schedule, with a block size of two, by a researcher (C.D.E.) who was not involved in baseline or outcome assessment or in the statistical analysis. Researchers involved in outcome assessment and analysis were blinded to group assignment, with statistical analysis blinded through coding of the study groups.
Participants
Participants were recruited through advertisement by the local MS Society of Canada office and social media from November 20, 2016, through January 20, 2017. The inclusion criteria were purposely kept broad and consisted of a definite diagnosis of MS, not restricted to a wheelchair or scooter, and the ability to travel to the assessment (University of Saskatchewan) and intervention (Lead Pilates and Integrative Therapies) sites, both located in Saskatoon, Saskatchewan, Canada. To keep the study as real-world as possible, participants were not excluded because of involvement in previous or current exercise programs.
Based on a meta-analysis of Pilates in older adults, we estimated a Hedges' g effect size of 1.39 for improvement in walking performance.15 Using this effect size, a power of 80%, and an α of .05, we determined that ten participants per group were required. We aimed to recruit 15 participants per group (30 total) to account for potential attrition. All the participants signed informed consent forms and completed the Physical Activity Readiness Questionnaire for Everyone16 before baseline testing to ensure that there were no contraindications to exercise participation. The study was approved by the University of Saskatchewan Biomedical Ethics Review Board.
Pilates and Control
The Pilates intervention consisted of two 50-minute Pilates sessions per week. The Pilates sessions were led by experienced Comprehensive Certified Pilates instructors with training on adapting Pilates exercises for individuals with MS. The 12-week program included exercises in the standing position on the CoreAlign apparatus (www.pilates.com; Balanced Body, Sacramento, CA) and floor mat work. Each session started with a warm-up and ended with a cool-down. A range of exercises were performed, such as the CoreAlign “hoof” (focused on gait) and “angels in the snow” (focused on shoulder mobility). Existing exercises progressed in difficulty, and new exercises were introduced over the study period based on each participant's individual performance. A detailed curriculum of the Pilates program is available from the authors on request. The Pilates sessions were conducted in a group setting (n = 5–10) but were individualized to each participant's ability level and focused on proper breathing, correct body alignment, and core stabilization. Participants in the Pilates group also received a weekly 1-hour massage therapy session with a registered massage therapist specially trained in massage for MS.
Participants in the control group received only the once-weekly 1-hour massage therapy session. Massage therapy was chosen as the control because it has the potential to improve some outcomes in MS (eg, pain and stress) but would have minimal effect on the primary (walking ability) and secondary (muscular strength and endurance) outcomes.17 All the Pilates and massage therapy sessions occurred at the same location (Lead Pilates and Integrated Therapies). To ensure that the study was as pragmatic as possible, participants were not restricted from performing other exercise during the study period.
Outcomes
The primary outcome was walking ability as assessed via the 6-Minute Walk Test (6MWT), per the guidelines provided by the American Thoracic Society.18 In brief, participants were instructed to walk as far as possible in 6 minutes by walking back and forth on a 100-ft course while using their typical assistive devices. Rest breaks were permitted, although the stopwatch continued to run during breaks, and the total distance was recorded. In exception to the guidelines, the researcher (W.R.D.D.) administering the test walked alongside the participant due to safety concerns surrounding the course (eg, doorways, floor transition molding).18 Secondary outcomes included functional ability (Timed Up and Go [TUG] tests with left and right turns)19; balance (Fullerton Advanced Balance Scale)20; flexibility (sit-and-reach test); body composition (dual-energy X-ray absorptiometry)21; core endurance (plank-hold test)22; quadriceps strength (maximum voluntary contraction), fatigability (sustained maximum voluntary contraction torque drop), and voluntary muscle activation (interpolated twitch technique) (Figure S1, which is published in the online version of this article at ijmsc.org); daily/weekly physical activity (Actical accelerometers [Respironics, Bend, OR])23; and quality of life (Multiple Sclerosis Quality of Life–54 instrument).24 Many of the secondary outcomes were exploratory in nature in an attempt to determine the feasibility of measuring these outcomes for future exercise-related studies in the MS population. As well, outcomes such as muscle strength and neural activation are novel to the present study and may be helpful in determining mechanisms by which mobility might be improved. Detailed protocols for all the secondary outcomes are available in Appendix S1. All the outcome measures were assessed at baseline and within 1 week after the end of the intervention. All the assessments were completed at research facilities located at the University of Saskatchewan.
