Publication
Research Article
International Journal of MS Care
Occupation-Based Intervention for People With Multiple Sclerosis: A Feasibility Study
ABSTRACT
BACKGROUND:
This study aims to evaluate the feasibility of an occupation-based intervention (OBI) on dexterity and occupational performance for people with multiple sclerosis (MS) and to gather preliminary efficacy data.
METHODS:
In this feasibility study, 2 women with MS participated in 12 OBI sessions that focused on increasing upper extremity function. The Canadian Occupational Performance Measure, 9-Hole Peg Test, Expanded Disability Status Scale, Montreal Cognitive Assessment, and Fatigue Severity Scale (FSS) were used as outcome measures. The scores of these assessments are reported descriptively.
RESULTS:
According to preliminary data, both participants demonstrated improvements in dexterity, occupational performance, and occupational performance satisfaction. These data suggest that OBI may be implemented effectively in Iran.
CONCLUSIONS:
OBI improved the functional use of the participants’ upper extremities as well as their occupational performance and satisfaction with their occupational performance in each of the 2 women with MS. This preliminary intervention program should be further tested using randomized controlled trials.
People with multiple sclerosis (MS) may confront complex motor, sensory, visual, cognitive, and psychological symptoms.1 In recent decades, numerous studies have focused on lower extremity functioning, gait, and balance changes that occur in the early stages of MS. However, there have been few studies that examine hand and upper extremity function changes in people with MS.2 Approximately three-quarters of people with MS have demonstrated upper extremity dysfunction on 1 or both sides of their bodies.3,4 Upper extremity dysfunction contributes to reducing the ability to perform activities of daily living and is an important predicator of overall activity and participation within the community,5 possibly resulting in decreased independence and lower quality of life.6
Several rehabilitation interventions have been developed to address upper extremity dysfunction, such as exercise training, task-oriented training, sensory training, robotics, and constraint-induced movement therapy. According to a systematic review, however, there is a lack of sufficient evidence of improvement, perhaps because the interventions do not target the upper extremity exclusively.2
Occupational therapists are rehabilitation team members who focus on improving occupational performance through occupation-based interventions (OBIs). OBI is a patient-centered practice in which the occupational therapist, in collaboration with the patient, chooses interventions based on the patient’s interests, needs, health, and participation in daily life.7
OBI provides a holistic and a strong base for patients to achieve their occupational therapy goals, enhances the ability of therapists to communicate with their patients, and can improve patients’ satisfaction with services.8 However, occupation-based therapies are somewhat culture dependent, so it is necessary to investigate their effectiveness in different cultures.9 Some barriers to using OBI are that therapists lack the knowledge and skills to implement the theory into practice,8 preference for the dominant medical model, patient request, lack of resources, environmental context,10 culture,11 and time required for goal setting.12
Preliminary evidence supports the effectiveness of OBI for people with some degenerative and neurologic diseases such as stroke or a traumatic brain injury.13 The aim of this study is to describe the development and content of an OBI program focused on hand function that was used to improve the occupational performance of 2 Iranian women with MS.
METHODS
This feasibility study evaluated the effect of OBI for hand function on 2 women with MS from the Isfahan MS Society. Both volunteers were examined by a neurologist to determine the type of MS they have and their level of disability.
After explanations of the purpose of the study, written consent was obtained from both of the participants and they were assured that their information would be kept confidential. This study was approved by the Ethics Committee of the University of Social Welfare and Rehabilitation Sciences under the code of ethics IR.USWR.REC.1396.319.
Participants
Participant 1 was a divorced woman, aged 41 years, with an undergraduate education. Her MS was diagnosed 9 years ago. She has no income or insurance and lives with her mother. According to her report, the strength and coordination of movement in her hands and upper extremities has worsened with the progression of MS symptoms. She needs help in home maintenance and self-care, including bathing and hair brushing.
Participant 2 was a woman, aged 50 years. Her MS was diagnosed 12 years ago. She states that she feels numbness and tingling, and has decreased hand strength and endurance. Sometimes she is responsible for taking care of her grandson and her mother-in-law, who had a stroke. She is independent in all her self-care and mobility activities, but struggles with home maintenance activities.
