Practice Points
- To expand the fall anamnesis to better understand the complexity of fall situations and fall risk factors, we recommend mapping the interaction between triggering and circumstantial factors, the impact of preceding factors, and fluctuating symptoms.
- Fall risk evaluation and management should be viewed as personalized rehabilitation, and rehabilitation should be customized to each person using a holistic approach.
- Consider how to strengthen patients’ self-awareness and self-management of fall risk by identifying different risk situations in relation to the current individual’s state to enable self-assessment of fall risk and individual strategies to avoid falling.
Multiple sclerosis (MS) affects approximately 2.8 million people worldwide.1 Onset is commonly between 20 and 30 years,1 with a considerably higher proportion of women being diagnosed compared with men.2 Although the incidence of MS is increasing, the disease course has become milder; contributing causes include disease-modifying therapies and increased attention to lifestyle habits and exposure to risk factors.3 People with MS report a higher fall incidence than the general population.4 Globally, the prevalence of falls for older people is 26.5% (95% CI, 23.4%-29.8%).5 A meta-analysis reported that 56% of people with mild to moderate MS reported falls during a 3-month period; 37% of them reported multiple falls.6 A higher proportion (85%) of a sample of people with MS who used walking aids reported multiple falls in an 8-month fall history.7 Fall risk seems to peak at Expanded Disability Status Scale (EDSS) scores of 4 and 6.6 Monitoring fall risk factors and reporting fall history in medical records are important; however, underreporting may be present.8
Predicting, understanding, and intervening to minimize the risk of falling are of particular interest. Evaluation of multifactorial fall risk factors and interventions to reduce falls require specialized teams. A multiprofessional approach is advantageous, with each profession sharing information within their specific competence. Self-management is important in reducing fall risk, and each patient’s personal resources and circumstances should be considered. Self-management in patients with chronic diseases must be encouraged. Initiatives such as designing fall risk apps for people with MS may contribute to self-management.9
Although balance impairments become more obvious with MS deterioration over time, they are also detected in early phases.10,11 Brandstadter et al studied a sample of people with MS with a mean EDSS score of 1 (170 participants with EDSS 0-2; 15 participants with EDSS ≥ 2.5). One year after inclusion, 11% reported having fallen once during 1 month and 5% reported 2 or more falls.12 Conversely, in another sample (EDSS mean score, 3; range, 0-6) not only did 71% of people with MS fall during a 6-month period, but also 41% of people in the control group (mean age, 38.7 years; range, 18-50) reported falling during this period.4 Although healthy patients in the control group mainly fell outdoors (86%), people with MS fell almost as often indoors as outdoors. For both groups, climbing up or down stairs caused falling (more often among people with MS). People with MS reported transfers, including upright mobility or transfers on or off a chair, in 38% of the falls.
Several fall risk factors have been identified,13 including previous fall history, use of prescribed medications,14 dual-tasking, fatigue, reduced muscular endurance, heat sensitivity,15 higher EDSS scores,15,16 self-reported deteriorating MS status,17 reduced fall self-efficacy,18 and variation in body functioning and capacity within and between days.7,19 Other challenging factors are environmental, such as slippery or uneven surfaces, slopes, crowded places, and having or not having an assistive device,7,15,20,21 or are personal factors such as reduced balance confidence.22 Fall risk factors have been identified that relate to all components defined in the International Classification of Functioning, Disability and Health (ICF).23
Given that fall risk factors have been well established for people with MS, exploring and describing the complexity of fall situations and the factors associated with falls, including intrinsic (eg, symptoms due to MS and their fluctuating impact) and extrinsic factors (eg, surroundings and assistive technology devices), are indicated. Fall situations are likely to differ somewhat between those who use and do not use walking aids. The literature to date focuses mainly on samples of participants with more limited walking capacity. Gaining more knowledge of the complexity of fall risk situations in people with MS who do not yet use walking aids may allow intervention at an earlier stage. Increased understanding of the complexity of fall situations may reveal information that leads to improved fall risk–reducing strategies. In the present study, we aim to explore and describe in a structured way both contributing factors to falls and the complexity of fall situations shortly after they happen in people with MS who do not report use of walking aids.
Methods
Research Team and Reflexivity
All researchers (A.H.W., A.S.F., Y.E.N.) have long experience as registered physiotherapists with specialist qualifications in the field of neurology, with a special focus on people with MS, balance, and falls. They had no relationships with the participants before the study.
Study Design
A cohort longitudinal study with individual telephone interviews was performed using a manifest deductive content analysis24 with the ICF framework.23 The study followed the World Medical Association Declaration of Helsinki and was approved by the Regional Ethics Committee in Uppsala-Örebro (2019-03398). Participants were recruited at 8 primary health care centers and hospitals in central Sweden by physiotherapists in their respective departments.