Statistical Analysis
Baseline characteristics were compared between groups using one-way analysis of variance (ANOVA). A two-factor repeated-measures ANOVA with between-group factor for study group (Pilates vs. control) and within-group factor for time (baseline vs. postintervention at 12 weeks) was used. We reported effect size via partial eta-squared () and significance at P ≤ .05 for differences in the mean change over time between groups (ie, the group × time interaction). All data were checked and cleared for skewness and kurtosis, as well as for outliers. Welch's F tests were used in place of ANOVA to adjust for homogeneity of variance violations where appropriate. All the results are expressed as mean (SD) or mean absolute changes and 95% CIs. Data were analyzed on both an intention-to-treat (missing data were carried forward from the last recorded value) and per-protocol basis using IBM SPSS Statistics for Windows (version 24.0; IBM Corp, Armonk, New York).
Results
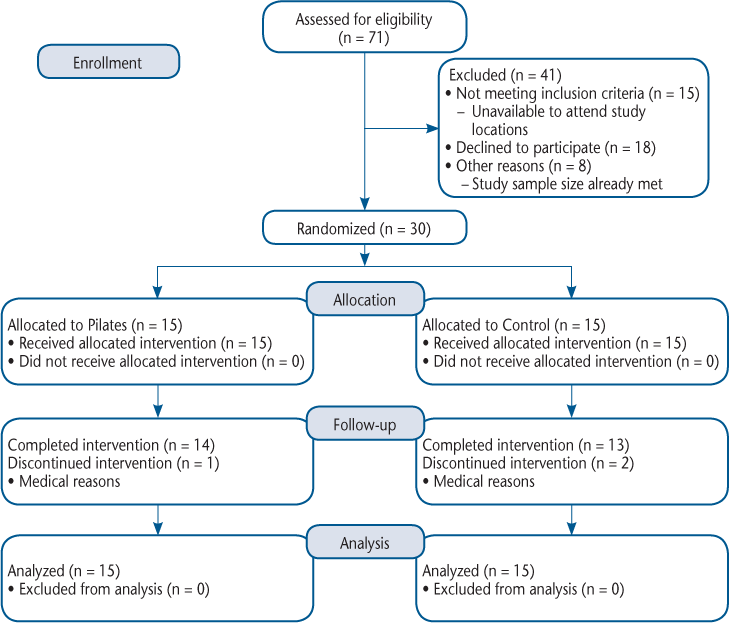
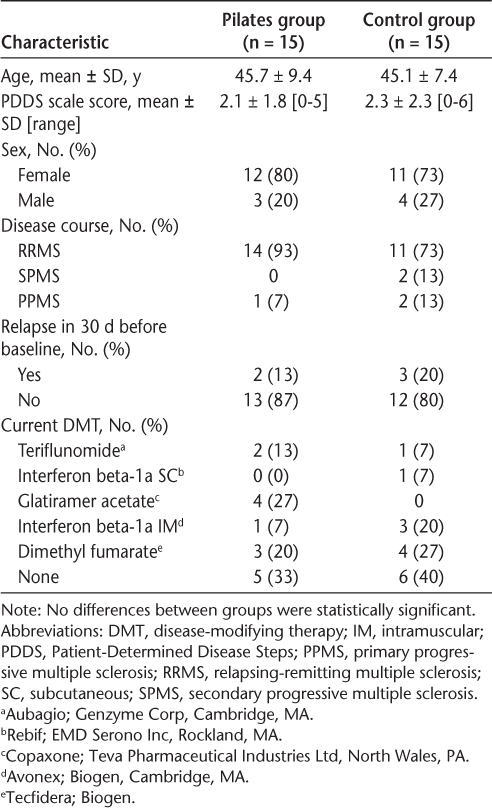
A total of 71 individuals were identified as potential participants; 30 were randomized to either the Pilates or control group (Figure 1). The mean (SD) participant age was 45.4 (8.3) years, and 77% were women. Baseline characteristics were similar between groups (Table 1). Compliance with the Pilates intervention was high, with a mean (SD) of 84.8% (15.5%) of sessions attended (median, 88.0%; range, 36%–100%). Three participants (one in the Pilates group and two in the control group) were not able to complete postintervention testing due to medical reasons but were still included in the final analyses.
