Publication
Research Article
International Journal of MS Care
Effect of Functional Electrical Stimulation Cycling Exercise on Lower Limb Strength Asymmetry in Persons With Multiple Sclerosis
Abstract
Background:
Lower limb strength asymmetry (ie, significant difference between contralateral limbs) has been associated with mobility impairment in persons with multiple sclerosis (MS). However, whether an adaptive exercise modality can be used to modify lower limb strength and potentially improve mobility is unclear. The effect of functional electrical stimulation (FES) cycling on lower limb strength asymmetry in persons with MS with mobility impairment was assessed, and the association between change in lower limb strength asymmetries and changes in functional and self-reported mobility outcomes was explored.
Methods:
Eight adults with MS (Expanded Disability Status Scale scores, 5.5–6.5) were included. Outcomes included knee extensor and knee flexor strength asymmetry, Timed 25-Foot Walk (T25FW) test, 2-Minute Walk Test (2MWT), Timed Up and Go (TUG) test, and 12-item Multiple Sclerosis Walking Scale (MSWS-12). Participants received 24 weeks (3 times per week) of FES cycling or passive leg cycling.
Results:
The FES condition demonstrated a small decrease in knee extensor (d = −0.33) and knee flexor (d = −0.23) strength asymmetry compared with passive leg cycling. With both groups combined, weak-to-strong associations were observed between change in knee extensor asymmetry and change in T25FW test time (rs = −0.43), 2MWT time (rs = −0.24), TUG test time (rs = 0.55), and MSWS-12 score (rs = 0.43). Moderate correlations were observed between change in knee flexor asymmetry and change in T25FW test time (rs = −0.31), TUG test time (rs = 0.33), and MSWS-12 score (rs = 0.35).
Conclusions:
FES cycling may be an efficacious exercise modality for reducing lower limb strength asymmetry and improving mobility in persons with MS.
A symmetries in lower limb strength (ie, differences greater than or equal to 10% between contralateral muscle groups) are common in persons with multiple sclerosis (MS) and increase with disability progression.1 A previous review reported lower limb strength asymmetry values ranging from 10% to 38% in persons with MS, and significant associations between strength asymmetries and mobility and postural outcomes.2 These findings suggest that interventions such as exercise training might target lower limb strength asymmetry for reducing mobility impairment in persons with MS with increasing levels of disability.
Persons with MS who experience mobility impairment often require specialized or adapted strategies for exercise training, such as functional electrical stimulation (FES) cycling, which uses systematic electrical stimulation delivered to lower extremity muscle groups to produce leg cycling movement. Exercise rehabilitation with FES has been reported to be a promising approach for persons with MS with mobility impairment (Expanded Disability Status Scale [EDSS] scores of 6.0–7.5).3 A recent pilot randomized controlled trial by our research group provided evidence for the feasibility and preliminary efficacy of 24 weeks of FES cycling exercise in persons with MS (EDSS range, 5.5–6.5)4; small to moderate improvements in mobility and fitness outcomes, including lower limb strength, were reported.
The present analysis examined the efficacy of 24 weeks of FES cycling exercise on lower limb strength and cycling asymmetries and explored potential associations between changes in lower limb asymmetry and mobility with FES cycling.
