Publication
Research Article
International Journal of MS Care
Case Report: Combining Dalfampridine with Multicomponent Exercise and Gait Training in a Person with Multiple Sclerosis
Author(s):
Abstract
Background:
Dalfampridine extended release (D-ER) improves gait speed in some people with multiple sclerosis (MS), but many patients who take D-ER demonstrate only small improvements of questionable clinical significance. Physical therapy (PT) may augment the treatment effects of D-ER on the nervous system and improve clinical outcomes. This case report describes the successful use of D-ER combined with multicomponent PT in a patient who did not have a clinically important change in gait speed with D-ER alone.
Methods:
A 59-year-old woman with a 6-year history of relapsing-remitting MS was prescribed D-ER by her neurologist. After 3 weeks of D-ER therapy (10 mg twice daily), she demonstrated only a 7.1% improvement in the Timed 25-Foot Walk test. She then commenced PT consisting of two 40-minute sessions per week for 6 weeks while continuing D-ER therapy. Training focused on gait, balance, coordination, functional strengthening, and dual-task performance.
Results:
After 6 weeks of D-ER + PT, she had a further 14.6% improvement in Timed 25-Foot Walk gait speed, for a total improvement of 20.7%, which elevated her above the clinically meaningful threshold of 20%. Similar patterns of improvement were also observed for self-selected gait speed in single- and dual-task conditions. Improvements in fast and dual-task gait speed were retained 3 weeks later.
Conclusions:
For this patient, combining PT with D-ER therapy improved gait speed more than the use of D-ER alone. Further investigation of D-ER + PT or PT as an alternative to D-ER in patients with submeaningful medication response is warranted.
Oral dalfampridine extended release (D-ER; Ampyra, Acorda Therapeutics Inc, Ardsley, NY) is a leading treatment for gait impairments in people with multiple sclerosis (MS). Oral D-ER can substantially improve gait speed within 2 to 6 weeks of starting the medication.1,2 Unfortunately, pooled results from two phase 3 clinical trials demonstrated that a clinically meaningful improvement is observed in only 33% of all people who take D-ER.3 A clinically meaningful improvement is defined by at least 20% improvement in gait speed on the Timed 25-Foot Walk (T25FW) test.4 The “responder” rate is slightly higher (38%) when responders are defined as patients with faster walking speed for at least three of the four on-treatment visits compared with the maximum off-drug T25FW gait speed.3 Responders average 25% improvement in T25FW gait speed, whereas the average change in nonresponders is only 7%.3
Exercise and gait training interventions may be an excellent alternative or adjunct treatment for patients who do not respond meaningfully to D-ER alone. Two meta-analyses5,6 and three systematic reviews7–9 provide evidence that both exercise and task-specific gait training interventions can improve walking ability in people with MS. It is unclear whether one form of gait training is superior to other approaches10; however, conventional physical therapy (PT) typically includes both functional strength training and task-specific gait training to improve gait limitations in MS. It is possible that the treatment effects of D-ER may be enhanced by combining the medication with a progressive exercise and gait training program, especially because it is not presently known why some patients respond meaningfully to D-ER and others do not. In this case report, we describe the successful use of D-ER combined with a multicomponent exercise and gait training PT program in a patient with MS who did not demonstrate a clinically meaningful change in T25FW gait speed on D-ER alone.
Methods
Participant Description
The participant was a 59-year-old woman with a 6-year history of relapsing-remitting MS who was experiencing gait impairments and had been prescribed D-ER by her neurologist. Her Expanded Disability Status Scale score was 3.0. She had lower extremity weakness and impaired proprioception. Although she had fallen only once in the previous 12 months, she admitted that she purposely avoided stairs without a handrail due to fear of falling. Her self-rated balance self-efficacy on the Activities-specific Balance Confidence scale was 68%. She was 0% confident that she could maintain her balance during stair ascent or descent (no handrail). Her baseline T25FW time was 6.61 seconds, which is noteworthy because a T25FW time greater than 6 but less than 8 seconds is associated with some occupational disability and possible limitations in instrumental activities of daily living.11
Procedures
Study procedures were approved by The University of North Carolina institutional review board (Chapel Hill, NC), and the participant provided informed consent. The patient was participating in a pilot study in which D-ER + PT was being compared with PT without D-ER. The patient in this case report was the first patient in the D-ER + PT group. The participant was initially assessed before she commenced D-ER (ie, off-drug baseline). She was reassessed after 3 weeks of D-ER use to evaluate her response to the medication. The participant then commenced a PT program twice per week for 6 weeks. She was reassessed after the 6-week combined D-ER + PT intervention, with a follow-up assessment 3 weeks later to assess retention of treatment effects.