Participants and Procedures
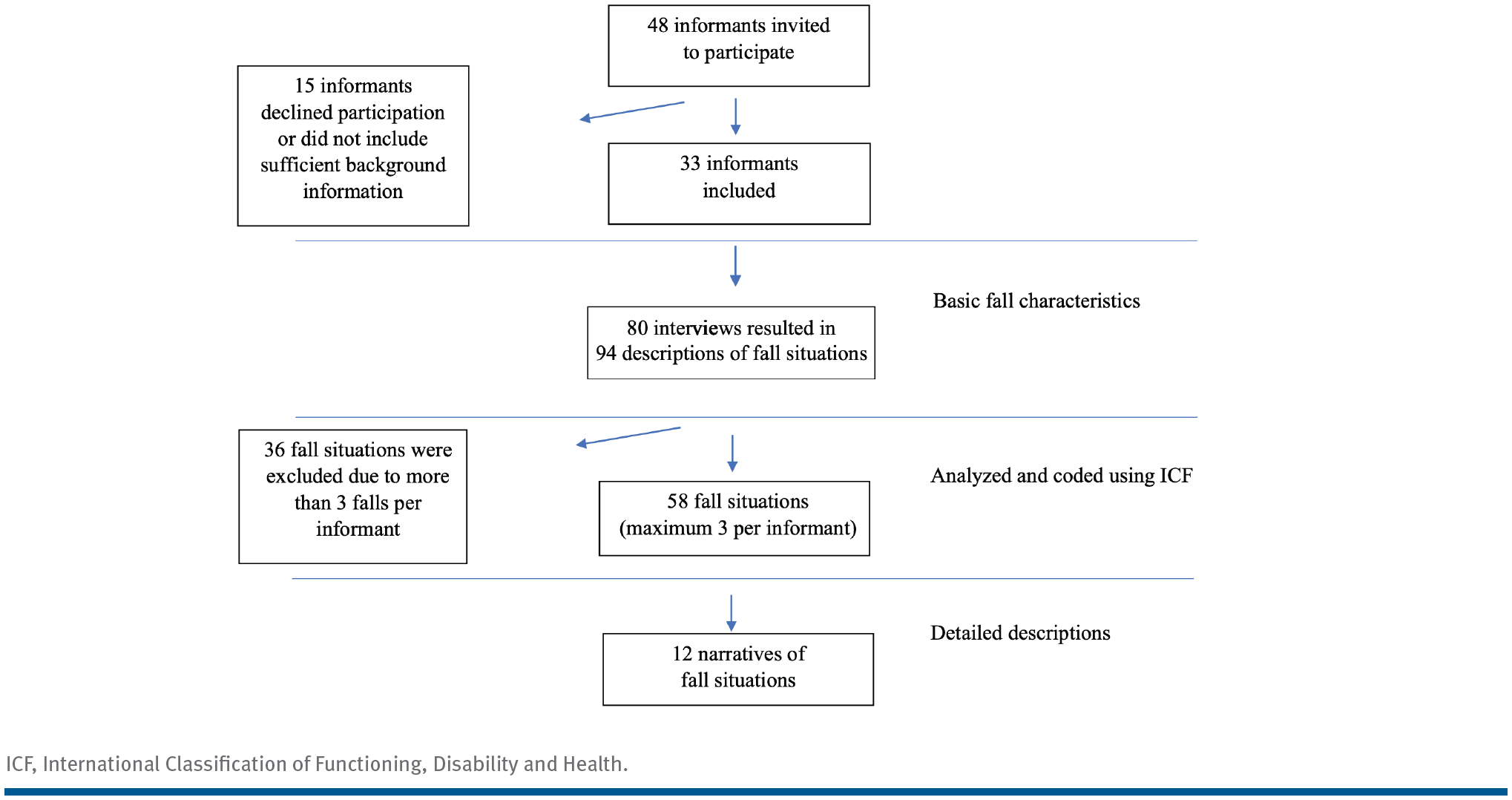
We used a convenience sampling strategy with the following inclusion criteria: MS diagnosis, 18 years or older, report of at least 1 fall in the past year, and no walking aid use. We aimed to include approximately 100 fall situations during the study period (October 2019 to November 2021). Due to the COVID-19 pandemic, the recruitment process was interrupted in March 2020 because outpatient visits to physiotherapeutic facilities were no longer allowed. Of the 48 patients invited to the study, 33 agreed to participate and provided background data and written consent.