Methods
The present study is a secondary analysis of a pilot randomized controlled trial of FES cycling exercise in persons with MS with mobility impairment.4 The present study was in compliance with the standards of the Declaration of Helsinki, with all procedures approved by the University of Illinois at Urbana-Champaign Institutional Review Board; all participants provided written informed consent before participation. The detailed protocol and recruitment procedures have previously been described.5 Outcome measures relevant to the present analysis were collected by blinded assessors and included muscular strength asymmetry of the knee extensors and knee flexors, asymmetry in force production during the cycling sessions, and change in walking speed, endurance, dynamic balance, and patient-reported MS walking impairment. Muscular strength was assessed bilaterally for the knee extensors and knee flexors using an isokinetic dynamometer (Biodex Medical Systems Inc). With the knee flexed at 60°, participants performed three 5-second maximal isometric contractions of the knee extensors and knee flexors, with a 5-second rest period between contractions.4 The highest peak torque value for both muscle groups was recorded and used to calculate asymmetry scores using the following equation: [1 − (limb strengthweaker/limb strengthstronger)] × 100, with higher scores reflecting greater differences between contralateral limbs.1 Walking speed, endurance, and dynamic balance were assessed using the Timed 25-Foot Walk (T25FW) test, the 2-Minute Walk Test (2MWT), and the Timed Up and Go (TUG) test using standardized testing protocols.5 Patient-reported walking was assessed using the 12-item Multiple Sclerosis Walking Scale (MSWS-12).5 , 6
Participants were randomly assigned to undergo 24 weeks (3 times per week) of either supervised FES cycling or passive leg cycling using RT300 cycles (Restorative Therapies Inc). The specific training parameters are reported elsewhere and are based on previous studies of FES cycling in persons with MS.3 , 4 The FES cycling group received electrical stimulation to the quadriceps, hamstring, and gluteal muscle groups while actively pedaling at a prescribed target heart rate and a cadence of 50 rpm. The FES stimulation parameters were set as symmetrical biphasic waveforms with a 250-μs phase duration and a pulse rate of 50 pulses per second. Stimulation intensity was set and adjusted based on the participant’s sensory tolerance for each muscle group with the goal of maintaining the target heart rate and cadence for the entire session. The passive leg cycling condition was identical to the FES cycling condition except that participants did not receive electrical stimulation and leg movement was motor-driven, resulting in a symmetrical movement pattern. The FES cycling condition received motor assistance only when cycling cadence dropped below 50 rpm. The average force produced by each limb during cycling sessions yielded asymmetry scores for cycling force, using the same calculation as lower limb strength asymmetry.1
Data analysis was performed using SPSS Statistics for Windows, version 25.0 (IBM Corp). Group data are expressed as mean ± SD, unless otherwise specified. Due to the size of the sample, the efficacy of the intervention for reducing asymmetry was examined as mean absolute differences and mean percentage change between groups over time, as well as effect sizes, expressed as Cohen d. Effect sizes of 0.2, 0.5, and 0.8 were interpreted as small, moderate, and large differences, respectively.7 Cycling force asymmetry was analyzed as change over time in the FES condition only because leg movement in the passive leg cycling condition was motor-driven and set to follow a symmetrical pattern. The association between change in asymmetry and change in mobility was explored using Spearman correlations (rs). Correlation coefficients of 0.1, 0.3, and 0.5 were interpreted as weak, moderate, and strong, respectively.7
Results
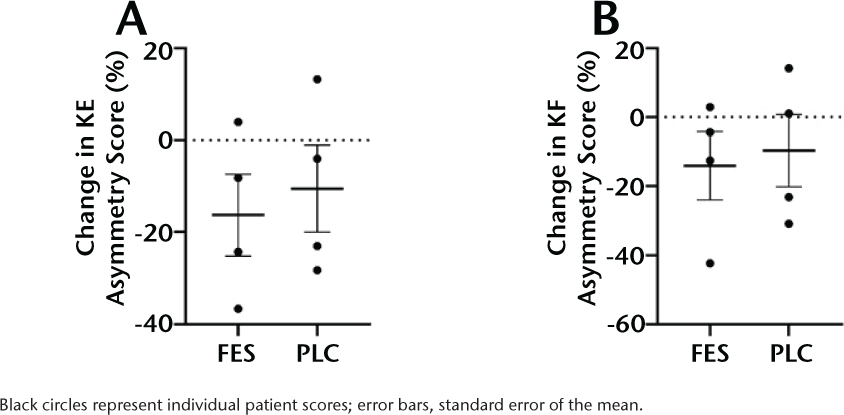
The FES and passive leg cycling groups each included 4 adults with MS (3 and 4 women, respectively). The mean ± SD age, height, and weight of persons in the FES cycling condition were 57.3 ± 6.0 years, 161.1 ± 10.4 cm, and 70.6 ± 19.5 kg, respectively, and those of persons in the passive leg cycling condition were 48.5 ± 7.7 years, 160.5 ± 9.2 cm, and 85.8 ± 46.0 kg, respectively. Median (interquartile range) EDSS scores for the FES and passive leg cycling conditions were 6.3 (0.5) and 6.3 (0.9), respectively. No significant differences were observed between groups at baseline in demographic and clinical data.4 Full clinical and demographic characteristics are reported elsewhere.4 The FES cycling condition demonstrated a small decrease in knee extensor strength asymmetry (5.9% mean absolute difference between groups, 4.6% mean percentage change over time between groups, d = −0.33) and knee flexor strength asymmetry (4.4%, 5.4%, d = −0.23) compared with the passive leg cycling condition after 24 weeks (Figure 1). Of note, both groups demonstrated an improvement in strength asymmetry after the intervention; however, the magnitude of the effect was larger in the FES cycling condition. There was no change in mean ± SD cycling force asymmetry in the FES cycling condition over time (pre: 12.5% ± 16.8% vs post: 12.0% ± 18.7%, d = −0.03).