Study Instruments
The Montreal Cognitive Assessment (MoCA) was used because it is more sensitive than the Mini–Mental State Examination in identifying mild cognitive impairment in the general population.14 The Cronbach α of the MoCA has been reported as 0.77; a cutoff score of 24 is considered mild cognitive impairment.15
The Expanded Disability Status Scale (EDSS) was used to evaluate the severity of the participants’ MS. A higher score on this scale indicates a higher degree of severity.16 The validity and reliability of this tool are adequate.17
The Canadian Occupational Performance Measure (COPM) was used to investigate occupational performance.18 It is a valid and reliable tool with acceptable test-retest reliability and content validity that identifies occupational performance problems across the areas of self-care, productivity, and leisure through a semistructured interview.18–20 A self-rated score of 1 indicates minimum performance and satisfaction with performance, and a score of 10 is the highest score.
The 9-Hole Peg Test (9HPT) is the gold standard tool for evaluating hand dexterity. Interrater and test-retest reliability of this test is high.21 Bertoni et al reported a cutoff point of greater than 1.95 SD of the norm.22
The Fatigue Severity Scale (FSS) is a 9-point scale assessing fatigue in people with MS. Lower scores on this scale indicate less fatigue and less impact on everyday life activities. The test-retest reliability of this tool in Iran is 0.93.23 The lowest score possible is 9 and the highest is 63.
Inclusion criteria were a neurologist-determined EDSS score between 3.5 and 5.5 (ie, able to walk independently) and a MoCA score of greater than 24.
Procedure
Initially, the primary clinical program was developed based on a comprehensive review of OBIs, as well as the biomechanical model and interventions used in rehabilitation of hand and upper extremities with persons with MS.24 The OBI used in this study guides patients through their self-identified goals regarding their occupational hand function. The developed intervention uses the Model of Human Occupation25 (MOHO) to describe occupational performance and participant involvement; motivation for, as well as patterns and performance of, daily tasks; and the fit between occupational goals, participant ability, and capacity in hand function and environment.26 The therapist used MOHO strategies to support the participants, including validating, identifying, giving feedback, advising, negotiating, structuring, coaching, encouraging, and providing physical support.26 In addition, solution-focused coaching,27 adult learning theory,28 solution-focused therapy,29 and self-management30 were used as components of the intervention. Each session was approximately 1 hour and occurred 2 times a week for 6 weeks. The content of the sessions was based on the participants’ selected goals and priorities based on the COPM (TABLE 1).
Characteristics and Process of the Occupation-Based Intervention
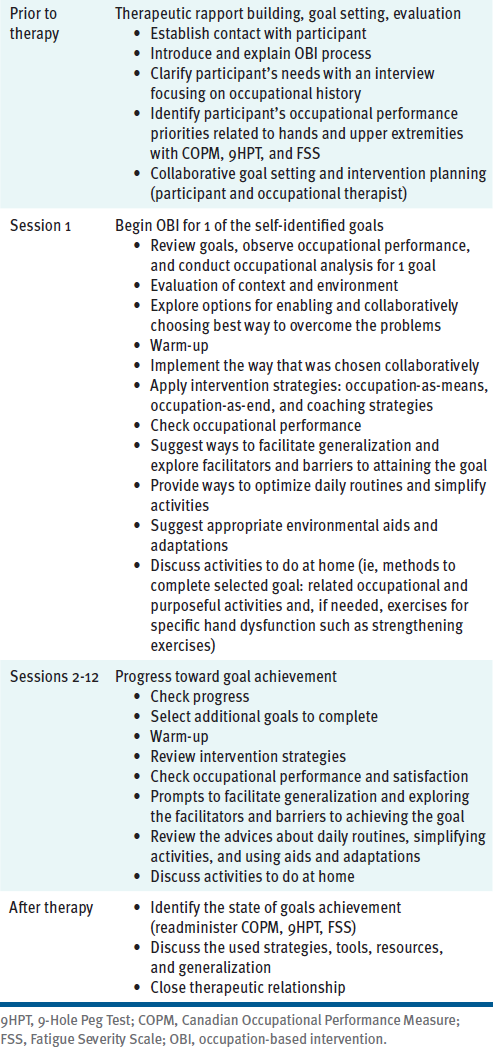
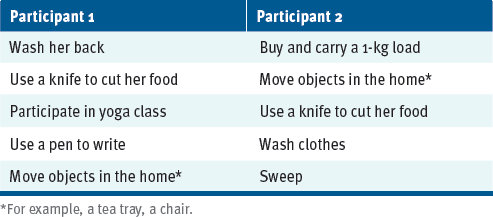
At the first session, both participants chose their own goals (TABLE 2). In the second session, the therapist asked them about how they did activities in the past, observed how these tasks were currently performed, and discussed how performance could be improved by asking reflective questions. During the sessions, the emphasis was on self-assessment. The occupational therapist and patient also discussed ways to promote the construction of a daily routine, to return to a healthy routine, to develop positive habits to save energy, to increase ways to be active for a longer time, and methods to prevent fatigue. When the goals were achieved, the next goal was examined. Reevaluation was conducted in the week after attaining the goal.