Physiotherapists at each site were responsible for recruitment. Patients were given written information about the study, followed by a phone call from the first author (A.H.W.), during which they could find out more about the study. The participants were instructed to contact A.H.W. by text message or phone for an interview as soon as possible after experiencing a fall. A fall was defined in line with the Prevention of Falls Network Europe guidelines as “an unexpected event in which the participants come to rest on the ground, floor, or lower level.”25 A telephone interview was scheduled shortly after contact. The informants were asked to report all falls they experienced during the study period. Text message reminders were sent monthly.
Data Collection
The main outcome measure was a detailed description of a variety of fall incidents together with disease burden, activities-specific balance confidence, age, sex, and working status. The patient-administered EDSS was used to measure disease burden,26 with each patient’s score determined by an experienced neurologist who interpreted the filled-in questionnaires. The patient-administered EDSS score is known to correlate well with the neurologist-administered score.25 The Activities-Specific Balance Confidence (ABC) scale measures confidence in maintaining balance during 16 different tasks.22,27 It has shown good concurrent and convergent validity as well as good ecological validity, discriminating well between those who do and do not use walking aids.21
Each interview started with a standardized opening question: “Can you tell me what happened the last time you fell?” This was followed by questions to capture details of how and when the fall occurred, preceding events and circumstances, and potential consequences of the falls. At the end of each interview, the informants were encouraged to provide the interviewer with any additional information regarding the fall situation that had not already been covered. Each interview lasted 4 to 27 minutes (mean, 9 minutes and 14 seconds) and was recorded via audio and transcribed verbatim. The interview guide was pilot tested on a patient not included in the study to verify that the questions were understandable and relevant to the study aim.
Analysis
Demographic data, ABC scale scores, and EDSS scores were analyzed using descriptive statistics. A manifest deductive content analysis24 was then conducted based on the ICF framework23 following the steps below:
Transcriptions were compared with recordings to correct any errors or ambiguities and were then read several times in their entirety.
A maximum of 3 falls per informant were selected by AHW with the intent to achieve variation in the described fall situations, resulting in 58 fall situations.
To elucidate the complexity of fall situations, the authors chose 12 fall situations to describe in more detail.
The preparation phase started with choosing units of analysis that were related to the research questions. Microsoft Excel was used to manage data.
To get a sense of the whole, the following questions were asked regarding the transcripts: Where did they fall? When did it happen? What was happening? Why did it happen? What were the consequences?
Influencing factors were coded using the ICF structure as a matrix. Factors were divided into direct factors involved in the specific situation and indirect circumstances that made the informants more vulnerable to falling (eg, preceding activities, mood, or climate). Codes that did not fit the matrix were included if considered relevant to the research question.
All authors played an active part throughout the analytical process. Consensus was reached by discussion and by moving back and forth between the ICF framework and the transcriptions. The COREQ (COnsolidated criteria for REporting Qualitative) research checklist was used to conduct and report this study.
Results
Population Characteristics
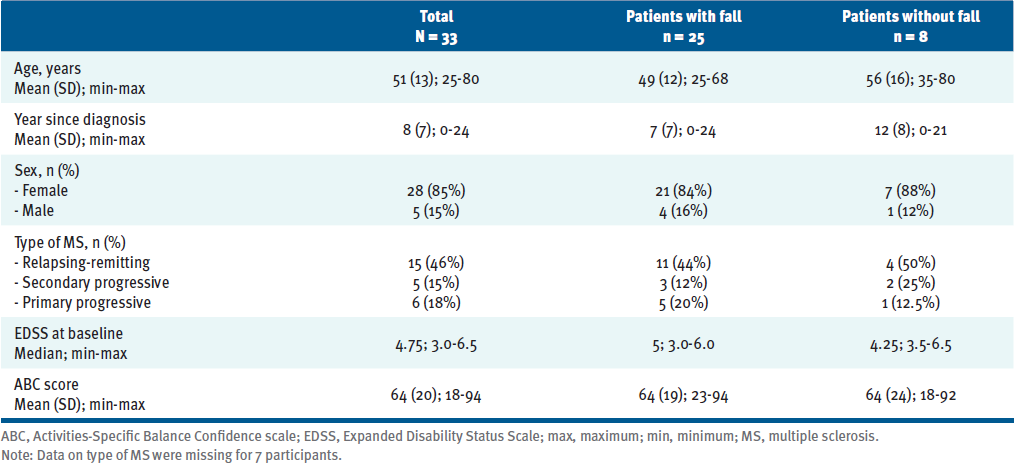
The final sample comprised 28 women and 5 men (mean age [SD], 51 years [13]; mean time since diagnosis [SD], 8 years [7]), with the majority reporting relapsing-remitting MS (Table). Informants not reporting falls during the study period were somewhat older but had a lower EDSS score. For some people, study participation implied that they needed a walking device. Consequently, 5 informants reported that they began using a walking aid during the study period: cane (n = 2), Nordic poles (n = 1), walker (n = 1), or wheelchair (n = 1). Of these 5 people, 1 had a baseline self-administered EDSS score of 6, 3 had a score of 5.5, and 1 had a score of 4.