CONSORT flow diagram
Baseline characteristics
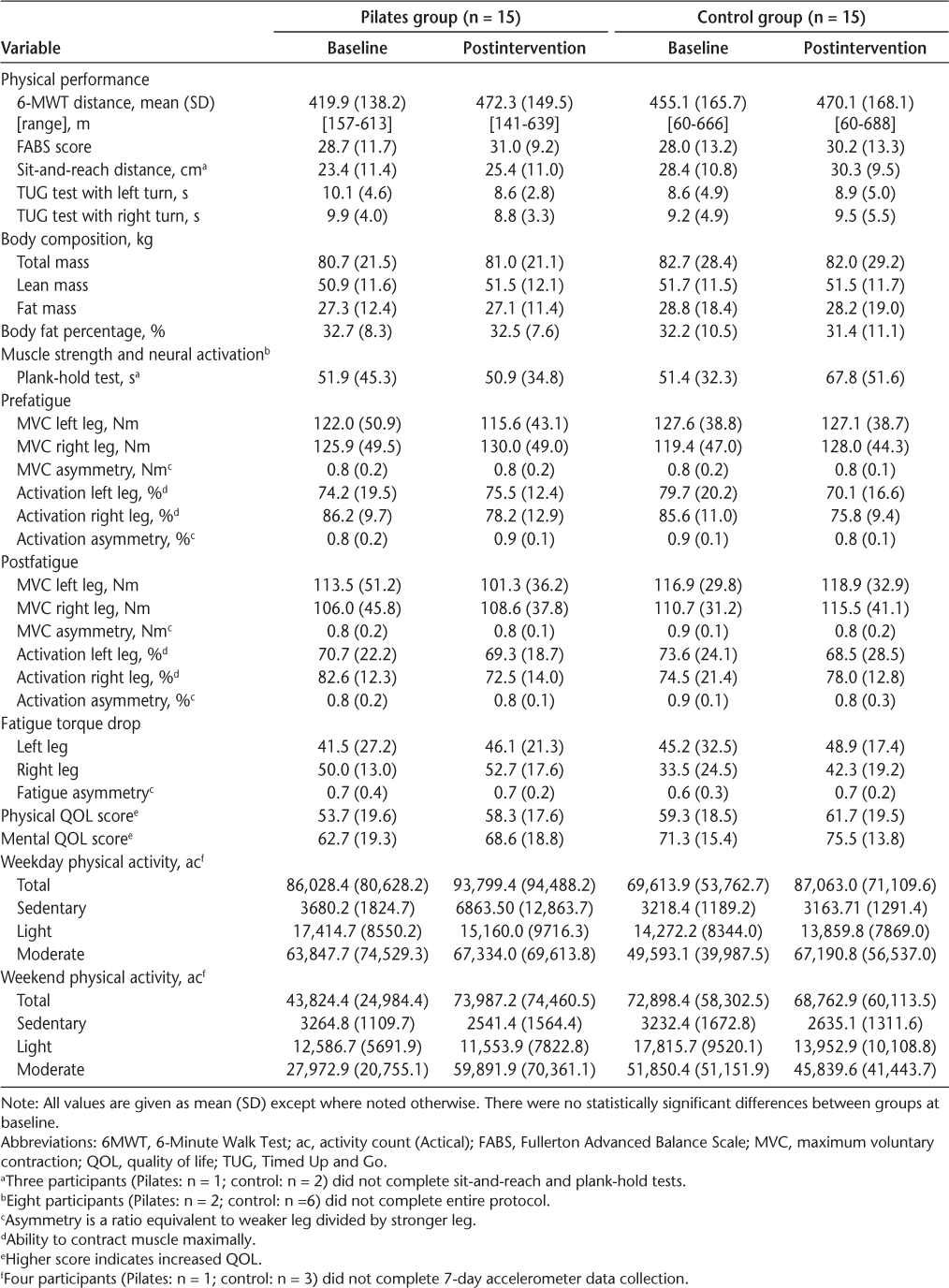
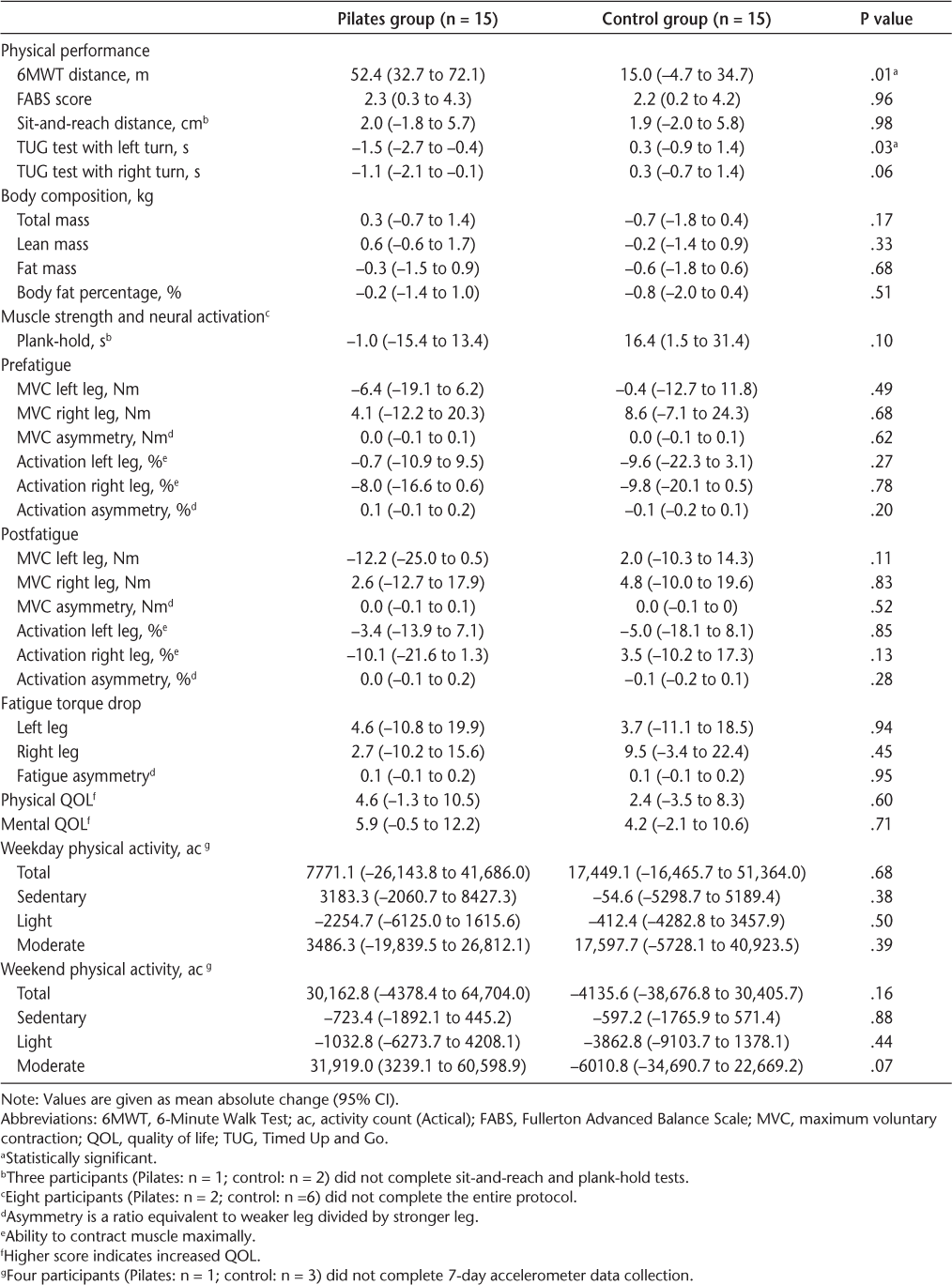
The distance covered in the 6MWT increased by a mean of 52.4 m in the Pilates group compared with 15.0 m in the control group (group × time, P = .01) (Table 2). Although baseline scores were not statistically different between groups, we also adjusted for the baseline 6MWT distance using analysis of covariance and found similar results (P = .01 for the difference in post-training scores between groups adjusted for baseline scores). No differences between groups were observed for any of the secondary outcomes except for functional ability (Tables 2 and 3). Results of the TUG test with a left turn improved in the Pilates group, with a mean (SD) decrease of 1.5 (2.8) seconds compared with an increase of 0.3 (0.9) seconds for the control group (group × time, P = .03) (Table 3).
Baseline and postintervention data by group
Mean absolute changes from baseline to 12 weeks for all outcomes within groups
No adverse events were reported in either group during the intervention. However, one participant experienced severe muscle spasticity of the leg during the baseline stimulation protocol. This person fully recovered within 2 hours of the testing.
Discussion
In this 12-week randomized study, a Pilates exercise program improved walking distance and a measure of independent functional ability (TUG test) in individuals with MS. There were no differences between groups for a variety of secondary end points, including balance, flexibility, muscle strength, and quality of life.