Participants' Goals
Validity of the OBI Program
The validity of the OBI program was investigated in interviews with 5 occupational therapists who had at least 5 years of clinical experience focused on OBI. The experts evaluated the validity of the intervention program rating the simplicity, clarity, relevance, and necessity of the program on a Likert scale. They were asked to recommend suggestions, corrections, or additions. The experts had an average work experience of 10.2 (SD = 3.4) years. Three of them had a doctorate degree, 1 had a master’s degree, and 1 had a bachelor’s degree; 4 were women. Analysis of the experts’ opinions showed that the program was written simply and clearly and that all written content was essential and relevant.
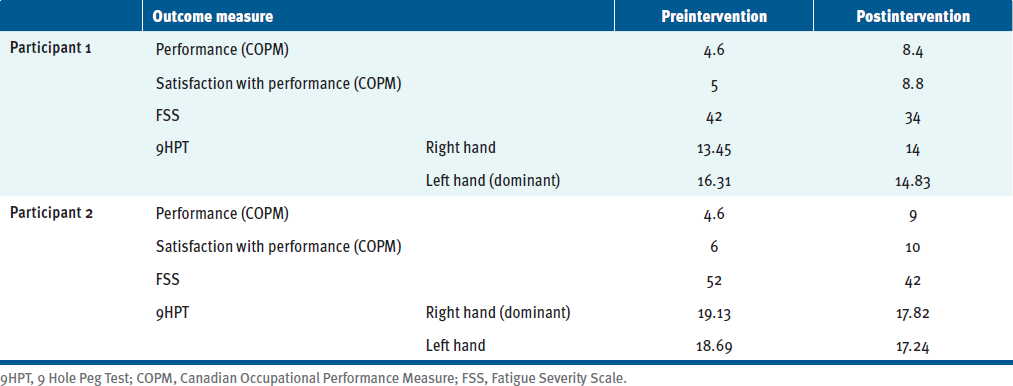
RESULTS
TABLE 3 descriptively summarizes the COPM, 9HPT, and FSS data. MoCA scores indicated mild cognitive impairment for participant 2 and no cognitive impairment for participant 1. Both participants had an EDSS score of 3.5, indicating moderate disability but no walking impairment. Participant 1 and participant 2 achieved their goals in 8 and 10 sessions, respectively, confirmed by the changes in COPM scores. Both participants had an increase of more than 2 points for both performance and satisfaction, indicating that the OBI intervention made a difference in goal obtainment.
Preintervention and Postintervention Scores on COPM, 9HPT, and FSS
DISCUSSION
The results of this study indicate an improvement in goal performance and performance satisfaction for both participants, as a change of more than 2 points on the COPM31 is clinically meaningful. Likewise, the women’s 9HPT scores reflected improvement in dexterity. FSS scores also indicated reduced fatigue severity for both participants.
In Eastern culture, which includes Iran, people are usually supported by their families during illness, and people with disabilities often come to rely on others for help completing certain tasks and activities of daily living.11 This is juxtaposed with the fact that, in Iran, housework is often performed by women, and women are mostly responsible for caring for other family members. In the context of this study, one of the participants was divorced and the other was responsible for caring for others, so their motivation to achieve maximum hand function was very high.