Interventions
The D-ER was taken as prescribed in 10-mg doses twice per day. Physical therapy consisted of a multicomponent exercise and gait training program involving a progressive sequence of training activities (Table 1) focusing on gait, balance, lower extremity coordination, functional strengthening, and dual-task performance. Each 40-minute training session comprised 10 minutes of part-task training, 20 minutes of whole-task practice, and 10 minutes of contextual transfer activities. Part-task practice included step practice (eg, swing kinematics), as well as balance, lower extremity coordination, and functional strengthening exercises. Whole-task practice involved continuous walking, alternating every other session between overground and treadmill gait training. Contextual transfer practice was conducted overground in the real world and included activities such as walking outdoors and negotiating different surfaces and obstacles (stationary and moving). Handheld support for any activity was rarely permitted, unless the principal purpose of the activity was to maximize repetitions for strengthening. If a task could not be performed at all without handheld support it was modified so that the participant was trained to become less reliant on using her arms to maintain or regain balance. Otherwise, she was given encouragement and feedback and was educated about why it was important to challenge her balance in this way.
Exercise and gait training activities
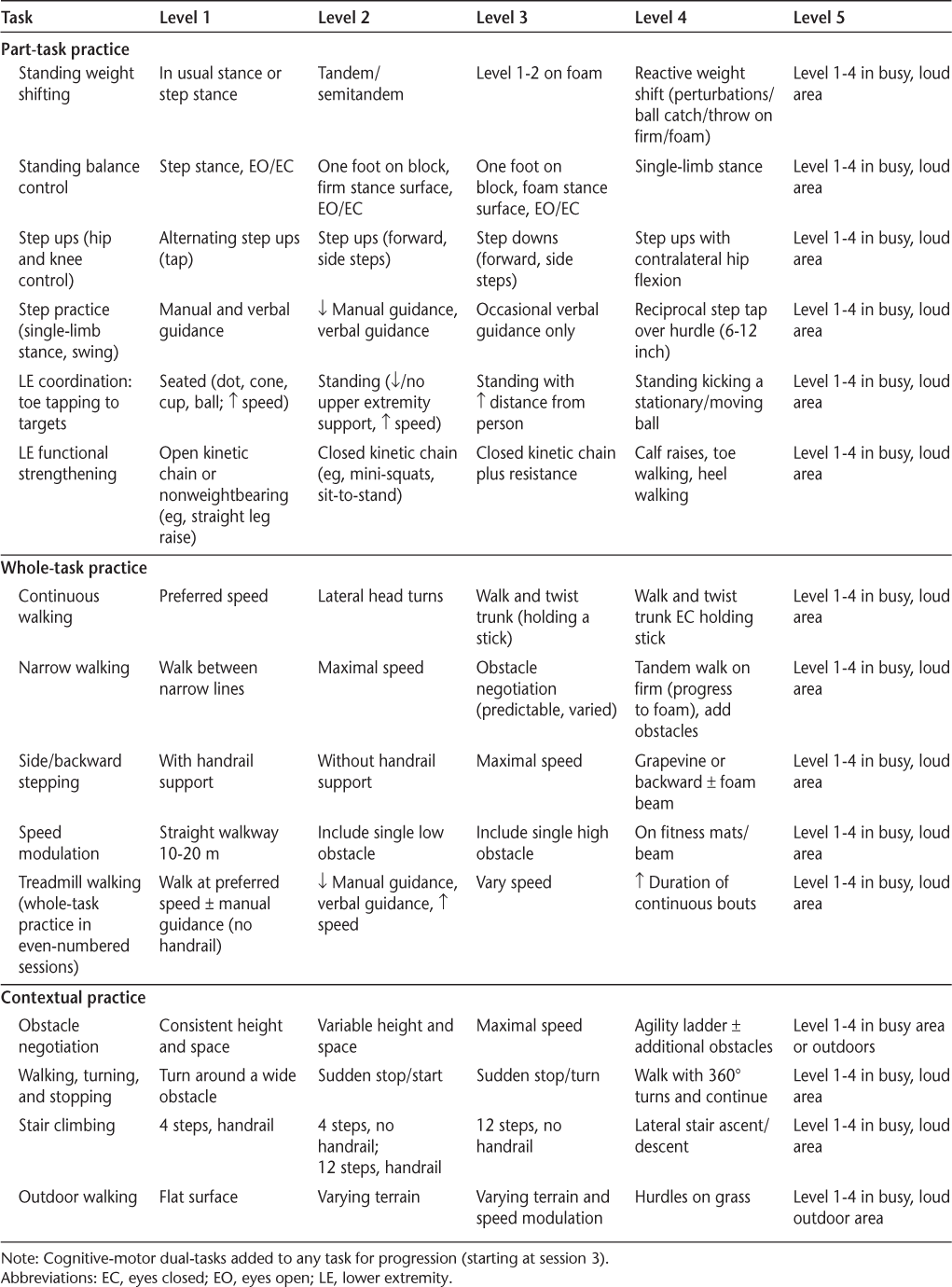
During treadmill walking, the participant wore a safety harness that did not provide any body weight support. The participant occasionally grabbed the handrails to regain balance but was compliant with not holding the handrails at other times. Manual assistance was provided as needed (eg, to facilitate increased step length); however, she was responsive to verbal cueing to make adjustments to her gait pattern. Treadmill speed and duration of walking bouts were adjusted according to her individual ability and fatigue, but speed, endurance, and independence (reduced manual assistance and verbal cueing from the therapist and reduced reliance on handrails for reactive postural adjustments) were progressed in each session. The challenge point framework was applied to all training activities to ensure an optimal level of task difficulty for motor learning.12
Dual-task training was also incorporated in sessions 3 to 12 as part of the gait training intervention (whole-task practice), and to increase functional difficulty during part-task practice and contextual transfer activities as appropriate. Ten different tasks were used to involve a range of cognitive functions (working memory, executive function, visuospatial processing, and language) during dual-task training. Cognitive tasks were progressed based on the individual's performance and the progression of gait activities.
Outcome Measures
