Publication
Research Article
International Journal of MS Care
Selecting Rehabilitation Outcome Measures for People with Multiple Sclerosis
Author(s):
Despite the well-known benefits of using standardized outcome measures (OMs) in clinical practice, a variety of barriers interfere with their use. In particular, rehabilitation therapists lack sufficient knowledge in selecting appropriate OMs. The challenge is compounded when working with people with multiple sclerosis (MS) owing to heterogeneity of the patient population and symptom variability in individual patients. To help overcome these barriers, the American Physical Therapy Association appointed the Multiple Sclerosis Outcome Measures Task Force to review and make evidence-based recommendations for OM use in clinical practice, education, and research specific to people with MS. Sixty-three OMs were reviewed based on their clinical utility, psychometric properties, and a consensus evaluation of the appropriateness of use for people with MS. We sought to illustrate use of the recommendations for two cases. The first case involves a 43-year-old man with new-onset problems after an exacerbation. The second case pertains to an outpatient clinic interested in assessing the effectiveness of their MS rehabilitation program. For each case, clinicians identified areas that were important to assess and various factors deemed important for OM selection. Criteria were established and used to assist in OM selection. In both cases, the described processes narrowed the selection of OMs and assisted with choosing the most appropriate ones. The recommendations, in addition to the processes described in these two cases, can be used by clinicians in any setting working with patients with MS across the disability spectrum.
Despite the importance of measuring outcomes in clinical practice, a variety of barriers limit the use of standardized outcome measures (OMs), and evidence suggests that rehabilitation therapists do not routinely apply them in practice.1 One barrier that restricts the use of OMs is lack of knowledge to choose the most appropriate OM for a given patient or situation.2,3 Selection of OMs has received considerable attention,4–10 but little information exists to specifically describe clinical decision-making processes that clinicians can use in practice. Rehabilitation therapists working with people with multiple sclerosis (MS) have additional challenges in OM selection because of the heterogeneous patient population and symptom variability in individual patients.
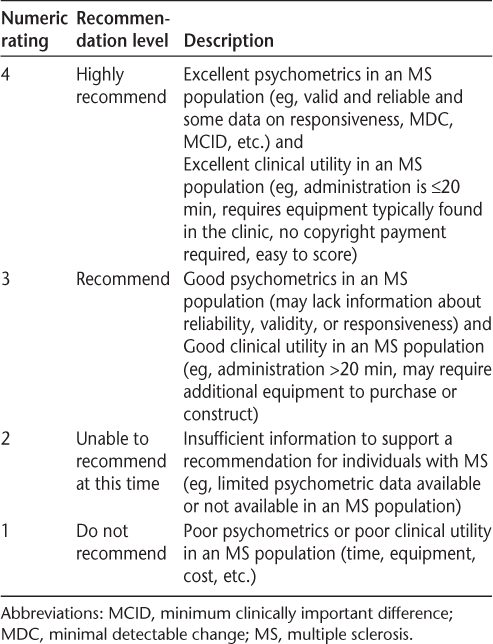
In 2010, the Neurology Section of the American Physical Therapy Association appointed the Multiple Sclerosis Outcome Measures Task Force (MSTF) to review and make evidence-based recommendations for the use of OMs in clinical practice, education, and research specific to people with MS. Sixty-three rehabilitation OMs were reviewed. An Evaluation Database to Guide Effectiveness (EDGE) form, developed by the Research Section of the American Physical Therapy Association, was modified and used by the MSTF to record each OM's properties, psychometrics, clinical utility, and recommendations. Recommendations were based on an analysis of the OM's clinical utility, a synthesis of psychometric data, and a consensus evaluation of the appropriateness of the OM for people with MS via a modified Delphi process. A 4-point rating scale, based on the strength of the OM's psychometrics and clinical utility, was used to evaluate each OM and provide recommendations for use in patients across the MS disability spectrum and in five practice settings (Table 1). These recommendations have been published previously.11
The Multiple Sclerosis Outcome Measures Task Force's outcome measure rating scale
The purpose of this article is to describe the clinical decision-making process for selecting OMs for two distinct MS-related cases. We demonstrate application of the MSTF recommendations to select the appropriate OMs for one individual with MS and one outpatient program for MS. The overarching question for each case was, “Which OM(s) should be selected?” To answer this question for each case, the rehabilitation therapist considered OMs across body function, activity, and participation levels of the International Classification of Function, Disability, and Handicap, 12 aiming to select OMs with high clinical utility and adequate psychometrics. Additional criteria and questions were used to assist in OM selection for each of the two cases. The reader is referred to the MSTF's previous work for detailed information on each OM discussed in the following cases.11,13
Case 1: Selecting Rehabilitation OMs for a Person with MS
The rehabilitation clinician conducts a detailed interview and systems review with an individual with MS to identify which constructs (ie, issues or concerns) might require standardized assessment. Factors to consider include the MS disease phenotype and severity, health-care setting, premorbid and comorbid conditions, goals identified by the patient, issues raised during the history and interview, and any occult issues (eg, fatigue or depression) that may not be obvious at the outset. The goal in identifying constructs is to direct and narrow the selection of OMs. The clinician chooses the OMs that are closely aligned with the patient's goals, most helpful in guiding decisions about intervention, and able to provide a basis for accurate documentation of changes during the intervention period.