The informants reported a total of 94 falls during 80 semistructured telephone interviews conducted from November 2019 to April 2022 (Figure). Informants remained in the study for a mean of 33 months (range, 22-37) from inclusion. Twenty-five (76%) of the 33 informants reported at least 1 fall, and 19 of them (58%) reported multiple falls during the study period. Time to contact AHW after falling varied from the day they fell to 2 days later.
Basic Characteristics of the Falls
Overall, 25 informants reported 94 falls (Figure), 53 of which (56%) occurred outdoors and 41 indoors (44%). Regarding location, 43 falls occurred in their own homes (24 indoors and 19 outdoors), 11 at work, 30 in public places (27 outdoors and 3 indoors), 7 in a forest, and 3 in someone else’s home. More than half of the falls (61%) occurred during the daytime, whereas 24% occurred in the evening, 14% in the morning, and only 1% during the night. Most injuries were considered minor. Three informants sought hospital care (wrist fracture, subluxation of the shoulder, and a wound that needed stitches), and 3 participants sought primary health care (ankle sprain, concussion, and thigh bruise).
ICF Coding
Potential impact factors were coded according to the ICF (Appendix, available as a PDF at the end of the online article). These factors were spread among the 4 components of the ICF. Body functions and structure domains were mental function, sensory function and pain, neuromusculoskeletal and movement-related function, and movement function. Several activities and participation domains were identified; mobility and domestic life were the most common. Both indoor and outdoor environmental factors were identified, as were a range of personal factors. Fluctuation of symptoms or variability of functioning within and between days is not covered by the ICF.
Complexity of Fall Situations
All 12 author-selected fall situations involved the interaction of multiple triggering and circumstantial factors. The complexity of each fall situation is described in greater detail in Table S1 (available as a PDF at the end of the online article) together with the informant’s age, sex, working status, ICF codes, ABC score, EDSS score, and a description of the fall’s consequences. Excerpts from the informants’ narratives are used to exemplify the fall situations, and both intrinsic (“I have nothing to stabilize me”) and extrinsic factors (“There were a lot of toys and stuff like that on the ground”) are reported.
The informants reported falls indoors, outdoors, at work, at home, when away, and when performing household chores, transfers, and walking. The activities described when falling were common everyday activities that are unavoidable in daily living (“I was about to go and put the rubbish out,” “I was doing stuff at home, dusting,” “I was riding the bike to the shop”) and when participating in society (“Well, it was at work, which is where I most commonly fall,” “We were visiting friends, and then I stepped on a stone and fell backwards”). Typical MS symptoms such as muscle weakness (“I don’t have any strength in my left side,” “That’s what usually happens, that I don’t have the strength in that leg or my knees give away”), impaired proprioception (“I don’t really know if I’m lifting my leg high enough”), and attention deficits (“A typical thing every time I’m about to fall is that I’m having to keep my attention on something I’m carrying”) in combination made the individuals prone to falling.
Fall situations were also affected by indirect factors when previous activities were described as causing falls later that day: “I came home from my exercise,” “I’d been walking a lot, so my legs were a bit tired,” and “I was physically exhausted after having walked uphill.” Feelings of loss of energy seemed to make participants especially vulnerable to fall risk: “I was so tired that evening, my energy was running out” and “I’m generally worn out and tired at present because my parents are old and I mind them a lot.”
The informants mentioned the difficulty of foreseeing their capacity due to previous activities and fluctuating MS symptoms in general: “I learned something, if you can say that. I won’t overestimate my capacity again. I’ve noticed after this incident that I’m really affected by heat.” Living with a disease that is not only progressive but also potentially variable over time challenged their coping strategies: “But I don’t perceive my balance as really good right now. I think it changes a lot. It gets like that; it differs from day to day.” In addition, some described taking chances as a personality trait or just a way to get things done: “It’s when I do things that I’m not able to do, [because] I test my limits there because I enjoy it so much.”
The following theme was formulated after analyzing the narratives: The complexity of falls in MS includes the interaction of all ICF components and the consideration of preceding factors and fluctuating symptoms.