In this report, we focus primarily on gait speed outcomes: fast, usual, and dual-task gait speeds. The T25FW test, which is a measure of “fastest safe” gait speed, provides a direct comparison with the D-ER clinical trials. The average of two trials was used at each assessment visit. Self-selected (usual) and dual-task gait speeds were measured using a 20-foot instrumented walkway (Protokinetics, Havertown, PA). The participant completed four continuous passes over the walkway for each task, with turns completed off the walkway so that only steady-state strides were captured for analysis. The dual-task involved walking with simultaneous performance of the clock task,13 which requires the participant to respond to an auditory stimulus (eg, “one twenty-five”) with “yes” or “no” based on whether the hands of the clock are in the same (left/right) half of the clock at the given time. Given the participant's fear of falling, particularly during stair climbing, we also report changes in the Activities-specific Balance Confidence scale overall and the stair ascent/descent item.
Results
Feasibility and tolerance of the intervention were demonstrated by participant attendance at all 12 PT sessions within 6 weeks, despite commuting more than 75 miles each way. She also reported adhering to her D-ER medication throughout the study period. No adverse events or medication adverse effects were reported. Treadmill walking was well tolerated. We believe that not permitting use of the handrails for stability during treadmill walking was critical in training her reactive balance control and confidence. Indeed, the patient reported that she had never previously walked on a treadmill without holding on and believed this to be a “huge help.” Treadmill speeds began at 0.5 to 0.6 m/s in the first treadmill session and were between 1.0 and 1.2 m/s in the last treadmill session. As she progressed, treadmill speed was varied to promote gait adaptability.
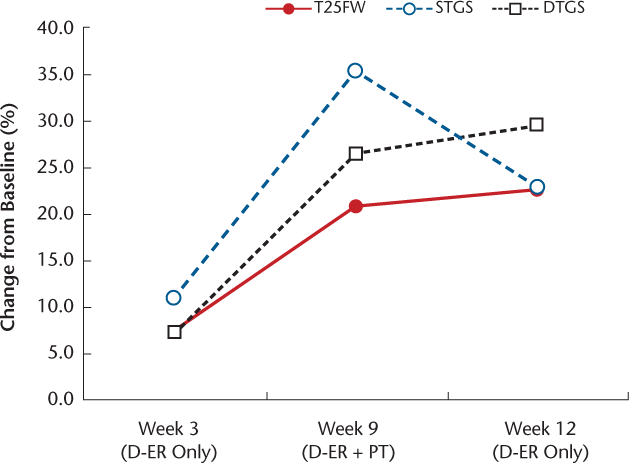
The participant demonstrated a 7.1% improvement in T25FW time after 3 weeks of taking D-ER, which does not exceed the 20% clinically meaningful threshold. Importantly, her T25FW time was also still greater than the 6-second benchmark associated with occupational and everyday-activity limitations.11 After 6 weeks of D-ER + PT, she had a further 14.7% improvement in T25FW time, for a total improvement of 20.7%, which elevated her above the clinically significant threshold of 20% and dropped her below the 6-second benchmark (Figure 1 and Table 2). Similar treatment responses were observed for both single-task and dual-task gait speed. Specifically, small improvements were observed after the 3-week D-ER run in (10.7% and 7.1%, respectively), with substantially greater improvements after the combined D-ER + PT phase (22.2% and 26.0%, respectively), for total improvement from baseline of 35.3% for single-task gait speed and 26.6% for dual-task gait speed. Improvements in fast and dual-task gait speed were retained at 3-week follow-up.