Case Description
Mr. G is 43 years old, has a 10-year history of relapsing-remitting MS, and is receiving care in an outpatient setting. He recently experienced an exacerbation and has subsequently had several falls. He was previously independent in all aspects of functional mobility and was working full time as a computer programmer. His chief concerns are marked fatigue and a decline in left arm and hand function and walking ability. Mr. G's primary goal is to return to work as a computer programmer. Findings from the systems review and screening examination appear in Table 2. The clinician determined that three health-related constructs were most important for this patient: upper-extremity function, fatigue, and walking ability. The clinician investigated OMs appropriate for the setting (outpatient) and for Mr. G's Expanded Disability Status Scale14 (EDSS) score of 6.0.
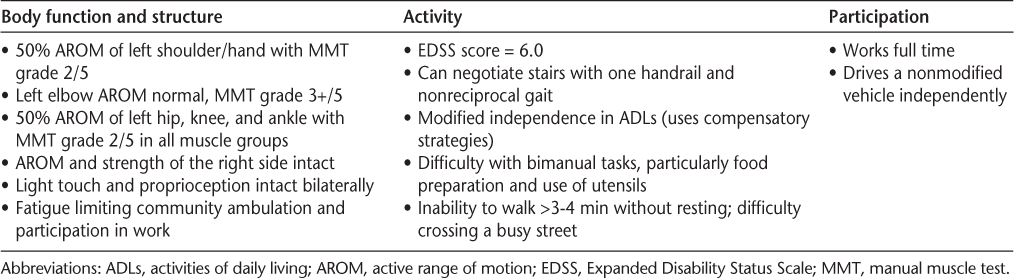
Systems review and screening examination findings
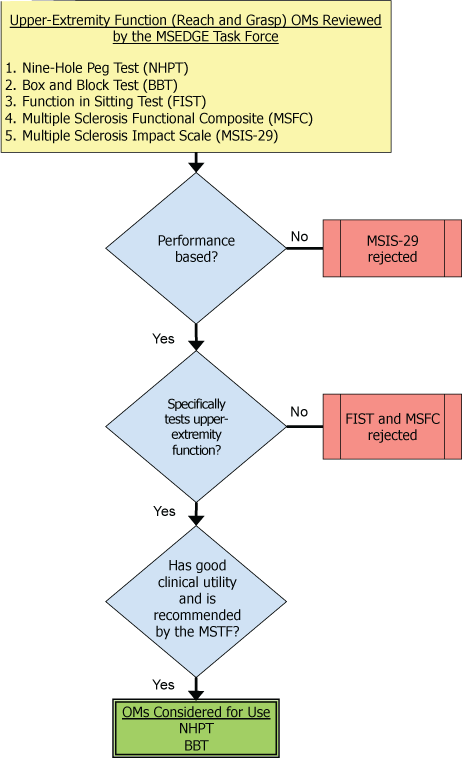
Selecting an OM for Upper-Extremity Function
The clinician wanted a performance-based standardized OM that would document the baseline agility of the upper extremities in a way most relevant to the patient's desired computer programming occupation. The MSTF reviewed five OMs that measured upper-extremity function. Each OM was screened for appropriateness for this case using the following criteria: a performance-based, standardized test of upper-extremity function with good clinical utility (Figure 1). In this case, a performance-based test was preferred over a self-report measure because the clinician wanted to measure actual, not perceived, upper-extremity functional ability. Two measures met the criteria:
Nine-Hole Peg Test (NHPT): A timed test whereby the individual removes nine ¼-inch pegs from a well, places them in a pegboard, and then replaces them back in the well, performing the sequence with the dominant and nondominant hands.15
Box and Block Test (BBT): A timed test in which the individual moves as many 1-inch blocks, one at a time, from one container to another within 1 minute.16
The MSTF recommendations for the NHPT and the BBT indicate that there is essentially equivalent psychometric data for these OMs in the MS population, and both require little time (<5 minutes) to administer. The NHPT was selected for two reasons. Because the patient was a computer programmer, the finer grip required for the NHPT (¼-inch pegs) was preferred to the grip required when manipulating the 1-inch cubes used for the BBT. Also, the NHPT has somewhat better clinical utility because the required equipment is less expensive than that required for the BBT.