Although it is known that physical activity is beneficial for individuals with MS,2 3 only a few studies have specifically examined Pilates, and none have been conducted in a Canadian cohort to our knowledge. The present observations of a 15% benefit in walking performance and some improved functional ability with Pilates exercises support previous studies.4,6–8,11 A 12-week Pilates program improved walking speed (Timed 10-Meter Walk test)4 and distance (2-Minute Walk Test and 6MWT) and functional ability (TUG test),7 but no more so than standardized physical therapy exercises. In the first study, improvements in walking speed were small and nonsignificant, although this could be due to the poor compliance to Pilates reported during the study.4 The Pilates interventions for both of these studies were limited to once-weekly 30-minute, mat-based sessions; this is below the recommended frequency of at least 2 days of strength training exercises per week for adults with MS.14 A higher-frequency (60 minutes, thrice weekly) 12-week Pilates program improved speed, coordination, and dynamic balance compared with a control, but not more than an aquatic training program of the same frequency.8 However, these results were based on per-protocol analyses including only participants with greater than 80% compliance with the Pilates intervention.8 Improvements in functional ability were observed with an 8-week program with two 60-minute Pilates sessions weekly, although no comparisons with a control group were reported.6 We attempted to improve on previous research by including participants with a wider range of disease severity, increasing the frequency of the Pilates exercises, and using the CoreAlign apparatus.
The improvement in walking ability that we observed may be partially a result of the CoreAlign exercises, which focus on improving gait by maintaining proper alignment and activation of the hamstrings. We observed a mean improvement in walking performance of 15%, which is less than the 20% considered clinically relevant.25 However, the mean improvement in TUG test time of 1.8 seconds is similar to the statistically significant difference of 1.2 seconds found when comparing older adult fallers and nonfallers.26 Such improvements may suggest that Pilates could be beneficial as a complementary therapy for managing MS in some individuals. Previous work has theorized that improvements in mobility are a result of increased core strength, stability, and activation with Pilates.6 11 Although the present study did not directly evaluate these variables, our measure of core endurance (timed plank) did not improve with Pilates compared with the control group. We also did not observe a difference in neuromuscular performance (strength, voluntary activation) of the legs. Thus, the improvements in mobility from Pilates may also be due to improved kinesthetic awareness, particularly during ambulation. Regardless of the specific mechanism of action, Pilates seems to be beneficial for individuals with MS.