Percentage change from baseline (week 0) at each visit for Timed 25-Foot Walk test (T25FW), single-task gait speed (STGS), and dual-task gait speed (DTGS)
Performance on gait speed outcome measures and balance confidence at each time point
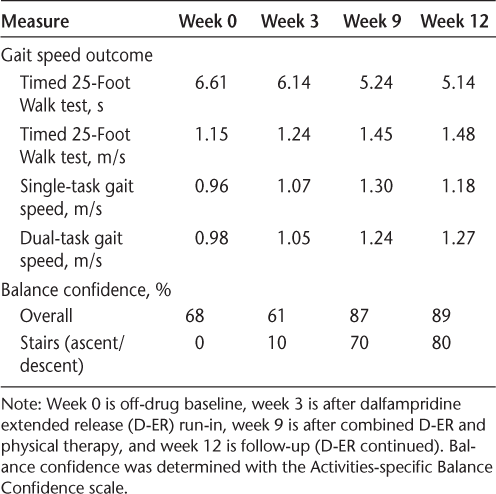
The participant's balance self-efficacy on stairs improved from 0% to 10% on D-ER alone but increased to 70% after combined D-ER + PT and improved slightly further in the 3-week follow-up period to 80%. Her overall balance self-efficacy scores declined 7% during the D-ER run-in but improved substantially (26%) in the D-ER + PT phase, with retention of improvement in balance confidence at follow-up (Table 2).
Discussion
The participant in this report had only 7% improvement in T25FW gait speed after 3 weeks of D-ER therapy, which is consistent with the results for nonresponders in the phase 3 clinical trials.3 We showed that providing a progressive, multicomponent PT program customized to continuously challenge the individual's ability in balance, gait, strength, and coordination, concurrently with prescribed D-ER, helped this participant achieve clinically meaningful improvements in T25FW gait speed that were not evident from D-ER alone. Importantly, the improvements in her T25FW (fast) gait speed translated to her habitual gait speed with and without cognitive distraction.
The gait speed improvements we observed with this combined intervention also exceed those that have been reported for exercise and gait training interventions in people with MS.5,14 For example, a pooled analysis of task-specific gait training interventions in people with MS found an overall improvement in self-selected gait speed of 0.06 (95% CI, 0.02–0.10) m/s,14 whereas the participant in this study had a 0.23-m/s increase in self-selected gait speed during the D-ER + PT phase. A meta-analysis of exercise interventions found only a small, nonsignificant improvement in T25FW time (−0.59 [95% CI, −2.55 to 1.36] seconds),5 whereas our participant improved T25FW time by 0.90 seconds with the combined intervention. Thus, this report provides promising preliminary evidence that combining a progressive and challenging multidimensional PT intervention with D-ER therapy can considerably improve the response to treatment in someone who has not responded meaningfully to D-ER alone and that the treatment effects of PT may be augmented by D-ER.
Although this patient had relatively minor disability according to the Expanded Disability Status Scale score, she was severely restricted by a fear of falling and low balance-related confidence during everyday activities. This may have caused her to slow her gait speed and would not be improved by D-ER but could be addressed by PT. Indeed, for a person whose activities are limited by factors beyond primary impairments in motor control, a challenging and progressive balance and gait training program may be an instrumental adjunct to maximize treatment effects of D-ER on mobility.
There are several reasons we believe this PT intervention to be particularly robust. Unlike most exercise and rehabilitation studies to date, which tend to focus on one particular type of training (eg, treadmill-based gait training or progressive resistance training in isolation), we incorporated a multicomponent intervention that included activities focusing on functional strengthening as well as gait, balance, and coordination. Moreover, many of the treatment activities simultaneously targeted multiple functions (eg, standing toe tapping incorporates hip strengthening, lower extremity coordination, and balance control when performed without any upper extremity support). Not permitting handheld support during activities was critical to maximizing the level of challenge and reducing reliance on arm support for dynamic balance and postural corrections. Due to the clinical decision making needed to constantly evaluate and advance (or modify) the challenge level, we consider this program of PT to be a skilled therapy that requires administration by a health care provider who has the capability to continuously observe and manipulate the practice conditions to ensure that task difficulty is appropriately matched to the changing skill level of the learner, which is needed to optimize motor learning. Given the high level of balance challenge prescribed, the need for guarding to ensure safety means that this particular PT program may not be amenable to a group format. This PT intervention is no more labor intensive than other one-on-one PT and uses commonly accessible clinic equipment (eg, a basic treadmill), so it is highly generalizable.