Decision tree for selecting an outcome measure (OM) for upper-extremity function
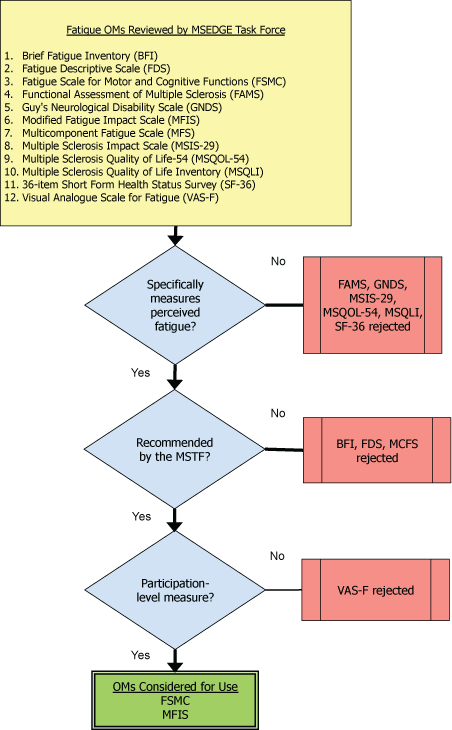
Selecting an OM for Perceived Fatigue
The clinician wanted a self-report measure of the impact of fatigue on Mr. G's participation in life. The MSTF reviewed 12 OMs that addressed the construct of fatigue. All 12 measures were screened for appropriateness for this case considering the following criteria: a participation-level measure specifically for fatigue that was recommended for use given the setting and the patient's level of disability (Figure 2). Two self-report OMs met the criteria:
The Fatigue Scale for Motor and Cognitive Functions (FSMC): A 20-item OM developed as a measure of cognitive and motor fatigue for people with MS.17
The Modified Fatigue Impact Scale (MFIS): A 21-item OM that assesses the effects of fatigue on physical, cognitive, and psychosocial functioning in people with MS.18
The FSMC and the MFIS have equal ratings and approximately equivalent clinical utility, as seen on their respective EDGE forms. The MFIS has data to support calculation of minimal detectable change for the total scale and its subscales (ie, physical, cognitive, and psychosocial). Having a minimal detectable change will help the clinician determine whether any changes with intervention are large enough to rule out measurement error, suggesting that a positive change is likely due to the intervention provided. A drawback to the MFIS for some situations is that it is recommended only for use in people with an EDSS score of up to 7.5 (because the literature reported use in these populations), whereas the FSMC was recommended for use in patients at all EDSS levels. This might make the FSMC a better choice when long-term outcomes across increasingly severe disability levels are a high priority. For this case, the MFIS was chosen because of the availability of minimal detectable change data and the expectation that this episode of care will be discrete.