It was determined that the participants could achieve the goals in 12 sessions of evidence-based, occupation-focused, and patient-centered therapy interventions, but both participants achieved their goals in fewer sessions. The intervention emphasized improving hand and upper extremity performance to meet occupational goals. Using OBI, the occupational therapist collaborated with the participants to help them find new ways to perform daily tasks. The collaboration between the therapist and the participant as well as participant feedback at all stages of the intervention was paramount. The intervention plan was continually adjusted and tailored to the needs of the individual. To ease the process of time-consuming goal setting, a semistructured COPM interview and occupational profile were used.
This was a preliminary study. Generalization would require more robust design. For example, participants in this study did not have significant cognitive problems, so future research should include people with different levels of MS severity in all areas.
CONCLUSIONS
This study introduces a simple, structured occupational therapy intervention for people with MS. The improvements in occupational performance, occupational satisfaction, and hand dexterity experienced by both participants suggest that OBI has the feasibility to be implemented with individuals with MS in Iran. More research with a larger sample size is needed to establish the effectiveness of this occupational therapy intervention among a wider population with varying degrees of MS severity and impairment.
PRACTICE POINTS
This feasibility study provides preliminary evidence on the applicability of an occupation-based intervention for upper extremity function for people with multiple sclerosis.
Collaborative goal setting in occupation-based interventions may increase patients’ motivation to participate in the rehabilitation program.
References
Kister I, Bacon TE, Chamot E, et al. Natural history of multiple sclerosis symptoms. Int J MS Care. 2013;15(3):146-158. doi: 10.7224/1537-2073.2012-053
Lamers I, Maris A, Severijns D, et al. Upper limb rehabilitation in people with multiple sclerosis: a systematic review. Neurorehabil Neural Repair. 2016;30(8):773-793. doi: 10.1177/1545968315624785
Chruzander C, Johansson S, Gottberg K, et al. A 10-year follow-up of a population-based study of people with multiple sclerosis in Stockholm, Sweden: changes in disability and the value of different factors in predicting disability and mortality. J Neurol Sci. 2013;332(1-2):121-127. doi: 10.1016/j.jns.2013.07.003
Johansson S, Ytterberg C, Claesson IM, et al. High concurrent presence of disability in multiple sclerosis. Associations with perceived health. J Neurol. 2007;254(6):767-773. doi: 10.1007/s00415-006-0431-5
Kierkegaard M, Einarsson U, Gottberg K, von Koch L, Holmqvist LW. The relationship between walking, manual dexterity, cognition and activity/participation in persons with multiple sclerosis. Mult Scler. 2012;18(5):639-646. doi: 10.1177/1352458511426736
Noori M, Hosseini SA, Shiri V, Akbarfahimi N. The relationship between balance and activities of daily living with the quality of life of patients with relapsing-remitting multiple sclerosis. J Rehabil. 2019;19(4):292-301. doi: 10.32598/rj.19.4.292
American Occupational Therapy Association. Occupational therapy practice framework: domain and process. 3rd ed. Am J Occup Ther. 2014;68:S1-S48. doi: 10.5014/ajot.2014.682006
Lee SW, Taylor R, Kielhofner G, Fisher G. Theory use in practice: a national survey of therapists who use the Model of Human Occupation. Am J Occup Ther. 2008;62(1):106-117. doi: 10.5014/ajot.62.1.106
Castro D, Dahlin-Ivanoff S, Mårtensson L. Occupational therapy and culture: a literature review. Scand J Occup Ther. 2014;21(6):401-414. doi: 10.3109/11038128.2014.898086
Daud AZC, Judd J, Yau M, Barnett F. Issue in applying occupation-based intervention in clinical practice: a Delphi study. Procedia Soc Behav Sci. 2016;222:272-282. doi: 10.1016/j.sbspro.2016.05.158
Yang S, Shek MP, Tsunaka M, Lim HB. Cultural influences on occupational therapy practice in Singapore: a pilot study. Occup Ther Int. 2006;13(3):176-192. doi: 10.1002/oti.217
Eyssen IC, Steultjens MP, de Groot V, et al. A cluster randomised controlled trial on the efficacy of client-centered occupational therapy in multiple sclerosis: good process, poor outcome. Disabil Rehabil. 2013;35(19):1636-1646. doi: 10.3109/09638288.2012.748845
Kim SH, Park JH. The effect of occupation-based bilateral upper extremity training in a medical setting for stroke patients: a single-blinded, pilot randomized controlled trial. J Stroke Cerebrovasc Dis. 2019;28(12):104335. doi: 10.1016/j.jstrokecerebrovasdis.2019.104335
Ahmadi MA, Ashrafi F, Behnam B. Comparison of Montreal Cognitive Assessment test and Mini Mental State Examination in detecting cognitive impairment in relapsing-remitting multiple sclerosis patients. Int Clin Neurosci J. 2015;2(4):137-141. doi: 10.22037/icnj.v2i4.11665
Emsaki G, Molavi H, Chitsaz A, Abtahi MM, Asgari K. Psychometric properties of the Montreal Cognitive Assessment (MoCA) in Parkinson’s disease patients in Isfahan. J Isfahan Med Sch. 2011;29(158):1606-1615.