In conclusion, the findings from this report suggest that further investigation of the combination of PT and D-ER therapy in people with MS is warranted, as well as examination of whether PT (without D-ER) is an effective alternative to D-ER therapy in those who do not experience clinically meaningful improvements on the medication alone. The multicomponent exercise and gait training program used in this study may be a robust model for PT intervention and should be examined against previously established efficacious treatments.
PRACTICE POINTS
Combining a multicomponent exercise and gait training intervention with dalfampridine therapy may enable dalfampridine nonresponders to achieve clinically meaningful changes in gait speed.
Combined treatment provided for only 6 weeks (12 sessions) was sufficient for this participant to achieve clinically significant improvements in gait speed after submeaningful improvements on dalfampridine extended release alone.
Exercise and gait training as an adjunct or alternative to dalfampridine therapy should be explored in larger studies.
Financial Disclosures
Dr. Plummer has served as a consultant and member of the Physical Therapy in Post Ischemic Stroke Advisory Board for Acorda Therapeutics Inc. The other authors declare no conflicts of interest.
References
Goodman AD, Brown TR, Edwards KR, et al. A phase 3 trial of extended release oral dalfampridine in multiple sclerosis. Ann Neurol. 2010;68:494–502.
Goodman AD, Brown TR, Krupp LB, et al. Sustained-release oral fampridine in multiple sclerosis: a randomised, double-blind, controlled trial. Lancet. 2009;373:732–738.
Goodman AD, Brown TR, Schapiro R, Klingler M, Cohen R, Blight AR. A pooled analysis of two phase 3 clinical trials of dalfampridine in patients with multiple sclerosis. Int J MS Care. 2014;16:153–160.
Goodman AD, Brown TR, Cohen JA, et al. Dose comparison trial of sustained-release fampridine in multiple sclerosis. Neurology. 2008;71:1134–1141.
Pearson M, Dieberg G, Smart N. Exercise as a therapy for improvement of walking ability in adults with multiple sclerosis: a meta-analysis. Arch Phys Med Rehabil. 2015;96:1339–1348.
Snook EM, Motl RW. Effect of exercise training on walking mobility in multiple sclerosis: a meta-analysis. Neurorehabil Neural Repair. 2009;23:108–116.
Rietberg MB, Brooks D, Uitdehaag BM, Kwakkel G. Exercise therapy for multiple sclerosis. Cochrane Database Syst Rev. 2005;1:CD003980.
Latimer-Cheung AE, Pilutti LA, Hicks AL, et al. Effects of exercise training on fitness, mobility, fatigue, and health-related quality of life among adults with multiple sclerosis: a systematic review to inform guideline development. Arch Phys Med Rehabil. 2013;94:1800–1828.
Haselkorn JK, Hughes C, Rae-Grant A, et al. Summary of comprehensive systematic review: rehabilitation in multiple sclerosis: report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology. 2015;85:1896–1903.
Swinnen E, Beckwee D, Pinte D, Meeusen R, Baeyens JP, Kerckhofs E. Treadmill training in multiple sclerosis: can body weight support or robot assistance provide added value? a systematic review. Mult Scler Int. 2012;2012:240274.
Goldman MD, Motl RW, Scagnelli J, Pula JH, Sosnoff JJ, Cadavid D. Clinically meaningful performance benchmarks in MS: timed 25-foot walk and the real world. Neurology. 2013;81:1856–1863.
Guadagnoli MA, Lee TD. Challenge point: a framework for conceptualizing the effects of various practice conditions in motor learning. J Mot Behav. 2004;36:212–224.
Plummer-D'Amato P, Altmann LJ, Behrman AL, Marsiske M. Interference between cognition, double-limb support, and swing during gait in community-dwelling individuals poststroke. Neurorehabil Neural Repair. 2010;24:542–549.
Plummer P. Critical appraisal of evidence for improving gait speed in people with multiple sclerosis: dalfampridine versus gait training. Int J MS Care. 2016;18:105–115.