Decision tree for selecting an outcome measure (OM) for perceived fatigue
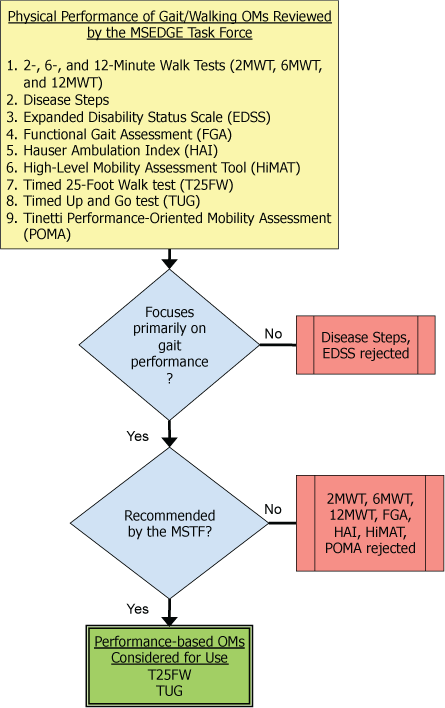
Selecting an OM for Gait and Walking Ability
Because the patient reported reduced walking ability, the clinician wanted an OM of physical performance and self-report. The MSTF reviewed nine performance-based gait measures. These were screened for appropriateness for this case considering the following criteria: focuses primarily on gait performance and was most highly recommended for use given the setting and the patient's level of disability (Figure 3). The MSTF reviewed five self-report gait measures. These were screened for appropriateness for this case considering the following criteria: focuses primarily on the impact of gait limitations and was highly recommended by the MSTF for use given the setting and the patient's level of disability (Figure 4). Two OMs met the criteria for physical performance, but only one met the criteria for self-report:
The Timed 25-Foot Walk test (T25FW): A measure of gait velocity as one walks 25 feet while timed.19
The Timed Up and Go test (TUG): The time for the person to stand up from a chair, walk 3 m, turn and walk back to the chair, and sit down.20
The 12-item Multiple Sclerosis Walking Scale (MSWS-12): A self-report measure of the impact of MS on the individual's walking ability.21
Decision tree for selecting an outcome measure (OM) for gait/walking performance
Decision tree for selecting an outcome measure (OM) for self-report of gait/walking ability
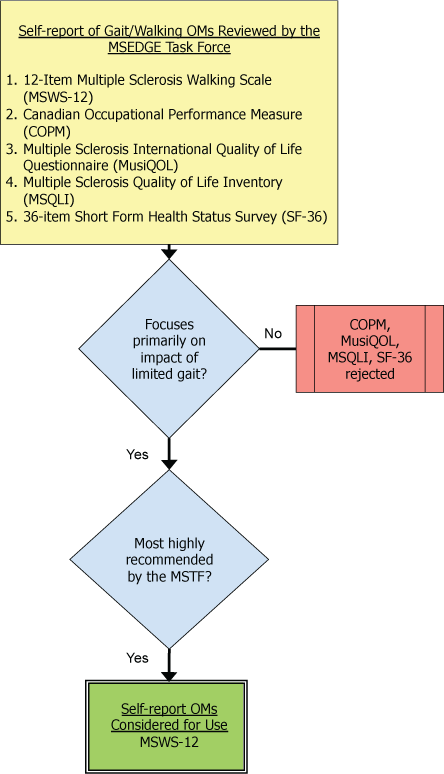
The decision was to use the T25FW in conjunction with the MSWS-12. Although the TUG and T25FW were each recommended by the MSTF, there is a richer body of literature for the T25FW for people with MS (eg, predictive and discriminative validity and responsiveness data). In addition, the TUG includes sit to/from stand and turning, yet neither was identified as problematic by the patient. An assessment of pure gait speed measured by the T25FW was determined to be more important because normative values for gait speed could help in setting goals and measuring progress. The MSWS-12 can provide the rehabilitation therapist with the patient's perception of the degree of limitations in walking ability in a variety of contexts (eg, indoors vs. outdoors) and has useful responsiveness and normative data. In addition, the MSWS-12 was viewed as a helpful complement to the T25FW because the T25FW is traditionally performed on an indoor level surface but the MSWS-12 includes items pertaining to a variety of gait-related tasks in the home and community.
To summarize, the clinician can use the four OMs selected—the NHPT, MFIS, T25FW, and MSWS-12—to record baseline performance and to monitor for changes throughout at the end of the episode of care.
Case 2: Selecting Rehabilitation OMs for People with MS in a System of Care
The clinician sometimes wants to assess the effectiveness of a rehabilitative program for multiple people rather than a single individual with MS. The goal is to standardize data collected on all people with MS who receive services in the practice so that the clinician can examine the outcomes of the practice as a whole.
Case Description
A local interdisciplinary rehabilitation practice (“the practice”) offers a long-term outpatient rehabilitation program (“the program”) for people with MS with EDSS scores of 0 to 7.5. The program focuses on restoration of maximal function and prevention of secondary complications. Team members include physical therapists, occupational therapists, speech-language pathologists, social workers, physicians, and others. In addition, the practice received a community grant from a charitable organization to provide program services to people with MS in the community.