Mean Change in Knee Extensor (KE) (A) and Knee Flexor (KF) (B) Strength Asymmetry Scores for the Functional Electrical Stimulation (FES) Cycling and Passive Leg Cycling (PLC) Conditions
Strong correlation coefficients were observed between change in knee extensor strength asymmetry and change in TUG test times (rs = 0.55). Moderate correlation coefficients were observed between change in knee extensor strength asymmetry and changes in T25FW test times (rs = −0.43) and MSWS-12 scores (rs = 0.43), and between change in knee flexor strength asymmetry and changes in T25FW test times (rs = −0.31), TUG test times (rs = 0.33), and MSWS-12 scores (rs = 0.35). Weak correlation coefficients were observed between change in knee extensor strength asymmetry and change in 2MWT time (rs = −0.24), and there was no association between change in knee flexor strength asymmetry and change in 2MWT time (rs = −0.07).
Discussion
The present study provides new evidence regarding the efficacy of FES cycling exercise for reducing lower limb strength asymmetries in persons with MS with mobility impairment. In addition, weak-to-strong associations were observed between reductions in lower limb strength asymmetries and improvements in mobility outcomes.
Previous studies of FES cycling in persons with MS have reported improvements in lower limb strength that may be attributed to greater motor unit recruitment and muscle activation induced by superficial stimulation during training.3 , 8 The observed reduction in both knee extensor and knee flexor strength asymmetry may similarly be due to additional muscle activation, as well as the unilateral nature of the FES cycle that allows the limbs to receive stimulation and produce force independently. Unilateral training has previously been incorporated in resistance training protocols for persons with MS and has been reported to be effective for improving muscular strength in unimpaired and impaired limbs.8 Of note, our research group observed a reduction in strength asymmetry in the passive leg cycling condition despite a lack of change in overall strength.4 In persons who have experienced a stroke, passive leg cycling has been reported to activate somatosensory receptors and generate ascending inputs to the central nervous system, resulting in a similar cortical activation pattern as active cycling, as well as improved motor performance.9 The observed improvement in lower limb strength asymmetry, independent of change in strength in the passive leg cycling condition, may be explained by increased cortical activation induced by performing passive movement in a repetitive, symmetrical pattern during the training sessions.
We did not observe a change in cycling force asymmetry in the FES cycling condition after the intervention, which may be attributed to a lack of focus on cycling symmetry during training. Participants in the present study were not instructed to attempt to reduce force asymmetry while cycling; however, the visual display panel on the FES cycle continually presents a measure of force asymmetry during cycling. Incorporating visual feedback with participant instruction to produce symmetrical movement has been an effective strategy for reducing asymmetries during cycling in persons with neurologic disorders.10 Future studies with FES cycling in persons with MS should investigate whether providing instruction to target asymmetry during cycling results in more symmetrical movement long-term. Functional electrical stimulation cycling with visual feedback is ideally positioned to target and reduce cycling asymmetry during training.
Greater asymmetry in lower limb strength has been associated with reduced walking speed and endurance in persons with MS.2 The present study observed weak to moderate inverse associations between changes in lower limb strength asymmetry and changes in T25FW and 2MWT times, whereas moderate to strong positive associations were observed with change in TUG test times and MSWS-12 scores. An increase in muscular strength of the impaired limb after training may potentially have resulted in greater propulsive forces generated during walking and thus contributed to improvements in mobility outcomes. These findings suggest that future rehabilitation programs aiming to improve mobility in persons with MS may consider incorporating exercise training that targets lower limb strength asymmetry.