Although pharmacologic options are available for the treatment of MS, there remains debate around the long-term effectiveness27–29 and concerns with the safety profiles, and a lack of long-term surveillance of the newer agents exists.30–35 This, and the fact that not everyone is eligible for these drugs, leads many individuals to seek nonpharmacologic methods, including exercise, to help manage their disease. However, given the demonstrated value of physical activity in general, exercise should be a consideration in the management of MS, regardless of an individual's pharmacologic status. Therefore, identifying Pilates as a safe and effective exercise option for individuals with MS is an important finding.
The strengths of this well-powered study include the randomized controlled design, the use of a reliable primary end point commonly used in MS research,36 and an intervention frequency that fulfills the current Canadian recommendations for strength training exercises in MS.14 We intentionally left the inclusion criteria broad to allow for participants with a range of ability and previous activity levels. This, combined with the fact that the intervention was conducted in an existing Pilates studio, increased the generalizability of the findings. However, limitations to this study exist. We assessed a large number of secondary outcomes without statistical adjustment. Although only one secondary outcome was statistically significantly different between groups (TUG with a left turn, P = .03), it is possible that this result was due to chance rather than to the Pilates intervention. Not all of the secondary outcomes were measured by tests specific to MS, such as the Fullerton Advanced Balance Scale, which was developed to identify balance problems in functionally independent older adults,20 and caused a ceiling effect for participants with lower disease severity in the present study. However, to our knowledge, this is one of the first studies to explore the potential neural mechanisms for improved physical performance in MS and to look at changes in training.13 Although we did not observe any statistically significant results for these outcomes, we were able to determine the feasibility of measuring such outcomes for future exercise-related studies in MS populations. We chose a primary end point that focused on mobility, which is not a symptom for all individuals with MS; however, the 6MWT is responsive to change,37 has excellent reliability,36 38 and is strongly correlated to subjective measures of fatigue and quality of life.36 39 Finally, we were unable to assess whether the benefits in mobility were sustained once the intervention was completed.
In conclusion, Pilates is a safe and effective exercise option for improving mobility in individuals with MS. Future studies should compare Pilates therapy with other exercise therapies and evaluate other outcomes important in MS.
PRACTICE POINTS
Evidence consistently shows that exercise therapy has beneficial effects on physical performance and quality of life in individuals with MS. As a series of exercises based on whole-body movement, Pilates may improve physical functioning in people with MS.
Walking ability was improved after a 12-week Pilates program in individuals with MS; no adverse events were reported.
This study adds to the growing body of literature suggesting that Pilates is a safe and effective exercise option for MS and can be used by individuals with a wide range of ability levels.
Acknowledgments:
The authors gratefully acknowledge all study participants and the team at Lead Pilates and Integrative Therapies.
References
Latimer-Cheung AE, Martin Ginis KA, Hicks AL, et al. Development of evidence-informed physical activity guidelines for adults with multiple sclerosis. Arch Phys Med Rehabil. 2013;94:1829–1836.e7.
Motl RW, Pilutti LA. The benefits of exercise training in multiple sclerosis. Nat Rev Neurol. 2012;8:487–497.
Rietberg MB, Brooks D, Uitdehaag BM, Kwakkel G. Exercise therapy for multiple sclerosis. Cochrane Database Syst Rev. 2005;1:CD003980.
Fox EE, Hough AD, Creanor S, Gear M, Freeman JA. Effects of Pilates-based core stability training in ambulant people with multiple sclerosis: multicenter, assessor-blinded, randomized controlled trial. Phys Ther. 2016;96:1170–1178.