To assess the success of the program, the practice manager wanted to identify a set of standard OMs to be collected at baseline and quarterly for each participant. To facilitate comparison within and across all patients receiving care at the program, the items should be standardized and not individualized (ie, not patient or clinician identified as in Goal Attainment Scaling).22 The aggregate data would help document and examine the program and would be used for internal research to provide outcome information to the charitable organization in hopes of securing additional community grant funds. Because MS presentation is heterogeneous, there is no “typical” clinical presentation. In addition, OMs need to have relevance for the multiple disciplines involved. Clinician time and facility resources are also important. Thus, body function measures were considered less useful because many of these are patient and discipline specific; the focus was on activity- and participation-level measures of the constructs most commonly affected in people with MS.
The practice identified the following three constructs as most important for measurement across the population served: quality of life (QOL) (a participation-level construct), general physical function/activity (an activity-level construct), and endurance (assessed as an activity- or participation-level construct).
Selecting an OM for QOL
The MSTF recommendations included nine OMs that measure various aspects of QOL and were deemed appropriate for the practice setting (outpatient) and the EDSS scores of the population (generally 0–7.5). The practice manager considered the following criteria: the OM should be comprehensive and measure varied constructs, be appropriate for research for program-level review of effectiveness, and be inexpensive to use (Figure 5). Four measures of QOL met the criteria for consideration:
The Functional Assessment of Multiple Sclerosis: A 59-item measure of QOL in six domains (mobility, symptoms, emotional well-being, general contentment, thinking/fatigue, and family/social well-being).23
The abbreviated version of the Multiple Sclerosis Quality of Life Inventory (MSQLI): A QOL measure totaling 81 items covering discrete aspects of QOL (eg, general health, fatigue, vision, and others).10
Multiple Sclerosis Impact Scale (MSIS-29): A 29-item self-report measure with 20 items associated with a physical scale and nine items associated with a psychological scale.24
Multiple Sclerosis Quality of Life (MSQOL-54): A multidimensional health-related QOL measure that combines generic and MS-specific items into a single instrument.25
Decision tree for selecting an outcome measure (OM) for quality of life (QOL)
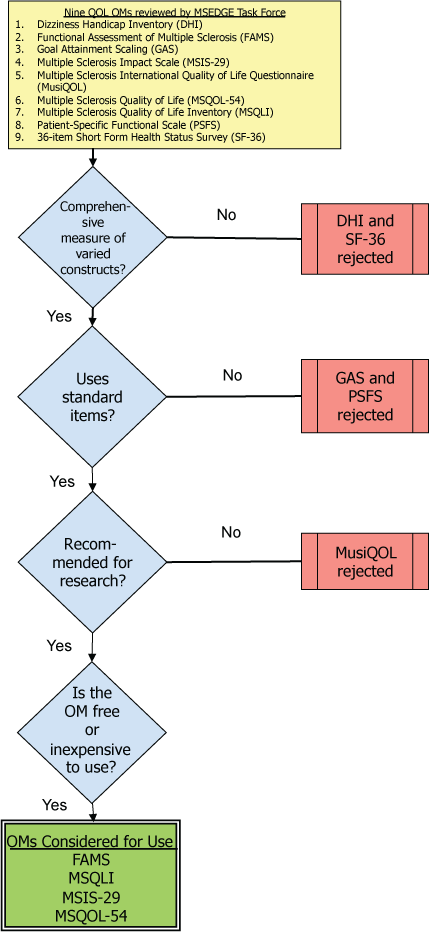
Ultimately, the program opted to implement the abbreviated version of the MSQLI because a separate score is calculated for each questionnaire, enabling the practice to better identify specific disciplinary strengths and weaknesses of the program. The MSTF rating of “recommend” for the MSQLI was based on its good psychometric properties, but it has limited clinical utility: approximately 30 minutes is required to complete the questionnaire, and additional time is required for scoring. This is in contrast to the MSQOL-54 and MSIS-29, which were rated “highly recommend” by the MSTF. The MSQOL-54 and MSIS-29 take approximately 15 minutes to complete but are less comprehensive, measuring fewer aspects of QOL compared with the MSQLI. Of benefit, most patients seen at the practice could complete the MSQLI independently, reducing the administration time by the clinician.