Kurtzke, J. (1983). Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS). Neurology. 1983;33(11):1444-1452. doi: 10.1212/wnl.33.11.1444
Amato MP, Fratiglioni L, Groppi C, Siracusa G, Amaducci L. Interrater reliability in assessing functional systems and disability on the Kurtzke scale in multiple sclerosis. Arch Neurol. 1988;45(7):746-748. doi: 10.1001/archneur.1988.00520310052017
Law M, Baptiste S, McColl M, Opzoomer A, Polatajko H, Pollock N. The Canadian occupational performance measure: an outcome measure for occupational therapy. Can J Occup Ther. 1990;57(2):82-87. doi: 10.1177/000841749005700207
Atashi N, Aboutalebi S. Reliability of the Persian version of Canadian Occupational Performance Measure for Iranian elderly population. Iranian Rehab J. 2010;8(12): 26-30.
Dehghan L, Dalvand H, Pourshahbaz A, Samadi S. Designing supplement form of the Canadian Occupational Performance Measure: item analysis and suggestions for refinement. Article in Persian. Rehab J. 2014;15(1):8-21.
Feys P, Lamers I, Francis G, et al. The Nine-Hole Peg Test as a manual dexterity performance measure for multiple sclerosis. Mult Scler. 2017;23(5):711-720. doi: 10.1177/1352458517690824
Bertoni R, Lamers I, Chen CC, Feys P, Cattaneo D. Unilateral and bilateral upper limb dysfunction at body functions, activity and participation levels in people with multiple sclerosis. Mult Scler. 2015;21(12):1566-1574. doi: 10.1177/1352458514567553
Azimian M, Shahvarughi Farahani A, Dadkhah A, Fallahpour M, Karimlu M. Fatigue severity scale: the psychometric properties of the Persian-version in patients with multiple sclerosis. Res J Biol Sci. 2009;4(9):974-977.
Skirvan TM, Osterman AL, Fedorczyk J, Arnadio PC. Rehabilitation of the Hand and Upper Extremity. Vol 2. 6th ed. Mosby; 2011.
Kielhofner G. A Model of Human Occupation: Theory and Application. Lippincott, Williams, and Wilkins; 2002.
Kielhofner G. Conceptual Foundations of Occupational Therapy Practice. FA Davis; 2009.
O’Connell B, Palmer S, Williams H. Solution Focused Coaching in Practice. Routledge; 2013.
Kaufman DM. Applying educational theory in practice. BMJ. 2003;326(7382):213-216. doi: 10.1136/bmj.326.7382.213
Macdonald A. Solution-Focused Therapy: Theory, Research and Practice. Sage; 2011.
Audulv Å, Ghahari S, Kephart G, Warner G, Packer TL. The taxonomy of everyday self-management strategies (TEDSS): a framework derived from the literature and refined using empirical data. Patient Educ Couns. 2019;102(2):367-375. doi: 10.1016/j.pec.2018.08.034
Law M, Baum C, Dunn W. Supporting Best Practice in Occupational Therapy. Slack Incorporated; 2005.