The size and characteristics of this sample limit the generalizability of the study findings. Participants were not preselected for inclusion based on the outcomes herein because these were not the primary outcomes of the trial. The asymmetry scores observed in the present investigation are greater than those previously reported and may reflect the higher EDSS scores of the present sample.2 Electrical stimulation was prescribed and adjusted per muscle group; however, lower limb asymmetries were not intentionally targeted for correction during the intervention.
The present study provides preliminary evidence regarding: (1) the efficacy of FES cycling exercise for modifying lower limb strength asymmetry in persons with MS with mobility impairment; and (2) the potential relationship between strength asymmetry and mobility in response to FES cycling exercise. Future investigations with larger sample sizes might explore optimal FES cycling prescription parameters (ie, frequency, intensity, duration, and stimulation parameters) as well as the efficacy of remote or home-based FES exercise delivery. In addition, future investigations to examine the efficacy of exercise training programs that specifically target and reduce lower limb strength asymmetry for improving mobility in persons with MS are needed.
PRACTICE POINTS
Functional electrical stimulation cycling exercise may be an efficacious modality for modifying lower limb strength asymmetry in persons with MS with mobility impairment.
Rehabilitation programs aiming to improve mobility in persons with MS may consider incorporating exercise training that targets lower limb strength asymmetry for modification.
References
Sandroff BM, Pilutti LA, Benedict RHB, Motl RW. Association between physical fitness and cognitive function in multiple sclerosis: does disability status matter? Neurorehabil Neural Repair . 2015; 29: 214– 223.
Rudroff T, Proessl F. Effects of muscle function and limb loading asymmetries on gait and balance in people with multiple sclerosis. Front Physiol. 2018; 9: 531.
Pilutti LA, Motl RW. Functional electrical stimulation cycling exercise for people with multiple sclerosis. Curr Treat Options Neurol. 2019; 21: 54.
Edwards T, Motl RW, Sebastião E, Pilutti LA. Pilot randomized controlled trial of functional electrical stimulation cycling exercise in people with multiple sclerosis with mobility disability. Mult Scler Relat Disord. 2018; 26: 103– 111.
Pilutti LA, Motl RW, Edwards TA, Wilund KR. Rationale and design of a randomized controlled clinical trial of functional electrical stimulation cycling in persons with severe multiple sclerosis. Contemp Clin Trials Commun. 2016; 3: 147– 152.
Hobart JC, Riazi A, Lamping DL, Fitzpatrick R, Thompson AJ. Measuring the impact of MS on walking ability: the 12-Item MS Walking Scale (MSWS-12). Neurology. 2003; 60: 31– 36.
Cohen J. Statistical Power Analysis for the Behavioural Sciences. 2nd ed. Lawrence Erlbaum Associates; 1988.
Broekmans T, Roelants M, Feys P, . Effects of long-term resistance training and simultaneous electro-stimulation on muscle strength and functional mobility in multiple sclerosis. Mult Scler. 2011; 17: 468– 477.
Lin P-Y, Chen J-JJ, Lin S-I. The cortical control of cycling exercise in stroke patients: An fNIRS study. Human Brain Mapp. 2013; 34: 2381– 2390.
Ambrosini E, Ferrante S, Pedrocchi A, Ferrigno G, Guanziroli E, Molteni F. A novel biofeedback cycling training to improve gait symmetry in stroke patients: a case series study. IEEE Int Conf Rehabil Robot. 2011; 2011: 5975495.
Financial Disclosures: The authors declare no conflicts of interest.
Funding/Support: This work was supported, in part, by the National Multiple Sclerosis Society (grant PR-1411-0209), the Consortium of Multiple Sclerosis Centers (CMSC), and the Multiple Sclerosis Society of Canada (grant EGID 2665).
Prior Presentation: This analysis has been published as a platform presentation/conference abstract for the 2020 CMSC Annual Meeting (virtual).