Selecting an OM for Physical Function/Activity
The MSTF recommendations included seven OMs of general physical activity and were deemed appropriate for the practice setting (outpatient) and the EDSS scores of the population (generally 0–7.5). The practice manager screened OMs for those that are comprehensive (measuring multiple items) and likely to be appropriate for research for program-level review of effectiveness (Figure 6). Two measures met these requirements:
MSIS-29: Previously described.24
Multiple Sclerosis Functional Composite (MSFC): A tool consisting of three discrete performance-based tests: the NHPT (for upper-extremity function), the T25FW (for walking/lower-extremity function), and the 3-Second Paced Serial Addition Test (for cognition/working memory).26
Decision tree for selecting an outcome measure (OM) for physical function/activity
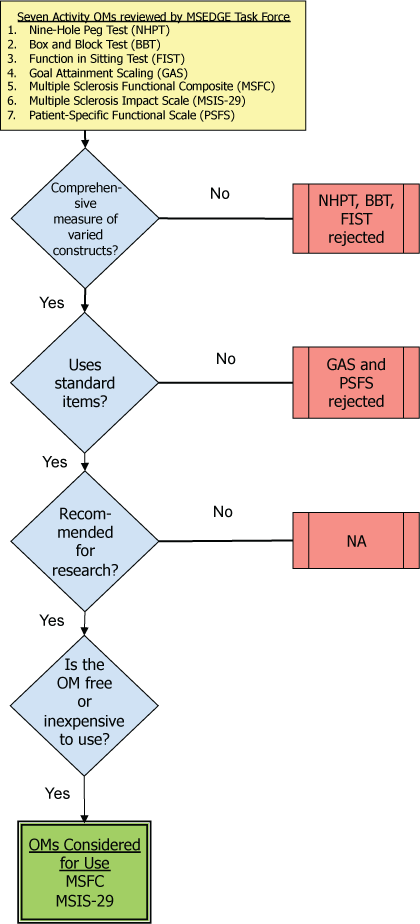
The practice opted to implement the MSFC because it is a measure of general physical and cognitive function. In addition, some of the content of the MSIS-29 is captured in the MSQLI, selected previously, and the team aimed to avoid redundancy of information gathered from the measures selected. Last, the three separate measures included in the MSFC enable a representative examination of the strengths and weaknesses of different disciplines in the practice.
Selecting an OM for Endurance
The MSTF identified nine OMs of aerobic capacity/endurance. The practice manager screened these OMs to include standardized measures of functional endurance that are appropriate for research for program-level review of effectiveness and that demonstrated good clinical utility (Figure 7).
Decision tree for selecting an outcome measure (OM) for endurance
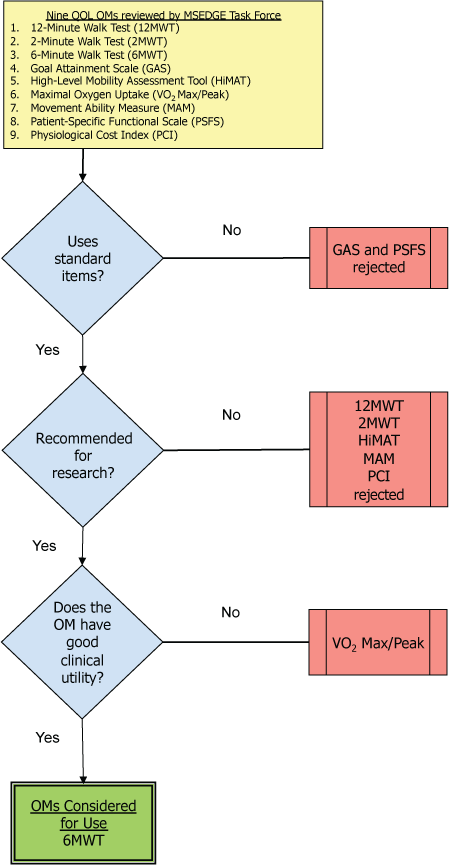
Only the Six-Minute Walk Test (6MWT) met the criteria identified by the program. The 6MWT measures the distance the person can walk in 6 minutes.27 This is a particularly good option because responsiveness and normative data in MS exist for the 6MWT, enabling within- and between-patient comparisons and overall program evaluation.
To summarize, the practice was seeking OMs that were standardized, easy to administer, broad in scope, and useful for program evaluation. In addition to individualized examinations conducted by each member of the health-care team, each participant who entered the program was tested using the MSQLI, MSFC, and 6MWT.
Discussion
This article illustrates a clinical decision-making process by which the recommendations of the MSTF were used to select appropriate OMs for an individual person with MS and for programmatic assessment in an interdisciplinary practice for people with MS. The process narrowed OM selection to a manageable number to compare with clinician- or practice-identified criteria. From these OMs, clinicians could then choose a discrete set of the most appropriate OMs to meet their situation. The process described could be applied by clinicians in any practice setting working with people with MS at any disability level.