Lanzetta D, Cattaneo D, Pellegatta D, Cardini R. Trunk control in unstable sitting posture during functional activities in healthy subjects and patients with multiple sclerosis. Arch Phys Med Rehabil. 2004;85:279–283.
Guclu-Gunduz A, Citaker S, Irkec C, Nazliel B, Batur-Caglayan HZ. The effects of Pilates on balance, mobility and strength in patients with multiple sclerosis. NeuroRehabilitation. 2014;34:337–342.
Kalron A, Rosenblum U, Frid L, Achiron A. Pilates exercise training vs. physical therapy for improving walking and balance in people with multiple sclerosis: a randomized controlled trial. Clin Rehabil. 2017;31:319–328.
Marandi SM, Nejad VS, Shanazari Z, Zolaktaf V. A comparison of 12 weeks of Pilates and aquatic training on the dynamic balance of women with mulitple sclerosis. Int J Prev Med. 2013;4(suppl 1):110S–117S.
Tomruk MS, Uz MZ, Kara B, Idiman E. Effects of Pilates exercises on sensory interaction, postural control and fatigue in patients with multiple sclerosis. Mult Scler Relat Disord. 2016;7:70–73.
van der Linden ML, Bulley C, Geneen LJ, Hooper JE, Cowan P, Mercer TH. Pilates for people with multiple sclerosis who use a wheelchair: feasibility, efficacy and participant experiences. Disabil Rehabil. 2014;36:932–939.
Freeman JA, Gear M, Pauli A, et al. The effect of core stability training on balance and mobility in ambulant individuals with multiple sclerosis: a multi-centre series of single case studies. Mult Scler. 2010;16:1377–1384.
Skurvydas A, Brazaitis M, Andrejeva J, Mickeviciene D, Streckis V. The effect of multiple sclerosis and gender on central and peripheral fatigue during 2-min MVC. Clin Neurophysiol. 2011;122:767–776.
Rice CL, Vollmer TL, Bigland-Ritchie B. Neuromuscular responses of patients with multiple sclerosis. Muscle Nerve. 1992;15:1123–1132.
Canadian Society for Exercise Physiology. Canadian physical activity guidelines for adults with multiple sclerosis. http://www.csep.ca/CMFiles/Guidelines/specialpops/CSEP_MS_PAGuidelines_adults_en.pdf. Accessed July 13, 2017.
Bullo V, Bergamin M, Gobbo S, et al. The effects of Pilates exercise training on physical fitness and wellbeing in the elderly: a systematic review for future exercise prescription. Prev Med. 2015;75:1–11.
Warburton DER, Jamnik VK, Bredin SSD, Gledhill N. The ePARmed-X+ physician clearance follow-up. Health Fit J Canada. 2014;7:35–38.
Finch P, Bessonnette S. A pragmatic investigation into the effects of massage therapy on the self efficacy of multiple sclerosis clients. J Bodyw Mov Ther. 2014;18:11–16.
ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the Six-Minute Walk test. Am J Respir Crit Care Med. 2002;166:111–117.
Sebastiao E, Sandroff BM, Learmonth YC, Motl RW. Validity of the Timed Up and Go test as a measure of functional mobility in persons with multiple sclerosis. Arch Phys Med Rehabil. 2016;97:1072–1077.
Rose DJ, Lucchese N, Wiersma LD. Development of a multidimensional balance scale for use with functionally independent older adults. Arch Phys Med Rehabil. 2006;87:1478–1485.
Chilibeck PD, Vatanparast H, Pierson R, et al. Effect of exercise training combined with isoflavone supplementation on bone and lipids in postmenopausal women: a randomized clinical trial. J Bone Miner Res. 2013;28:780–793.
Strand SL, Hjelm J, Shoepe TC, Fajardo MA. Norms for an isometric muscle endurance test. J Hum Kinet. 2014;40:93–102.