Discussion
The present study adds to the literature by describing the complexity of fall situations with both direct and indirect influences and circumstantial factors. The narratives from study participants made it obvious how small the margin for maintaining balance can be. Previous activities, stress, or having a cold were enough for some to exceed this margin and fall. We have shown that exploring risk factors at the point of falling is insufficient because preceding activities may play an important role. This finding is important because it may affect how clinicians talk to their patients about fall history and adjust interventions to minimize fall risk.
The ICF framework offers a structured and standardized language to describe functioning and disability in relation to health. It is our understanding that when designing individual interventions, it is helpful to distinguish between different types of factors: body functions, activities and participation, environmental factors, and personal factors.
A delayed response to postural perturbations due to a sudden change of external circumstances, previously described by Cameron et al,28 appeared in several of the narratives. We also verified previously reported fall risk factors,13,15,29 including both physical and cognitive factors. Spasticity was likely to have had an impact in some incidents, described as stumbling or as not lifting the foot high enough. The severity of fall consequences varied substantially among our informants, with fracture being the most severe. Fractures have been reported previously but are uncommon.29,30
In contrast with findings from previous studies,6,30 most of our informants reported falls occurring outdoors. This may be partially because the informants in our sample did not use walking aids at inclusion and likely had less MS-related impairment of their walking ability. The present findings indicate that attention to the inner environment can make a difference. Environment can be adjusted to a certain degree, such as removing obvious risk-inducing objects such as carpets or thresholds at one’s home. Working tasks and environment can also be adjusted to some extent, although the informants’ descriptions of their fall situations underlined the difficulty of achieving full adjustments. Although it is possible to take measures to increase accessibility in the public environment, outdoor life is more challenging. Taking careful note of the ground, adjusting speed, and asking for help were described as facilitating factors for maintaining balance, although these competed with the desire for independence. The informants used a wide range of coping strategies in line with those previously reported,15 and the abandonment of these strategies was one cause of falls. Given that fluctuating symptoms will produce variation in individual capacity both within and between days, we recommend proactive adjustments with reasonable margins.
The falls reported occurred during everyday activities, and taking part in society is vital. Fall situations can occur for all people, and avoiding falls completely is not realistic. Consequently, individuals should not reduce activities and participation but instead adjust to reduce fall risk.
Health care staff should help each patient become an expert on their own personal fall risk–triggering factors and how specific situations and preceding events may lead to falls. Finding patterns in preceding causes can raise individual awareness and help them pay particular attention after physical efforts or other conditions that may increase fall risk. Our findings suggest that clinicians should focus on personal factors by addressing negative feelings, low self-confidence in performing activities or trusting one’s body, and the risks and benefits of pushing one’s limits.
The modus of data collection has been tried before7 and allowed repeated contact with the informants shortly after falling to gain a deeper understanding of falls with reduced risk of recall bias. Time to contact was, in general, within a day or 2 days of the fall. Using a semistructured interview guide helped to keep the focus on the research question and check that all areas were covered. The findings were well matched with the ICF structure, which strengthens the credibility despite some previously known limitations, such as not coding changes in function over time. We endeavored to increase the credibility of the results with thorough discussions of all steps of the analytical process between the authors. To describe the complexity in a trustworthy way, we chose to provide detailed and authentic descriptions of a variety of fall events. We described the informants’ levels of disability using their self-administered EDSS and ABC scores to help clinicians interpret and translate the complex fall situations described here for similar patients. The transferability of the results to all people with MS may be somewhat limited due to the inclusion criterion of not using any walking aid. However, using a variety of fall situations should increase the transferability, including to different countries and contexts. We did not expect to include people with EDSS scores greater than 5; however, 5 people began using walking aids during the study period and 4 had an EDSS score greater than or equal to 5.5. A clinical examination at inclusion might have led to their exclusion.
Eight informants did not report any falls despite regular reminders. One limitation of this study is that we did not follow up to verify whether they fell or not (that is, to find out whether there was a reporting bias). The COVID-19 pandemic heavily affected the inclusion of informants. For a long period, people with MS were not allowed to visit the physiotherapeutic facilities where the inclusion process started. The sample could have been larger without this restriction. However, the narratives show a broad spectrum of fall situations. A weakness is that cognitive function was not assessed apart from using the patient-administered EDSS.26
Conclusions
The combination of a progressive disease and fluctuating symptoms is a challenge for many people with MS. The complexity of fall situations must be recognized and fall prevention should be personalized and tailored to match the individual. Identification of personal fall risk–triggering factors and self-management is crucial because falls occur during everyday activities. Clinicians should consider and discuss preceding and circumstantial factors for falls with their patients.