Many benefits accrue for those using the MSTF's recommendations in clinical practice. The recommendations have broad applicability across the disability spectrum of MS and in any health-care setting. The recommendations allow efficient identification of OMs pertinent to constructs important to people with MS, and the summaries of psychometric data on the EDGE documents facilitate sound OM selection. For example, reported responsiveness and normative data provided a basis for measuring change and making comparisons, respectively, for an individual with MS. In addition, the usefulness of OMs for particular settings and ability levels for people with MS has been recorded, enabling clinicians to efficiently identify OMs that might have particular relevance. References for evidence on the OMs are reported, along with instructions for administration and information on other available resources (eg, Web-based links). The recommendations can facilitate assessment of clinician and programmatic effectiveness, which could, in turn, be used for marketing and public relations efforts.
There are several limitations to the MSTF recommendations. First, the recommendations did not result directly from a systematic review or meta-analysis of the literature. They were developed through a consensus process based on a review of the literature by a single individual and evaluation of the reported characteristics by a secondary reviewer and then the whole task force. Time constraints limited the number of OMs reviewed. The MSTF aimed to review a broad group of OMs, representing all major constructs relevant to physical therapy for people with MS. Some OMs relevant to this population (eg, the Fatigue Severity Scale) were not included in the MSTF review. Limited availability of published evidence for many OMs across the MS disability spectrum led to a rating of “unable to recommend at this time” for many of the reviewed OMs. Others had good reliability and validity data but lacked responsiveness values, leading to a rating of “recommend” rather than “highly recommend.” Completion of the EDGE forms relied on the literature available at the time of the reviews, generally the summer of 2011. Last, it is unknown whether use of the recommendations will assist in standardizing the selection of OMs and whether they will assist clinicians with making better clinical decisions when developing a plan of care.
The recommendations of the MSTF provide important information to assist with clinical decision making; however, more work is needed. The MSTF acknowledges the need for additional research to document the usefulness of the measures in less-studied populations of people with MS and the need to update and complete the information in the MSTF documents. Also, the MSTF did not attempt to identify core sets (ie, specific OMs to be used for all patients receiving services in a given practice setting or at a given MS-related disability level). The MSTF contends that the development of core sets could be a next step to improve the consistency and quality of care. The EDGE documents and recommendations could provide a foundation to inform the development of core sets.
In summary, the recommendations provided by the MSTF provide guidance for patient- and program-level evaluation. The cases described herein illustrate how the recommendations can be used in selecting OMs. Given practice and patient circumstances, alternative OMs might be helpful in particular situations. The MSTF does not endorse any particular OM as serving all the needs of patients or clinicians. The MSTF does propose that clinicians use a thoughtful process, such as the one described herein, when they seek the appropriate OMs to enhance patient care.
PracticePoints
Rehabilitation clinicians underuse standardized outcome measures when working with people with MS.
Using patient- and practice-specific outcome measures can help clinicians and practices better measure patient status and progress.
The report and recommendations of the American Physical Therapy Association's Multiple Sclerosis Outcome Measures Task Force can be used as a resource to assist rehabilitation clinicians in selecting useful outcome measures for their patients and their practice.
References
Jette DU, Halbert J, Iverson C, Miceli E, Shah P. Use of standardized outcome measures in physical therapist practice: perceptions and applications. Phys Ther. 2009; 89: 125–135.
Huijbregts M, Myers A, Kay T, Gavin T. Systematic outcome measurement in clinical practice: challenges experienced by physiotherapists. Physiother Can. 2002; Winter: 25–36.
Wedge FM, Braswell-Christy J, Brown CJ, Foley KT, Graham C, Shaw S. Factors influencing the use of outcome measures in physical therapy practice. Physiother Theory Pract. 2012; 28: 119–133.
Freeman J, Morris M, Davidson M, Dodd K. Outcome measures to quantify the effects of physical therapy for people with multiple sclerosis. J Neurol Phys Ther. 2002; 26: 139–144.
Hutchinson B, Forwell SJ, Bennett S, Brown T, Karpatkin H, Miller D. Toward a consensus on rehabilitation outcomes in MS: gait and fatigue: report of a CMSC Consensus Conference, November 28–29, 2007. Int J MS Care. 2009; 11: 67–78.