Kayes NM, Schluter PJ, McPherson KM, Leete M, Mawston G, Taylor D. Exploring Actical accelerometers as an objective measure of physical activity in people with multiple sclerosis. Arch Phys Med Rehabil. 2009;90:594–601.
Vickrey BG, Hays RD, Harooni R, Myers LW, Ellison GW. A health-related quality of life measure for multiple sclerosis. Qual Life Res. 1995;4:187–206.
Learmonth YC, Dlugonski DD, Pilutti LA, Sandroff BM, Motl RW. The reliability, precision and clinically meaningful change of walking assessments in multiple sclerosis. Mult Scler. 2013;19:1784–1791.
Frank-Wilson AW, Farthing JP, Chilibeck PD, et al. Lower leg muscle density is independently associated with fall status in community-dwelling older adults. Osteoporos Int. 2016;27:2231–2240.
Shirani A, Zhao Y, Karim ME, et al. Association between use of interferon beta and progression of disability in patients with relapsing-remitting multiple sclerosis. JAMA. 2012;308:247–256.
Trojano M, Pellegrini F, Fuiani A, et al. New natural history of interferon-beta-treated relapsing multiple sclerosis. Ann Neurol. 2007;61:300–306.
Tedeholm H, Lycke J, Skoog B, et al. Time to secondary progression in patients with multiple sclerosis who were treated with first generation immunomodulating drugs. Mult Scler. 2013;19:765–774.
Yousry TA, Major EO, Ryschkewitsch C, et al. Evaluation of patients treated with natalizumab for progressive multifocal leukoencephalopathy. N Engl J Med. 2006;354:924–933.
Polman C, Killestein J, Rudick R. Natalizumab to treat multiple sclerosis. In: Cohen J, Rudick R, eds. Multiple Sclerosis Therapeutics. 4th ed. Cambridge, UK: Cambridge University Press; 2011:330–343.
Clifford DB, DeLuca A, Simpson DM, Arendt G, Giovannoni G, Nath A. Natalizumab-associated progressive multifocal leukoencephalopathy in patients with multiple sclerosis: lessons from 28 cases. Lancet. 2010;9:438–446.
Health Canada. Gilenya (fingolimod): stronger safety recommendations regarding first-dose heart monitoring and use in patients with heart conditions: for the public. http://healthycanadians.gc.ca/recall-alert-rappel-avis/hc-sc/2012/14795a-eng.php. Published August 23, 2012. Accessed July 19, 2017.
US Food and Drug Administration. FDA Drug Safety Communication: revised recommendations for cardiovascular monitoring and the use of multiple sclerosis drug Gilenya (fingolimod). http://www.fda.gov/Drugs/DrugSafety/ucm303192.htm. Accessed July 19, 2017.
Government of Canada. TECFIDERA (dimethyl fumarate): risk of rare brain condition known as progressive multifocal leukoencephalopathy (PML): for the public. http://healthycanadians.gc.ca/recall-alert-rappel-avis/hc-sc/2015/43627a-eng.php. Published February 6, 2015. Accessed July 19, 2017.
Goldman MD, Marrie RA, Cohen JA. Evaluation of the six-minute walk in multiple sclerosis subjects and healthy controls. Mult Scler. 2008;14:383–390.
Baert I, Freeman J, Smedal T, et al. Responsiveness and clinically meaningful improvement, according to disability level, of five walking measures after rehabilitation in multiple sclerosis: a European multicenter study. Neurorehabil Neural Repair. 2014;28:621–631.
Paltamaa J, West H, Sarasoja T, Wikstrom J, Malkia E. Reliability of physical functioning measures in ambulatory subjects with MS. Physiother Res Int. 2005;10:93–109.
Stuifbergen AK, Blozis SA, Harrison TC, Becker HA. Exercise, functional limitations, and quality of life: a longitudinal study of persons with multiple sclerosis. Arch Phys Med Rehabil. 2006;87:935–943.