Pearson O, Busse M, Van Deursen R, Wiles C. Quantification of walking mobility in neurological disorders. QJM. 2004; 97: 463–475.
Potter K, Fulk GD, Salem Y, Sullivan J. Outcome measures in neurological physical therapy practice, part I: making sound decisions. J Neurol Phys Ther. 2011; 35: 57–64.
Provance PC. Physical therapy in multiple sclerosis rehabilitation. http://www.nationalmssociety.org/NationalMSSociety/media/MSNationalFiles/Brochures/Clinical-Bulletin-Physical-Therapy.pdf. Accessed August 1, 2014.
Rudick R, Antel J, Confavreux C, et al. Recommendations from the National Multiple Sclerosis Society clinical outcomes assessment task force. Ann Neurol. 1997; 42: 379–382.
National Multiple Sclerosis Society. Clinical Study Measures. http://www.nationalmssociety.org/For-Professionals/Researchers/Resources-for-Researchers/Clinical-Study-Measures. Accessed June 9, 2015.
Potter K, Cohen ET, Allen DD, et al. Outcome measures for individuals with multiple sclerosis: recommendations from the American Physical Therapy Association Neurology Section Task Force. Phys Ther. 2014; 94: 593–608.
World Health Organization. Towards a common language for functioning, disability and health: ICF. http://www.who.int/classifications/icf/training/icfbeginnersguide.pdf. Accessed August 1, 2014.
Potter K, Allen D, Bennett S, et al. Report and recommendations of the APTA Neurology Section Multiple Sclerosis Outcome Measures Taskforce. http://neuropt.org/docs/ms-edge-documents/final-ms-edge-document.pdf?sfvrsn=4. Accessed August 1, 2014.
Kurtzke JF. Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS). Neurology. 1983; 33: 1444–1452.
Goodkin D, Hertsgaard D, Seminary J. Upper extremity function in multiple sclerosis: improving assessment sensitivity with box-and-block and nine-hole peg tests. Arch Phys Med Rehabil. 1988; 69: 850–854.
Mathiowetz V, Volland G, Kashman N, Weber K. Adult norms for the Box and Block Test of manual dexterity. Am J Occup Ther. 1985; 39: 386–391.
Penner I, Raselli C, Stöcklin M, Opwis K, Kappos L, Calabrese P. The Fatigue Scale for Motor and Cognitive Functions (FSMC): validation of a new instrument to assess multiple sclerosis-related fatigue. Mult Scler. 2009; 15: 1509–1517.
Fisk JD, Ritvo PG, Ross L, Haase DA, Marrie TJ, Schlech WF. Measuring the functional impact of fatigue: initial validation of the Fatigue Impact Scale. Clin Infect Dis. 1994;18(suppl 1):S79–S83.
Newsome SD, Wang JI, Kang JY, Calabresi PA, Zackowski KM. Quantitative measures detect sensory and motor impairments in multiple sclerosis. J Neurol Sci. 2011; 305: 103–111.
Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991; 39: 142–148.
Hobart J, Riazi A, Lamping D, Fitzpatrick R, Thompson A. Measuring the impact of MS on walking ability: the 12-Item MS Walking Scale (MSWS-12). Neurology. 2003; 60: 31–36.
Khan F, Pallant JF, Turner-Stokes L. Use of goal attainment scaling in inpatient rehabilitation for persons with multiple sclerosis. Arch Phys Med Rehabil. 2008; 89: 652–659.
Cella D, Dineen K, Arnason B, et al. Validation of the functional assessment of multiple sclerosis quality of life instrument. Neurology. 1996; 47: 129–139.
Hobart J, Lamping D, Fitzpatrick R, Riazi A, Thompson A. The Multiple Sclerosis Impact Scale (MSIS-29): a new patient-based outcome measure. Brain. 2001; 124: 962–973.
Vickrey B, Hays RD, Harooni R, Myers LW, Ellison GW. A health-related quality of life measure for multiple sclerosis. Qual Life Res. 1995; 4: 187–206.
Fischer J, Rudick R, Cutter G, Reingold S. The Multiple Sclerosis Functional Composite measure (MSFC): an integrated approach to MS clinical outcome assessment. Mult Scler. 1999; 5: 244–250.
Savci S, Inal-Ince D, Arikan H, et al. Six-minute walk distance as a measure of functional exercise capacity in multiple sclerosis. Disabil Rehabil. 2005; 27: 1365–1371.
Financial Disclosures: The authors have no conflicts of interest to disclose.







